Abstract
Type 2 diabetes mellitus is a global epidemic that due to its increasing prevalence worldwide will likely become the most common debilitating health condition. Even if diabetes is primarily a metabolic disorder, it is now well established that key aspects of the pathogenesis of diabetes are associated with nervous system alterations, including deleterious chronic inflammation of neural tissues, referred here as neuroinflammation, along with different detrimental glial cell responses to stress conditions and neurodegenerative features. Moreover, diabetes resembles accelerated aging, further increasing the risk of developing age-linked neurodegenerative disorders. As such, the most common and disabling diabetic comorbidities, namely diabetic retinopathy, peripheral neuropathy, and cognitive decline, are intimately associated with neurodegeneration. As described in aging and other neurological disorders, glial cell alterations such as microglial, astrocyte, and Müller cell increased reactivity and dysfunctionality, myelin loss and Schwann cell alterations have been broadly described in diabetes in both human and animal models, where they are key contributors to chronic noxious inflammation of neural tissues within the PNS and CNS. In this review, we aim to describe in-depth the common and unique aspects underlying glial cell changes observed across the three main diabetic complications, with the goal of uncovering shared glial cells alterations and common pathological mechanisms that will enable the discovery of potential targets to limit neuroinflammation and prevent neurodegeneration in all three diabetic complications. Diabetes and its complications are already a public health concern due to its rapidly increasing incidence, and thus its health and economic impact. Hence, understanding the key role that glial cells play in the pathogenesis underlying peripheral neuropathy, retinopathy, and cognitive decline in diabetes will provide us with novel therapeutic approaches to tackle diabetic-associated neurodegeneration.
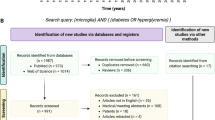
Graphical abstract

Similar content being viewed by others
Background
In an increasingly aging population, the growing prevalence of chronic diseases such as diabetes represents a serious challenge for healthcare systems. Diabetes prevalence is expected to increase to 643 million affected people in 2030, doubling the number of people suffering from diabetes since 2011[1, 2]. This rapid and concerning escalation is predominantly linked to the increased prevalence of type 2 diabetes mellitus (T2D). T2D represents one of the most common metabolic diseases in Western societies and it is considered “the epidemic of the twenty-first century”, affecting 1 in 11 people in Europe [2]. In addition, 318 million adults are estimated to have pre-diabetes or impaired glucose tolerance, representing a population at higher risk of further developing diabetes [2]. Diabetes-associated medical care represents around the 8–12% of the total National Health System expenditures [3,4,5] due to its strong association with several disabling complications, including alterations in the peripheral (PNS) and central nervous system (CNS) such as peripheral neuropathy, and diabetic retinopathy or cognitive decline, respectively [5,6,7,8].
Diabetic retinopathy (DR) is one of the most common diabetic complications and represents one of the leading causes of preventable visual impairment in the working-age population in developed countries, accounting for the 15–17% of all cases of total blindness in Europe and USA [1, 9]. Due to its limiting and debilitating nature, DR severely impacts in the healthcare and social costs of diabetic patients [10]. Current available treatments for DR include laser photocoagulation, intravitreal injections of anti-VEGF agents or corticosteroids. However, all these treatments are invasive and expensive, have a significant number of side effects, and are used exclusively in advanced stages of the disease, when the vascular phenotype becomes evident, and the vision has already been significantly affected. Therefore, new, and more efficient preventive and interventional strategies based on a better understanding of the pathogenesis of the disease are urgently needed.
Diabetic peripheral neuropathy (DPN) is also commonly described as a diabetic complication since 50–66% of diabetic patients will eventually develop DPN during the time course of the disease [11, 12]. DPN is characterized by a progressive distal-to-proximal degeneration of peripheral nerves, which results in sensory symptoms, including spontaneous pain, allodynia (painful sensati5on to innocuous stimuli), hyperalgesia (increased pain perception to noxious stimuli), weakness, and/or paraesthesia and numbness, which vary in nature and severity depending on the specific neuronal subpopulation affected [12]. Although some patients with DPN do not present any symptoms, the vast majority report pain and/or loss of function in distal regions such as in their toes, feet, fingers, or hands. The early onset of DPN is characterized by the hyperexcitability of the sensory nerve fibers, which translates into pain symptoms. Later stages are characterized by a progressive loss of neuronal fibers, and thus significant morbidity and mortality [12]. Similar to neuropathic pain with other etiology, DPN is refractory, partially responsive to existing pharmacotherapy [13] or its adverse effects limit its clinical use.
In addition to DR and DPN, diabetes is strongly associated with cognitive impairment and dementia, with diabetic patients showing reduced performance in multiple cognitive functions. Hence, diabetes and, especially T2D, is often considered an accelerator of cognitive decline (CD) [14]. The tight relationship between diabetes and cognitive impairment and the accumulation of neurological symptoms observed in diabetic patients has driven the growth of epidemiological and clinical studies, including reviews and meta-analysis studies, aiming at establishing a relationship between the two [7, 15]. It has already been established that T2D patients have twofold higher risk of developing Alzheimer’s disease (AD) and vascular dementia, with approximately 30% of T2D diabetic patients over 65 years old showing mild cognitive impairment[16]. Due to this close association and the commonly shared mechanisms between diabetes and Alzheimer’s disease (AD), some researchers have suggested using the terminology “Type -3-Diabetes” for Alzheimer’s disease [17]. CD in diabetic patients is predominantly linked to higher levels of tau and phosphorylated tau in the cerebrospinal fluid, while only 39% of diabetic patients show positivity for Aβ plaques [17, 18]. These features have also been observed in the two most common animal models of type 1 and T2D, Streptozotocin (STZ) and db/db mouse models, respectively [19, 20].
