Abstract
Background
In the present article, we present our first experiences with a new type of balloon-expandable Myval valve (Meril Life Sciences, Gujarat, India).
Materials and methods
A total of 25 consecutive patients who underwent transcatheter aortic valve implantation (TAVI) from June 2020 to November 2020 were included in the study.
Results
The mean age of the study population was 83 (75–87) years; 17 (68%) were female, and 20 (80%) had hypertension. The Society of Thoracic Surgeons (STS) score of the group was 5.4% ± 3.5%. TAVI was performed via the transfemoral route on all patients. In 19 (76%) cases, we started the procedure without predilation. In two (10.5%) cases performed without predilation, the prosthesis did not pass the native valve. We had to implant the valve from the descending aorta in one (4%) patient. We used Prostar XL (Abbott Vascular, Santa Clara, CA, USA) for six (24%) patients and ProGlide (Abbott Vascular) for 19 (76%) patients for vascular closure. Two (8%) in-hospital deaths occurred in our study but there were no deaths in the 30-day and 90-day follow-up. Vascular complications were observed in one (4%) patient. None of the patients in our study had severe paravalvular leak (PVL), while two (8%) patients had moderate PVL. A permanent pacemaker (PPM) was required in two (8%) patients for the indication of complete atrioventricular block. The mean hospital stay for the whole group was 4 (3–7) days.
Conclusion
Based on our experiences, the new balloon-expandable valve Myval is easy to use, efficient, and has only a few negligible drawbacks such as the need for predilation of the sheath. While shaft flexibility may have advantages in some situations including in very tortuous arteries, it may cause some difficulties in alignment of the valves.
Zusammenfassung
Hintergrund
Im vorliegenden Beitrag werden erste Erfahrungen mit einem neuen Typ ballonexpandierbarer Myval-Klappen (Fa. Meril Life Sciences, Vapi, Gujarat, Indien) beschrieben.
Material und Methode
Von Juni bis November 2020 wurden 25 aufeinanderfolgende Patienten in die Studie einbezogen, bei denen eine Transkatheter-Aortenklappenimplantation erfolgte.
Ergebnisse
Das Durchschnittsalter der Studienpopulation betrug 83 (75–87) Jahre; davon 17 (68 %) Frauen, bei 20 Personen (80 %) bestand eine Hypertonie. Der Score gemäß Society of Thoracic Surgeons (STS) betrug für die Gruppe 5,4 % ± 3,5 %. Die Transkatheter-Aortenklappenimplantation erfolgte bei allen Patienten über einen transfemoralen Zugang. In 19 Fällen (76 %) wurde die Operation ohne Prädilatation begonnen. In 2 Fällen (10,5 %) ohne Prädilatation konnte die Prothese die natürliche Klappe nicht passieren. Daher musste die Klappe bei einem Patienten (4 %) von der Aorta descendens aus implantiert werden. Bei 6 Patienten wurde (24 %) Prostar XL (Fa. Abbott Vascular, Santa Clara, CA, USA) und bei 19 Patienten (76 %) ProGlide (Fa. Abbott Vascular) zum Gefäßverschluss verwendet. In dieser Studie kam es noch im Krankenhaus zu 2 Todesfällen (8 %), es traten jedoch keine Todesfälle während des 30-Tage- und während des 90-Tage-Follow-up auf. Gefäßkomplikationen gab es bei einem Patienten (4 %). Keiner der Patienten in dieser Studie wies ein schweres paravalvuläres Leck (PVL) auf, bei 2 Patienten (8 %) lag ein mittelgradiges PVL vor. Einen permanenten Schrittmacher benötigten 2 Patienten (8 %) für die Indikation eines kompletten atrioventrikulären Blocks. Die mittlere Krankenhausverweildauer in der Gesamtgruppe betrug 4 (3–7) Tage.