Therefore, diabetes represents a health and economic burden, and thus demands cost-effective and innovative therapeutic strategies to limit its epidemic escalation and the debilitating effects driven by its complications. To do so, determining the underlying mechanisms associated with diabetic complications is of paramount importance.
Despite being primarily a metabolic disorder in which PNS- and CNS-associated complications (such as DR, DPN, and CD-AD) have been linked mainly to microvascular pathology, in the recent years, it has become clear that diabetes significantly impacts both, neuronal and glial cell function in the retina, brain, and the PNS. A growing body of evidence supports the idea that neuronal damage and glial cell alterations are already present in the early stages of DR and DPN, while becoming more dominant in later stages in the CNS [21,22,23]. Hence, it has been widely hypothesized that neuroprotective therapeutic strategies may be effective in preventing and arresting diabetes-associated neurodegeneration [22, 24]. In the case of DR, retinal functional abnormalities are detectable even before microvascular lesions appear, with especial emphasis been placed in the pathophysiology of the neurovascular unit (NVU), which consists of vascular elements (endothelial cells and pericytes), the basement membrane, neurons, and glial cells (Müller cells, astrocytes, and microglia), which dysfunction greatly impacts neuronal function and may initiate both neuronal degeneration and microvascular impairment [22]. In the PNS, a large amount of data supports the essential role of glial cells, namely satellite glial cells (SGCs) and Schwann cells (SCs) as key components of neuronal structure and function maintenance and therefore, of DPN pathogenesis [25]. On the other hand, diabetic CNS alterations in astrocytes, microglia, and myelin have predominantly been described in association with brain atrophy, hyperpermeability of the blood–brain barrier (BBB) and cognitive decline [26, 27].
Thus, in this review, we aim to describe common and cell-type-specific alterations observed in the different glial cell populations (Fig. 1) in diabetes to better understand the mechanisms underlying central and peripheral nervous system diabetic complications such as DR, DPN, and CD-AD.
Central nervous system glia
Astrocytes and Müller cells
Astrocytes are found in the CNS (spinal cord, brain, and retina) and have a key crucial role in neuronal trophic support, neuronal signal transduction, vessel growth, and BBB and blood–retinal barrier (BRB) maintenance [28, 29]. Müller cells, on the other hand, are the main glial cell and the sentinels of the retina, having a pivotal role in both, retinal homeostasis and in pathological conditions, including DR. Müller cell functions include NVU support, releasing trophic factors, neurotransmitter recycling (e.g., glutamate, γ-aminobutyric acid), controlling water and ion (mainly K+) homeostasis, stabilizing microvasculature, regulating retinal innate immunity, and participating in the visual cycle [30]. The role of astrocytes in DR is still uncertain as they show the opposite reaction to Müller cells in hyperglycemia. While Müller cells become gliotic and hypertrophic associated with morphological alterations, the number of astrocytes is significantly decreased already in early DR [31], possibly leading to BRB impairment and vascular leakage. However, although debatable, Müller cells have also been reported to die via caspase-1-mediated pyroptosis in DR[32,33,34] exacerbating neuroprotection loss, BRB impairment, and vascular leakage [30, 34, 35]. Due to astrocyte and Müller glial cell relevance in maintaining the neurovascular structure and proper CNS function, it is believed that their dysfunction in diabetes may be a crucial factor in the pathophysiology of DR and diabetes-associated cognitive impairment, contributing to both microvascular and neurodegenerative lesions [7, 30].
Gliosis and inflammation
Müller cell gliosis has been described as one of the first pathogenic events and a hallmark of DR, being present even in the absence of vascular or clinical symptoms and persisting throughout the disease course. Gliotic Müller cells release a myriad of pro-angiogenic factors, pro-inflammatory, and pro-fibrotic factors that contribute to vascularization and neurodegeneration, and therefore to DR progression [30, 34, 36]. Müller glial cell production of vascular endothelial growth factor (VEGF), the major angiogenic factor, is known to be exacerbated in diabetes, where it contributes to vascular leakage and inflammation prior to neovascularization [36, 37].
In addition, under glycemic conditions, Müller cells also activated caspase-1 pathway, known to be a major source for IL-1β, which in turn, affects endothelial cell viability [38]. Besides IL-1β, Müller cells also produce a plethora of retinal neurovascular inflammation mediators, such as interleukin-6 (IL-6), IL-17, tumor necrosis factor-α (TNF-α), and chemokine ligand-2 (CCL-2), associated with vascular dysfunction and inflammation [39,40,41,42,43]. Moreover, aberrant Müller cell proliferation and release of pro-fibrotic mediators has been reported to play a pivotal role in the formation of fibroproliferative tissue [44], which represents an end stage in patients with proliferative diabetic retinopathy (PDR) and could cause retinal detachment [45]. Hence, Müller cells have been proposed as a source of myofibroblast in the epiretinal space where fibrovascular proliferation occurs [46], although the mechanism controlling Müller cell transdifferentiation in the context of diabetic retinopathy remains largely unknown [45].
In the brain, astrocytic alterations, on the other hand, have been profoundly described in other neurodegenerative diseases associated with diabetes, such as AD, where reactive astrogliosis is associated with amyloid plaques and Tau oligomers [47]. In the context of diabetes, however, the results are contradictory. While persistent astrocyte reactivity, identified by an enhanced glial fibrillary acidic protein (GFAP) expression and increased number of GFAP+ astrocytes, similar to that observed in AD, has been described in models of T1D and T2D in rats [48, 49], other authors reported attenuated GFAP expression in different areas of the brain of rats with T1D [50] or astrocytes exposed to hyperglycemia in vitro [51]. In the spinal cord, strong evidence points toward the relevance of reactive astrocytes in the development of diabetic peripheral neuropathy, mostly studied in animal models of T2D [52,53,54,55].
Crosstalk with neurons
The primary excitatory neurotransmitter responsible for learning, memory, and synaptic plasticity is glutamate, which in the retina also facilitates the transmission of visual signals from photoreceptors, bipolar cells, and ganglion cells. The clearance of glutamate from the extracellular space and its conversion into non-toxic glutamine is carried out by astrocytes in the CNS and Müller cells in the retina [34, 56] . Both, in DR and CD-AD, there are multiple lines of evidence of dysfunctional glutamate recycling leading to an excess of glutamate in the synapses, overstimulation of postsynaptic glutamate receptors, increased intracellular Ca2+ concentrations and subsequently, enhanced neuronal cell death [34, 56].
Glutamate transporter-1 (GLT-1) is the dominant glutamate transporter expressed by astrocytes in the brain and has been found to be significantly reduced or damaged in neurodegenerative diseases related with diabetes such as AD and cognitive impairment [57]. Despite the impairment in glutamate clearance [58], there are discrepancies about astrocyte GLT-1 expression in diabetic brains. While some groups reported no changes in the expression of GLT-1 and GLAST (glutamate/ aspartate transporter) despite an attenuated GFAP reactivity [50], others observed a marked reduction of GLT-1 [48]. Further studies aimed at elucidating alterations in glutamate transporters or recycling in diabetes and diabetes-associated CD are needed.
In the spinal cord, enhanced excitatory glutamatergic signaling has been associated with nociception in the context of diabetes [52, 59, 60]. The development of mechanical allodynia and hyperalgesia associated with T2D is usually linked to a decreased expression of GLT-1 particularly in the dorsal horn, and impaired extracellular glutamate recycling and accumulation [59].
Lastly, in the retina, Müller cells are essential to facilitate the use of glutamate for visual signal transmission by photoreceptors, and to do so, they express both, GLT-1 but mostly GLAST transporters, similarly to astrocytes, together with glutamine synthetase (GS), which in the retina is exclusively expressed in Müller cells [61]. Alterations in glutamate release and subsequent excitation of retinal ganglion cells have been observed already 4 weeks after the development of diabetes, being considered an early-stage diabetic symptom [62]. In experimental models of DR, an accumulation of glutamate occurs in the retina, either due to a significant decrease in glutamate transport via GLAST [62] or a decreased GS activity, necessary for neurotransmitter regeneration [63]. The expression of GLAST in diabetes has been reported to be significantly downregulated, leading to a higher amount of glutamate being transported to photoreceptor, bipolar, and ganglion cells [64]. Consistent with this, several reports showed an enhanced glutamate accumulation in experimental models of DR [65], with potentially toxic levels of glutamate detected in the vitreous humor of diabetic patients [66].
Glymphatic system
Fluid clearance is mediated by osmotic water transport coupled with the transport of osmolytes, mainly potassium, which alterations can also contribute to glutamate excitotoxicity. The main transporters involved in ion and water buffering are aquaporin-4 (AQP4) and inward rectifying K+ channel subtype 4.1 (Kir4.1), both located in Müller and astrocyte endfeet. Inwardly rectifying channels of the Kir family, mainly Kir4.1, play a critical role in spatial buffering of potassium ions that accumulate during neuronal activity, regulating the balance of water and glutamate uptake on astrocytes and Müller cells [67]. Both, Kir4.1 and AQP4, show an altered expression, location, and/or function in diabetic Müller retinal cells and brain and spinal cord astrocytes [55, 67, 68]. Astrocytes in hyperglycemic conditions and T2D mouse models show a significant reduction in the expression of Kir4.1 [64, 67], while Müller cells under diabetic stress conditions present an altered Kir4.1 location and activity [67, 69]. The redistribution of this channel in Müller cells has been recognized as the cause of reduced K+ conductance, that can result in an imbalance in K+ concentrations and disrupted K+ homeostasis and ultimately causing neuronal excitation and subsequent glutamate toxicity [34]. AQP4, on the other hand, shows an increased expression in astrocytes in hyperglycemic conditions [70], and although AQP4 role in DR is largely unknown, it has an increased expression in the vitreous of DR patients and in experimental models of DR, possibly as compensatory mechanism [71, 72]. This increase in AQP4 leads to impaired channel activity and glymphatic dysregulation [72, 73]. These alterations in Kir4.1 and/or AQP4 expression or activity in diabetic stress conditions are linked to a wide range of effects such as water and ion disruption homeostasis, Müller cell swelling, decrease glutamate recycling and gliosis, and even reduced Aβ clearance from the retina [34, 69].
In the brain, the glymphatic system contributes to Aβ and tau clearance, and the loss of polarity of AQP4 in the endfeet of astrocytes along with its upregulation in reactive astrocytes has been largely described in AD rodent models [74, 75]. Similarly, a dysfunctional glymphatic system has been also linked to cognitive impairment in T2D animal models [76, 77], possibly due to a downregulation of astrocytic Kir4.1 [68]. Likewise, spinal glymphatic system has been also found impaired in DPN due to reversed polarity of AQP4 in T2D rats [55, 78].
Microglia
Tissue-resident macrophages and sentinels of the CNS, microglia represent 10–15% of human brain [79, 80]. Microglia adapt to different CNS microenvironments, expressing a range of markers, density, and morphology, thus displaying different functional features [81, 82]. Besides being considered the sentinels of the CNS, microglial functions also encompass neuronal network preservation and trophic support through synaptic pruning, neuronal debris clearance, synaptic control, myelination, angiogenesis, and blood barrier maintenance [80, 82,83,84]. The wide range of functions associated with microglia are facilitated by their capacity to migrate and perform constant CNS surveillance, to rapidly adapt and respond to CNS environmental changes together with their phagocytic activity [80, 82].