Schlussfolgerung
Den Erfahrungen der Autoren zufolge ist die neue ballonexpandierbare Klappe Myval einfach zu verwenden, wirksam und hat nur wenige, vernachlässigbare Nachteile wie die Notwendigkeit der Prädilatation der Hülle. Zwar mag die Flexibilität des Schafts Vorteile in einigen Situationen, einschließlich stark geschlängelter Arterien, haben, doch kann dies auch Schwierigkeiten in der Ausrichtung der Klappen mit sich bringen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Transcatheter aortic valve implantation (TAVI), first applied on inoperable patients with severe aortic valve stenosis (AS; [1]), has become a treatment option for patients with even low surgical risk according to the latest American College of Cardiology (ACC)/American Heart Association (AHA) guideline [2]. Device selection for TAVI is based on the experience of the operator, the hospital’s systems, and the most suitable option for the patient. Until recently, however, the only balloon-expandable system option was SAPIEN 3 (Edward Lifesciences, Inc., Irvine, CA, USA), in many cases superior to those with surgical valve replacement and better clinical outcomes than self-expanding valves in unselected patients [3].
The Myval transcatheter heart valve (THV; Meril Life Sciences, Gujarat, India) is a balloon-expandable valve that obtained the European Community (CE) mark following the Myval-1 study [4]. In this study of 30 patients with AS in the medium–high-risk group, all procedures were successful without paravalvular leakage (PVL) or the need for a permanent pacemaker (PPM) after the procedure. These data are similar to the percutaneous arm of the PARTNER‑3 trial, but more data are needed.
In our institute, we have been performing TAVI procedures since 2011 and only used balloon-expandable valves (Edward Lifesciences, USA). In this article, we present our first experiences with of a new type of balloon-expandable valve (Myval).
Method
Patient population
Overall, 25 consecutive patients who underwent transfemoral TAVI from June 2020 to November 2020 were included in the study. Patient eligibility for TAVI was confirmed by a multidisciplinary cardiac team that included at least two interventional cardiologists, two cardiothoracic surgeons, and an anesthesiologist. Basic clinical features, procedural data, laboratory data, echocardiographic data, and outcome data were collected retrospectively. Surgical risk was calculated according to standard STS and Logistic EuroSCORE risk estimation tools. The STS scores of 4%, 4–8%, and > 8% were classified as low, medium, and high risk, respectively [5]. This study was granted the approval of the local ethics committee.
Echocardiographic assessment
Transthoracic echocardiograms of the population were obtained at baseline, before discharge, and 3 months after the procedure, according to the American Society of Echocardiography guidelines [6]. Severe AS was defined using echocardiography as an aortic valve area (AVA) of < 0.8 cm2 and/or a mean pressure gradient of 40 mm Hg or peak aortic velocity ≥ 4 m/s. The AVA was calculated using the continuity equation as the stroke volume measured in the left ventricular outflow tract (LVOT) divided by the aortic velocity–time integral.
Procedure
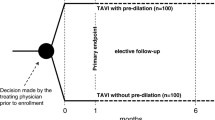
All TAVI procedures were performed using Myval THV. For all patients, both the vascular access and the aortic valve were evaluated with multislice computed tomographic angiography of the entire aorta using vascular window settings before the procedure. Transfemoral access was the first choice whenever possible. All TAVI procedures were performed by six independent healthcare teams in the same catheter laboratory. All procedures were performed with patients under conscious sedation using a traditional minimalist approach without transesophageal echocardiography. During the procedure, intravenous heparin was administered so that the activated coagulation time was > 250 s. Activated clotting time was measured every 30 min. Hemostasis was achieved using percutaneous closure devices Prostar XL or Perclose ProGlide 6‑Fr suture devices. After the sheath was removed, peripheral angiography was performed to evaluate the access site patency. Following a successful TAVI procedure, patients were given dual antiplatelet therapy consisting of 75 mg clopidogrel and 100 mg aspirin for 3–6 months. Considering the risk of bleeding in patients with atrial fibrillation (AF), personalized anticoagulant and antiplatelet therapy was administered.
Follow-up
In-hospital death, 30-day and 3‑month all-cause mortality, stroke, bleeding complications, vascular complications, acute kidney injury, device success, and side effects were defined according to the consensus document of the Valve Academic Research Consortium‑2 (VARC‑2; [7]). Death was confirmed through hospital records and family contacts. Details of pacemaker implantation and PVL after TAVI were also collected retrospectively at the index hospital admission. The patients underwent echocardiographic evaluation before the procedures, before discharge, and months after discharge.