Gliosis and inflammation
Alterations in microglia have been observed not only in T2D animal models such as db/db mice, but also in diabetic patients, both with and without proliferative DR [81, 85]. Microglia response to sustained diabetic insults, include alterations in microglial migration and enhance secretion of pro-inflammatory and apoptotic microglial mediators in the retina, optic nerve, spinal cord, and brain [85,86,87,88].
The diabetic milieu, which comprises continuous exposure to hyperglycemia, oxidative stress, ischemia, and hypoxia, have been shown to alter microglial phenotypic states toward an ameboid shape, increased migration and proliferation, and release of a diverse repertoire of cytokines and chemokines in several diabetic animal models [81, 85]. In the diabetic retina, microglia have been described to migrate into the plexiform layer, where they acquire a hypertrophic morphology, surround neovascular areas and proliferate [88]. Ophthalmological examinations of patients with DR found hyper-reflective spots, corresponding with aggregates of activated microglia whose changes in number, migration, and phenotype in the retina correspond with the clinical progression of DR [86, 89]. These changes lead to a sustained microglial responsive phenotype that exacerbates DR pathology by perpetuating chronic neuroinflammation and neuronal damage [81, 90]. This is in part mediated by the increased microglial secretion of a plethora of pro-inflammatory cytokines and chemokines (e.g., TNF-α, IL-6, IL-1β, nitric oxide, CCL-2, and complement), which can accumulate in the vitreous, especially in those diabetic patients undergoing proliferative DR [81, 90, 91]. Besides their inflammatory role, microglia could also alter retinal vasculature in DR. Juxtavascular microglia, a type of microglia located close to the vasculature and previously described in the brain [92], has been associated with the phagocytic removal of dying pericytes and vascular smooth muscle cells in DR, which might have potential implications in the vasodegenerative pathology of DR[93].
In addition, bidirectional feedback between Müller cells and microglia has been described, especially after retinal injury such as DR, further sustaining gliosis and inflammation [40, 94]. In response to diabetic insults, Müller cells, possibly via CD40 receptor, elicit the secretion of chemokines CCL-2 and CCL-3 and increase the expression of VCAM-1 and ICAM-1 adhesion proteins, which guide the intraretinal microglial mobilization, further enhancing microglial inflammatory response [94, 95]. Besides, and in line with what has already been described for reactive neurotoxic astrocytes in AD [96], microglia strongly influence Müller cell morphology and function leading to retinal ganglion cell death [94].
In different experimental models of DPN secondary to both, T1D and T2D, spinal cord microglia show similar features to the ones described in DR, with an increased expression of microglia markers CD11b, enhanced phosphorylation in different kinases and hypertrophied microglia [97, 98]. These changes are more pronounced in the vicinity of the L4 segment in the dorsal horn [87], area that is innervated by myelinated fibers connecting the L4 dorsal root ganglia sensory neurons and the hind paw [99, 100]. This is consistent with several studies observing tactile allodynia in the hind paw of diabetic models and in the distal regions of diabetic patients such as feet and ankles. In line with what we have described for the retina, spinal cord microglia in diabetic models also show an increased production of common inflammatory cytokines and chemokines, namely TNF-α, IL-6, IL-1β, CCL-2, CCL-3, CCL-5, and CXCL-12, further contributing to DPN [99, 100].
In the brain, on the other hand, microglial alterations observed in diabetes are linked to those already extensively described in AD [7, 85, 101], including microglia increase in IBA-1 expression, proliferation, changes in morphology, and the presence of microglia that exhibit gene expression patterns associated with pro-inflammatory disease-associated microglia (DAM) [85, 101]. Moreover, T2D exacerbated the microglial pathology in different mouse models of AD, highlighting the potential overlapping pathological mechanisms between AD and diabetes. For example, in the mixed murine model of AD and T2D APP/PS1xdb/db mouse model, T2D significantly increased the number of microglia located in areas free of senile plaques as well as in the number of spontaneous hemorrhages [102]. On the other hand, in the APswe/Psi1dE9/TauP301L mouse model, when exposed to a typical western diet to induce diabetes, microglia response to β-amyloid and Tau pathology was reduced, with a decreased phagocytic uptake and amyloid plaque clearance, along with less microglia located also in the vicinity of β-amyloid plaques in obese individuals with T2D than in those without T2D [103].
These observations have been validated through mechanistic studies in which primary microglia have been exposed to hyperglycemic conditions, which enhanced their proliferation and the production of pro-inflammatory factors such as TNF-α, CCL-2, oxygen radicals, stress proteins (e.g., HSP80), reactive oxygen species (ROS), heme oxygenase 1 (HO-1), and inducible nitric oxide synthase (iNOS), further maintaining pro-inflammatory microglial phenotype [81, 104, 105]. Interestingly, microglial cells that were under hyperglycemia and were then returned into normoglycemic conditions showed increased metabolic stress, bcl-2 and caspase-3-mediated apoptosis and autophagy, potentially further contributing to neurovascular complications [105].
Therefore, the continuous hyperglycemic insult in diabetes greatly impact microglia phenotype and function across the different regions of the CNS (optic nerve, retina, brain, and spinal cord), exacerbating microglial release of pro-inflammatory mediators and morphological shift to ameboid, creating a feedback loop that sustains chronic inflammation, and thus neurodegeneration.