Device evaluation of Myval THV system
Myval, a newer-generation balloon-expandable THV system, is designed on a nickel-cobalt alloy (MP35N) frame—which enables optimal radial strength and radiopacity—and decellularized bovine pericardium tissue, crafted into a tri-leaflet valve. The valve consists of a novel hybrid honey-comb scaffold design. The upper part of the frame is composed of a single row of tall, large, and open-cell configuration to ensure unjailing of the coronary ostia that preserves coronary flow; the lower part of the frame is composed of two short rows of tightly packed, close-cell hexagonal configuration providing high radial strength required at the annular base. This unique pattern of Myval helps the operator in planning the precise placement of the valve and ensures its orthotopic deployment. The lower closed cells of Myval THV are covered externally with a sealing cuff, made of polyethylene terephthalate, to form an external buffing that minimizes or eliminates PVL (Fig. 1). The THVs were available in different sizes: conventional (20, 23, 26, and 29 mm), medium (21.5, 24.5, and 27.5 mm) and extra-large (30.5 and 32 mm; extra-large sizes). All Myval sizes are compatible with 14-Fr expandable sheaths. Myval is mounted over the balloon outside the patient. The Navigator balloon-expandable THV delivery system has a unique design featuring a proximal deep flexion handle and a distal balloon with two counter-opposing soft stoppers within that create a superficial low-profile crimping zone and thus a comfortable fit that prevents any unwary movement of the Myval THV during crossover through the sheath or thereafter (Fig. 2). The delivery system allows for flexion of the distal catheter system that ensures trauma-free negotiation across the aortic arch and minimizes or eliminates risk of a periprocedural stroke during arch navigation.
Statistical analysis
Data were analyzed using SPSS version 22.0 (SPSS Inc. Chicago, IL, USA). All data are presented as mean ± standard deviation (SD) for parametric variables, median (interquartile range) for nonparametric variables, and percentages for categorical variables. Continuous variables were checked for normal distribution assumptions using the Kolmogorov–Smirnov test. Categorical variables are presented as frequencies and percentages and were compared using Pearson, Fisher’s exact, and chi-square tests. One-way repeated measures ANOVA was used for normally distributed continuous variables, and the Friedman test was used for nonparametric variables. Two-tailed p values < 0.05 were considered statistically significant.
Results
The laboratory and clinical characteristics of the patients are shown in Table 1. The mean age of the whole population was 83 years (75–87), 17 (68%) were female, and 20 (80%) were hypertensive. All patients were symptomatic, with 15 (60%) in class III–IV and 10 (40%) in class I–II, according to New York Heart Association (NYHA) functional class. Among the study patients, six (24%) were diabetic, ten (40%) had a known history of coronary artery disease, two (8%) had a known history of carotid stenosis, and six (24%) had a previous history of coronary artery bypass grafting. The mean STS score of the group was 5.4% ± 3.5%. Before the TAVI procedure, 12 (48%) patients had a diagnosis of permanent (AF), four (16%) patients had a previous stroke, and two (4%) patients were receiving renal replacement therapy. Initial echocardiographic parameters were mean AVA 0.608 ± 0.17 cm2, mean aortic valve gradient was 45.8 ± 9 mm Hg, and there were seven cases of (28%) moderate-to-severe mitral regurgitation with severe AS. In addition, five (20%) patients were diagnosed with paradoxical low-flow low-gradient AS according to the previously mentioned criteria.
Procedural outcomes
Procedural details are described in Table 2. The TAVI procedure was performed via the transfemoral route for all patients. We used Prostar XL for six (24%) patients and ProGlide for 19 (76%) patients for vascular closure. Procedural complications and outcomes are described in Table 3. Two (8%) in-hospital deaths occurred in our study but no deaths in 30 days and 90 days. Vascular complications were observed in one (4%) patient. None of the patients in our study had severe PVL, and two (8%) patients had moderate PVL; PPM was required in two (8%) patients, and the indications were complete AV block. We saw the valve moving back inside the sheath in three cases (12%) and there was ectopic valve deployment in one patient (4%). The mean hospital stay in the whole group was 4 days (3–7). Comparison of baseline and post-TAVI echocardiographic parameters of the patients are described in Table 4. It was observed that the improvement in LVEF continued at the 30-day and 90-day follow-up. After TAVI, all echocardiographic parameters improved significantly, and the mean gradient decreased to 9 mm Hg (8–11). In addition, a statistically significant increase in left ventricular ejection fraction (LVEF) was observed.