Oligodendrocyte lineage cells
Oligodendrocyte lineage cells encompass two groups of cells, on the one hand oligodendrocyte progenitor cells (OPCs) which are responsible for giving raise to oligodendrocytes in development and in response to injury, and on the other hand oligodendrocytes, the cells responsible for forming myelin in the CNS [106]. Myelin is an insulating lipid rich layer that surrounds axons, providing physical protection, trophic support and allowing the fast saltatory conduction of action potentials [107]. Even though myelin alterations in the CNS were initially associated exclusively with primary demyelinating diseases, such as multiple sclerosis or leukodystrophies, it is now widely accepted that myelin alterations are present in a wide range of neurological disorders including autism spectrum disorders, Parkinson’s disease, or AD [108]. As we mentioned, even if diabetes is not initially considered a neurodegenerative disease, it shares many CNS neurodegenerative hallmarks with AD, and myelin alterations are not an exception.
Loss of myelin sheaths has already been extensively described both, in diabetic CNS and PNS, around the 1960s [109, 110], with white matter hyperintensities observed in MRI of diabetic patients [111]. Already in the 1980s, it was established that the whole brain and especially brain myelin undergo excessive glycosylation in diabetes, with 3.8 more glycosylation than normal brain myelin, which may contribute to the functional abnormalities of myelinated neurons observed in diabetes [112]. However, the specific changes underlying myelin loss in the diabetic CNS are only starting to be elucidated. It has now been established that myelin alterations are present early, prior to neurodegeneration, both, first in the PNS and then in more advanced diabetic stages, in the CNS. Lipid profile analysis of the cortex of STZ-treated diabetic rats revealed that diabetes alters myelin composition in the CNS impacting phosphatidylcholine, phosphatidylethanolamine, plasmalogen, cholesterol, and polyunsaturated fatty acid levels, which are significantly decreased in the cerebral cortex myelin. Besides changes in myelin lipid composition, alterations in myelin basic protein (MBP), the most abundant myelin protein but not proteolipid protein (PLP) were also observed in STZ-treated rats. Surprisingly, treatment with dihydroxyprogesterone every other day for a month reversed all these changes, restoring myelin composition to the levels of healthy control rats [113]. Work performed by a different research group addressed spatiotemporal lipidomic changes in the CNS of db/db mice at 1, 2, and 4 months of age, further validating and expanding the previously described alterations in CNS myelin lipid composition. Sulfatide and cerebrosides were found significantly decreased in the spinal cord but not the brainstem of 1-month-old db/db mice and even further decreased at 2 and 4 months old. At 2 months old, not only sulfatides and cerebrosides, but also plasmalogens were reduced in the CNS, both in the spinal cord and the brainstem, while phosphatidylcholine levels were not altered. In vivo electrophysiological studies showed that myelin alterations in the CNS preceded neuronal functional changes, as electrophysiological changes were only detected in db/db mice at 4 months. Myelin ultrastructural analysis revealed no changes at 4 months between control and db/db mice in the CNS, suggesting that lipid changes occur prior to late-stage myelin loss in the CNS. These results were replicated in other diabetic models including high-fat diet model and STZ model [23].
Myelin loss is generally rapidly restored through a process known as remyelination, a regenerative process by which OPCs respond to myelin damage differentiating into myelinating oligodendrocytes and restabilizing myelin around denuded CNS axons [106]. However, this response appears to be hampered in diabetic models, which show an impaired oligodendrogenesis, aggravating symptoms and neuronal damage observed in other injuries such as stroke. T2D multiplies the risk of developing stroke fourfold by increasing neuronal tissue loss, white matter damage, and limiting oligodendrogenesis. OPC proliferation and the generation of new myelinating oligodendrocytes was significantly impaired in db/db mice upon middle cerebral artery occlusion, with significantly lower NG2+BrdU+ cells in the cortex. This translates into a decrease in the amount of MBP protein present 35 days upon stroke in db/db mice [114]. These results were also observed in another model of stroke, bilateral common carotid artery stenosis, in db/db mice. Diabetic mice also showed a decrease in the number of GSTpi+ oligodendrocytes 4 and 8 weeks after ischemia, as well as in the number of PDGFRα+ OPCs and proliferating OPCs. In addition, a decreased survival of proliferating OPCs upon ischemic stroke was also detected in db/db mice compared to heterozygous db/ + controls. Thus, diabetic mice exhibit a more severe white matter injury and a poorer recovery upon ischemic stroke, suggesting that diabetes may impair myelin regenerative capacity [115]. Similarly, STZ-treated mice show less exploratory behavior and more anxiety 4–8 weeks after treatment started, which is associated with a decrease in the number of OPC and MBP+ oligodendrocytes. This result is further supported by in vitro experiments, in which a hyperglycemic environment impairs OPC survival and migration, two key steps in CNS myelin regeneration [116]. These results are also replicated in the optic nerves of STZ-treated mice, which show a decrease in the number of oligodendrocytes and a decreased expression of PLP and MAG myelin proteins and nodal proteins. Electron microscopy analysis confirmed the decreased number of myelinated axons and nodes of Ranvier, corroborating myelin alterations in diabetic optic nerve. Treatment with Clemastine, a muscarinic receptor agonist shown to be able to restore remyelination, restored oligodendrocyte number and promoted optic nerve functional recovery in STZ-diabetic mice [117]. In addition, Metformin, a commonly used anti-diabetic drug, has recently been shown to have potent pro-remyelinating effects, potentially alleviating some of the cognitive symptoms observed in diabetic patients through this mechanism [118].
Therefore, systemic alterations underlying diabetes affect both, myelin maintenance and regeneration in the CNS. Drugs known to restore myelin regeneration in the CNS such as Clemastine or Metformin, are potentially capable of reversing some of the diabetic-induced neurological alterations at least partially through changes in myelin, suggesting that pro-myelinating drugs may open a new window of opportunity to prevent diabetes-associated neurodegeneration.
Peripheral nervous system glia
Schwann cells
SCs are the most abundant glial cells of the PNS and ensheath either myelinating or unmyelinating peripheral nerve axons [119, 120]. SCs are essential in maintaining conduction of electrical impulses along PNS axons, supporting nerve development and regeneration, and providing peripheral nerve axons metabolic and neurotrophic support [121]. DPN is one of the most common complications of diabetes, affecting more than half of the people suffering from diabetes during the course of the disease. Neuronal damage leading to DPN is associated with diabetes-induced changes in SCs that jeopardize the production and release of neuronal support factors and lead to the accumulation of neurotoxic and pro-inflammatory factors, such as (TNF)-α, interleukin (IL)-1α, IL-1β, MCP-1, CCL2, LIF, and CXCL2, contributing to the endothelial dysfunction, axonal degeneration, and neuronal damage underlying DPN [119, 122, 123]. Even if the nature of the primary lesion in DPN (demyelination or axonal loss) is still controversial, it is now well established that SCs play a key role in DPN pathogenesis.
Innervation
Autonomic dysfunction associated with altered innervation is common in DPN and affects several important functions. DPN is characterized by a progressive, distal-to-proximal degeneration of peripheral nerves, with unmyelinated small caliber nerve fibers being impacted first, followed by large-myelinated fibers [124]. Experiments assessing footpad autonomic innervation and sweating in db/db mice unveiled that unmyelinated fibers innervating sweat glands were more prominently affected than their unmyelinated epidermal sensory counterparts in the early diabetic stages [125]. Besides, db/db mice display progressive sensory loss and electrophysiological impairment in the early to-mid phases of the disease partially, at least, due to a decrease in intraepidermal nerve fiber density, and thus sensory loss. This sensory loss is highly associated with SC apoptosis and T cell infiltration in the sciatic nerve, which perpetuate inflammation and neuronal loss [126]. In addition, recent studies have also shown that DPN can affect adipose tissue innervation. Subcutaneous white adipose tissue (scWAT) contains both, myelinated and unmyelinated nerves, as well as SCs linked to synaptic vesicle-containing nerve terminals, suggesting that SC may be involved in regulating tissue nerve plasticity. However, in a type 2 diabetes model based on BTBR which carries a homozygous spontaneous and recessive mutation (Lepob) in the leptin gene (ob/ob mice), the adipose tissue develops small fiber demyelinating neuropathy with changes in SC marker gene expression, like what has been described in diabetic human adipose tissue. Thus, SC regulation of tissue nerve plasticity may also become altered as a consequence of diabetes [127].
Impaired neurotrophic support
During SC maturation and alignment, a variety of neurotrophic factors and adhesion molecules, such as nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF), and neurotrophins (NT-3, NT-4 or NT-5), are released, which orchestrate neuronal sprouting and targeting [128, 129]. Several studies have shown that diabetes impacts SC capacity to produce neurotrophic factors, limiting their capacity to support axonal growth and thus, contributing to DPN development and progression. For example, SCs show a decreased production of BDNF in the sciatic nerve of STZ-treated diabetic animals, similarly to SC ciliary neurotrophic factor-like activity, which is also reduced in SCs upon STZ treatment. This decrease in BDNF secretion is associated with the increased systemic glucose in diabetes, as SCs in culture under hyperglycemic conditions show reduced BDNF levels [130]. Similarly, SCs in hyperglycemic conditions show an impaired production and secretion of both, NGF and NT-3, which are essential for peripheral nervous system regeneration. This decline in NGF and NT-3 translates into an impaired neurite outgrowth of dorsal root ganglion and a poor association between neurons and SCs in SC-dorsal root ganglion co-cultures in diabetic conditions [131]. Moreover, in a situation of peripheral nerve injury, SCs have the capacity to reprogram and de-differentiate into repair SC phenotype that provides support and accelerates repair [132]. However, in db/db mice, skin wound healing was delayed and SCs failed to activate their repair program in a timely manner due to functional impairments in cell de-differentiation, cell-cycle re-entry and cell migration, problems associated with hyperglycemia as shown by in vitro experiments [133].
Inflammation
Recently, SCs have been recognized as immune-competent cells, exhibiting immune functions like the non-myelinating glia of the CNS [134, 135]. SCs can express major histocompatibility complex II molecules as well as adhesion molecules, several toll-like and inflammatory receptors and produce several cytokines and chemokines. These processes become exacerbated in the inflammatory conditions present in DPN. Under high glucose and oxidative stress conditions, like those observed in diabetes, SCs express increased levels of nuclear factor-κβ (NF-κβ), Toll-like receptors (e.g., TLR4) and pro-inflammatory cytokines and chemokines such as TNF-α, IL-6, IL-1β, CXCL9, CXCL10, and CXCL11 [120, 136,137,138]. These inflammatory cytokines can directly sensitize Aδ and C-fibers or contribute to the activation and recruitment into DPN tissues of other immune cells such as macrophages and CD8+Tcells, which in turn can trigger cytotoxicity by activating apoptosis toward SCs, thus perpetuating injury [136]. In addition, SCs p75 neurotrophin receptor (p75NTR), which is significantly downregulated in diabetes, regulates the neuroinflammatory landscape and promotes phagolysosomal remodeling in high-fat-diet-induced DPN. Therefore, the decreased expression of p75NTR in diabetic-like SCs leads to a significant upregulation of genes associated with inflammatory and immune functions such as Il7r, Serpina3n or Cxcl13 in SCs, suggesting that SCs have a primary contribution to DPN, as this pro-inflammatory phenotype may contribute to peripheral nerve degeneration [139].