Discussion
Transcatheter aortic valve implantation evolved into a treatment modality only for patients with severe AS and a moderate or high risk of cardiac-surgical mortality and/or morbidity. However, after the results of recent clinical trials with low-risk patients demonstrating that TAVI is at least as effective as surgery for low-risk patients, the recent ACC/AHA guidelines have recommended TAVI for such patients [2, 3, 8].
Two in-hospital deaths occurred in our study. One patient died during the procedure due to LMCA obstruction despite successful revascularization percutaneously. Another patient died due to acute tubular necrosis on the third postoperative day. No periprocedural death was observed in the Myval 1 study, but two (6.7%) patients died at the 6‑month follow-up. One of the patients died of acute renal failure, while the other died due to sepsis [4].
Compared to early TAVI studies [9], cumulative bleeding and vascular complication rates in TAVI have decreased in more recent reports [10] with the availability of lower-profile delivery systems, but these remain a common complication of TAVI. These complications lead to a worse prognosis and a longer hospital stay. A previous registry indicated that patients treated with Prostar XL with ProGlide at TAVI found higher closure device success rates and lower bleeding complications in the ProGlide cohort [11]. In our study, we used Prostar XL for six patients and ProGlide for 19 patients. No vascular complications were observed in the ProGlide group, but there was procedural failure with one patient in the Prostar XL group. In this patient, bleeding control was achieved after 15 min of occlusion by peripheral balloon.
Previous studies have shown that PVL is associated with a poor prognosis after TAVI [12, 13]. None of the patients in our study had severe PVL, and two patients had moderate PVL. Although the polyethylene terephthalate fabric skirt structure of Myval THV decreased the rate of PVL, our PVL rates were higher than those in other studies [14,15,16]. These findings may be related to the small number of patients in our study.
In our study, the need for PPM implantation was similar to the data in the literature for SAPIEN 3, between 7% and 17% [14]. A PPM was required for two patients, and the indications were complete AV block. We implanted a PPM in both of our patients before leaving the hospital.
The structure of the Myval valve (Fig. 1) is similar to the SAPIEN 3, but with some differences. The THVs were available in different sizes: conventional (20, 23, 26, and 29 mm), medium (21.5, 24.5, and 27.5 mm) and extra-large (30.5 and 32 mm; extra-large sizes) [17]. All Myval sizes are compatible with 14-Fr expandable sheaths, which are smaller than the SAPIEN-XT or SAPIEN‑3 inlet system. Another difference is that Myval is folded before introducing the valve through the sheath, whereas the Edwards valve is folded in the descending thoracic aorta. That would be a disadvantage for Myval, since we saw the valve moving back inside the sheath (Fig. 3a) in three cases with especially limited peripheral artery diameters and using large valve sizes. Thus, we have routinely predilated the sheath with 18‑F dilators that enabled the valves to advance more smoothly.
According to a recently published article, Myval could be retrievable in some cases through the sheath if the valve is not implanted [17]. We had to retrieve the valve in three cases. We successfully retrieved the valve in one case. In other case, while removing the valve, it was completely detached from the balloon and remained in the sheath (Fig. 3b). After retrieving the sheath completely, we were able to remove the valve by cutting the sheath (Fig. 3c), After removing the valve, we implanted the same valve again. In other case, however, while retrieving the valve, the distal part of the sheath that cannot be seen clearly on X‑ray stripped the valve from the balloon (Video 1). The valve was then implanted into the descending aorta. Following this, another valve was implanted successfully.
The delivery shaft of the Myval is relatively smooth compared to the Edwards valve and it may cause some difficulties during the annular alignment of the valve. In our experience, we could easily rotate the delivery shaft of the Edwards valve clockwise and anticlockwise in order to align the valve perpendicularly to the annular line. However, this is not the case for Myval due to the flexibility of the shaft.
We used the Myval successfully in 25 cases. While there is no direct comparison with the Edwards valve, according to previous experiences with Edwards in our hospital, we had similar rates of mortality, PPM need, and PVL with Myval.
Limitations
The limited number of patients is the major limitation of our study. Moreover,, the follow-up was short and thus the long-term efficacy of Myval should be evaluated in studies with longer follow-up.