Myelin maintenance
As mentioned previously, myelin alterations associated with diabetes were already described in the PNS in the 1960s [109, 110]. Electron microscopy images of the sural nerve of diabetic patients with or without neuropathy showed that even if fibers had similar diameter, peripheral nerve myelin sheaths of patients with DPN not only had fewer lamellae but also showed segmental demyelination and remyelination, suggesting a primary deficit in SCs [109, 140, 141]. To uncover the specific alterations underlying myelin changes in DPN, several groups have studied peripheral nerve myelin composition. An initial lipidomic analysis revealed that myelin of STZ-treated rats sciatic nerve showed a decrease in phospholipids, fatty acid, and cholesterol content. In line with this, they also observed a reduced expression of the genes associated with fatty acid biosynthetic pathway as well as a decreased expression of sterol regulatory element binding factor-1c (SREBF-1c), a key lipogenic factor. In addition, myelin protein P0, which is one of the major components of sciatic nerve myelin, was also decreased in STZ-treated rats. Electron microscopy analysis showed that STZ-treated rats had an increased number of abnormal fibers and myelin infoldings. STZ-treatment-associated PNS phenotype was surprisingly reversed by the activation of the nuclear receptor liver X receptor (LXR), a gene upstream SREBF-1c and a major regulator of fatty acid biosynthesis [142]. More recent spatiotemporal lipidomic analysis of db/db mice, STZ-treated mice, and mice exposed to high-fat diet validated this initial diabetic PNS myelin lipid profile and showed an altered lipid composition already in 1-month-old db/db mice. Lipidomic results revealed a significant decrease in total sulfatide, cerebrosides, and plasmalogen levels in PNS myelin, while phosphorylcholine was not altered. These changes were further exacerbated with age in the PNS. Electrophysiological studies to determine the conduction velocities of peripheral nerves in these mice show no alterations at 2 months of age, indicating that myelin alterations proceed axonal loss in the PNS. Electron microscopy analysis of myelin in 4-month-old db/db confirmed a significant decrease in average PNS myelin thickness, in line with the observed lipidomic changes, while axon caliber was not affected. These alterations in lipid content also translated into changes in both, myelin proteins and mitochondrial function in the PNS, as indicated by an increase in MBP at 1 month of age that was rapidly reverted into an MBP loss by 2 and 4 months of age, and significant effect in oxygen flux in sciatic nerve, indicating that global respiratory capacity was significantly impaired in db/db mice [23]. Myelin thinning and the presence of patches of demyelination and remyelination in the PNS suggest that demyelination is a pathological feature of DPN, even though the mechanisms behind DPN-linked demyelination remain unclear. This PNS demyelination could at least in part be caused by SC-mediated myelin degradation. A recent publication has shown a key role for mixed lineage kinase domain-like protein (MLKL), which participates in regulating necroptosis and is induced in SCs in STZ-induced diabetic model. Moreover, MLKL upregulation and subsequent phosphorylation in the serine 441 is responsible for SC-mediated demyelination and subsequent decrease in nerve conduction velocity, which was prevented either by SCs-specific MLKL knockout or by inhibiting MLKL pharmacologically [143]. An alternative or additional mechanism that may potentially contribute to PNS demyelination in DPN involves the formation of advanced glycation end products (AGEs). The formation of AGE has been liked to PNS myelin in diabetic neuropathy. PNS myelin modified by AGEs is more susceptible to macrophage-mediated phagocytosis, and thus facilitates myelin loss. Altogether, AGEs-modified PNS myelin together with changes in major axonal cytoskeletal proteins derived from AGEs-based modifications translate into impaired axonal transport and subsequent nerve degeneration [138].
Therefore, SCs play a key role in several aspects of DPN including PNS nerve innervation, myelination, and demyelination and the expression of inflammatory molecules that perpetuate peripheral chronic inflammation. Even it is yet to be determined whether the first event triggering DPN is axonal loss or demyelination, there is mounting evidence pointing toward a role for SCs in DPN pathology.
Satellite glial cells
SGCs are located surrounding neuronal soma in the sensory and autonomic PSN ganglia, establishing a narrow 20 nm gap between the neuron and SGCs, which allows a tight control of the neuronal extracellular space and a bidirectional communication between neurons and SGCs [144]. It is now well established that SGCs express neurotransmitter receptors, transporters, and ion channels, been capable of monitoring neuronal activity and responding to neuronal stress by proliferation, upregulation of GFAP, connexin 43 and P2 receptors [145]. Even though their biology remains largely unknown, their close communication with the perineuronal environment makes them an attractive target to treat peripheral neuropathies.
SGC to neuron signaling is regulated by the P2X7 receptor, which activation leads to the release of TNF-α and ATP by SGCS and subsequently drives neuronal hyperexcitability [25]. In STZ-diabetic models, SGCs increase GFAP expression through the upregulation of P2X7. Inhibiting upregulation of P2X7 receptors in SGCs reduced SGCs response and subsequent TNF-α release, decreasing dorsal root ganglia (DRG) hyperexcitability, and thus limiting thermal and mechanical hyperalgesia in diabetic rats [25, 146,147,148]. Besides, hyperglycemia has been recently shown to induce an increase expression of pro-inflammatory lipocalin-2 (LCN2) in DRG SGCs, potentiating neuroinflammation and neurotoxicity via LCN2-pyruvate dehydrogenase kinase isoform 2 (PDK2)-lactic acid pathway contributing to the progression of DPN [146]. Lastly, a recent study pointed toward a potential role of septin-9 (SEPT9), an upstream regulation of a N-methyl-D-aspartate receptor subunit NR2B on SGCs as a mechanism of mechanical nociception in PDN [149].
Hence, despite not being fully characterized yet, SGCs appear to contribute to DPN by modulating neuronal excitability and therefore altering the response to thermal and mechanical stimuli in DPN. Due to their proximity to DRG neurons and their close bidirectional communication, SGCs appear as a promising future target to modulate and limit DPN progression.