Conclusion
Based on our experiences, a new type of balloon-expandable valve is easy to use, efficient, and has only a few negligible drawbacks such as the need for predilation of the sheath.. While shaft flexibility may have advantages in some situations including very tortuous arteries, it may cause difficulties in the alignment of the valves. Finally, even if the valve is theoretically retractable, more attention should be paid to the distal part of the expandable sheath that is not easily recognizable on X‑ray images.
References
Cribier A, Eltchaninoff H, Bash A, Borenstein N, Tron C, Bauer F et al (2002) Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation 106(24):3006–3008
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F et al (2021) 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 143(5):e35–e71. https://doi.org/10.1161/CIR.0000000000000932
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M et al (2019) Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med 380(18):1695–1705
Sharma SK, Rao RS, Chandra P, Goel PK, Bharadwaj P, Joseph G et al (2020) First-in-human evaluation of a novel balloon-expandable transcatheter heart valve in patients with severe symptomatic native aortic stenosis: the MyVal-1 study. EuroIntervention 16(5):421–429
Ad N, Holmes SD, Patel J, Pritchard G, Shuman DJ, Halpin L (2016) Comparison of EuroSCORE II, original EuroSCORE, and the Society of Thoracic Surgeons risk score in cardiac surgery patients. Ann Thorac Surg 102(2):573–579
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC et al (2019) Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 32(1):1–64
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH et al (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium‑2 consensus document. Eur Heart J 33(19):2403–2418
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D et al (2019) Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med 380(18):1706–1715
Généreux P, Head SJ, Van Mieghem NM, Kodali S, Kirtane AJ, Xu K et al (2012) Clinical outcomes after transcatheter aortic valve replacement using valve academic research consortium definitions: a weighted meta-analysis of 3,519 patients from 16 studies. J Am Coll Cardiol 59(25):2317–2326
Carroll JD, Vemulapalli S, Dai D, Matsouaka R, Blackstone E, Edwards F et al (2017) Procedural experience for transcatheter aortic valve replacement and relation to outcomes: the STS/ACC TVT registry. J Am Coll Cardiol 70(1):29–41
Berti S, Bedogni F, Giordano A, Petronio AS, Iadanza A, Bartorelli AL et al (2020) Efficacy and safety of ProGlide versus Prostar XL vascular closure devices in transcatheter aortic valve replacement: the RISPEVA registry. J Am Heart Assoc 9(21):e18042
Jilaihawi H (2016) Paravalvular regurgitation after transcatheter aortic valve replacement: striving to perfect its prognostic evaluation with hemodynamic data. JACC Cardiovasc Interv 9(7):712–714
Mack MJ, Leon MB, Smith CR, Miller DC, Moses JW, Tuzcu EM et al (2015) 5‑year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 385(9986):2477–2484
Sawaya FJ, Spaziano M, Lefèvre T, Roy A, Garot P, Hovasse T et al (2016) Comparison between the SAPIEN S3 and the SAPIEN XT transcatheter heart valves: a single-center experience. World J Cardiol 8(12):735–745
Duran Karaduman B, Ayhan H, Keleş T, Bozkurt E (2020) Evaluation of procedural and clinical outcomes of transcatheter aortic valve implantation: a single-center experience. Anatol J Cardiol 23(5):288–296
Pibarot P, Salaun E, Dahou A, Avenatti E, Guzzetti E, Annabi MS et al (2020) Echocardiographic results of transcatheter versus surgical aortic valve replacement in low-risk patients: the PARTNER 3 trial. Circulation 141(19):1527–1537
Sharma SK, Rao RS, Chopra M, Sonawane A, Jose J, Sengottuvelu G (2021) Myval transcatheter heart valve system in the treatment of severe symptomatic aortic stenosis. Future Cardiol 17(1):73–80
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.R. Akyüz, A.H. Konuş, Ö.F. Çırakoğlu, S. Şahin, S. Kul and L. Korkmaz declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Supplementary Information
Video 1. while retrieving the valve, the valve was stripped from the balloon by attaching the sheath to its distal end.
Rights and permissions
About this article
Cite this article
Akyüz, A.R., Konuş, A.H., Çırakoğlu, Ö.F. et al. First experiences with a new balloon-expandable Myval transcatheter aortic valve: a preliminary study. Herz 47, 449–455 (2022). https://doi.org/10.1007/s00059-021-05069-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-021-05069-4
Keywords
- Aortic valve disease
- Percutaneous intervention
- Transcatheter valve implantation
- Complications
- Vascular access