Enteric nervous system glia
Enteric glial cells
Diabetes can lead to various complications affecting multiple organs, and the gastrointestinal (GI) tract is no exception. Diabetic patients often suffer from GI motility disorders that result in symptoms such as nausea, vomiting, bloating, and constipation. Although the underlying mechanisms of these disorders are not yet fully understood, recent studies have highlighted the potential role of enteric glial cells (EGCs) in diabetes-associated GI pathophysiology [150].
EGCs are a population of non-myelinating glial cells and the most numerous glial cell type in the enteric nervous system (ENS), which is a complex network of neurons and glia that controls GI function. EGCs play crucial roles in maintaining ENS function such as supporting the integrity and function of enteric neurons and regulating GI motility, inflammation, and epithelial barrier function. EGCs develop from neural crest precursors during embryonic days 9 to 13.5 in mice, and cells expressing markers of terminally differentiated glia such as S100β and GFAP are present by E14.5–16 [151, 152]. Mature EGCs are similar in morphology to astrocytes and express similar molecular markers, such as Aldh1L1. They also express SCs or oligodendrocyte markers such as Sox10 and Plp1 [153]. In addition, EGCs share the capacity of astrocytes to regulate tight-junction integrity and cellular interactions comparable with those maintaining the blood–brain barrier, creating the proper microenvironment for enteric neurons [154].
Several studies have investigated the potential involvement of EGCs in the pathophysiology of GI complications in diabetes. Autonomic neuropathy caused by diabetes mellitus is related to quantitative and morphometric changes in the enteric neurons in various GI segments, associated with the reduced levels of glutathione observed in diabetic patients [155, 156]. In addition, neurons depend directly on glial cells for glutathione synthesis, while glial cells directly promote neuronal protection by increasing the intracellular content of total glutathione and protecting enteric neurons against oxidative stress [157, 158]. Furthermore, glial preservation may be attributable to the resilience of the glial cell population and a defense mechanism exerted by glia in an attempt to promote the maintenance of neurons after the development of peripheral diabetic neuropathy [155]. In addition, EGCs secrete neurotrophic factors, such as glial-cell-derived neurotrophic factor (GDNF), NGF, and transforming growth factor-beta (TGF-β), which contribute to the maintenance of endothelial integrity and vasodilation. EGC-mediated GDNF secretion rescues hyperglycemia-mediated enteric neuronal loss through the activation of the PI3K/Akt pathway [159, 160]. However, in diabetes, EGCs can also present a reduction in the expression of neurotrophic factors or neurotrophins responsible for promoting neuronal survival and maintenance, thus contributing to the development of the disease [155, 160]. Besides changes in neurotrophic factors, EGCs also present alterations in GFAP expression in diabetes. GFAP expression changes in EGCs could be the consequence of unviable extracellular conditions such as hyperosmolarity, low nutrient availability or increased oxidative stress [160]. These findings suggest that there are complex interactions between enteric neurons and glial cells, which play an important role in the pathogenesis of diabetic enteric neuropathy.
In summary, EGCs play critical roles in the regulation of GI function and may contribute to the pathophysiology of GI complications in diabetes. Understanding the mechanisms underlying EGC dysfunction in diabetes and developing new therapies targeting EGCs may provide promising avenues for the treatment of GI motility disorders in diabetic patients.
Concluding remarks
This review summarizes glial cell alterations observed in the three most common and disabling neural diabetic complications, namely DR, DPN, and cognitive decline. Glial cells are known to have key roles in neuronal support and maintenance in the CNS, the PNS, and the ENS, which are significantly altered in diabetes (Fig. 2). Thus, understanding the mechanisms by which glial cells contribute to the pathogenesis and neurological progression of diabetes will open new avenues to develop therapeutic approaches aiming at preventing neurodegeneration, both in the CNS and PNS. Limiting neurodegeneration will restrain DR, DPN, and cognitive decline progression, thus decreasing the main health and economic burden associated with diabetes, and thus restricting the impact of diabetes in the society.
Summary of the glial cell alterations described in the most common neural diabetic complications. Glial cells show altered functions in the retina, as well as the peripheral and enteric nervous system, where they share common and unique alterations in response to diabetes. This figure was created with BioRender.com. AQP4 aquaporin-4, BDNF brain-derived growth factor, CNS central nervous system, CXCL C-X-C motif chemokine ligand, DRG dorsal root ganglia, ENS enteric nervous system, GFAP glial fibrillary acidic protein, GLAST glutamate aspartate transporter, GLT-1 glutamate transporter-1, GS glutamine synthase, IFN interferon, IL- interleukin, NGF nerve growth factor, NT neurotrophin, PNS peripheral nervous system, TNF tumor necrosis factor, VEGF vascular endothelial growth factor
Data availability
Not applicable.
Abbreviations
- Aβ:
-
Amyloid β
- AD:
-
Alzheimer’s disease
- AGEs:
-
Advance glycation end products
- APP/PS1:
-
APPswe/PS1ΔE9, double transgenic mice expressing a chimeric mouse/human amyloid precursor protein (Mo/HuAPP695swe) and a mutant human presenilin 1 (PS1-dE9) Alzheimer’s disease mouse model
- AQP4:
-
Aquaporin-4
- ATP:
-
Adenosine tri-phosphate
- BBB:
-
Blood–brain barrier
- BDNF:
-
Brain-derived neurotrophic factor
- BrDU:
-
Bromodeoxyuridine
- BRB:
-
Blood–retinal barrier
- BTBR ob/ob:
-
ob/ob Mice on a BTBR background (BTBR.Cg-Lep.ob/WiscJ)
- CCL:
-
Chemokine ligand
- CXCL:
-
C-X-C motif chemokine ligand
- CD:
-
Cognitive decline
- CD11b:
-
Macrophage-1-antigen, also known as OX-42
- CD-AD:
-
Cognitive decline and Alzheimer’s disease
- CNS:
-
Central nervous system
- DAM:
-
Disease-associated microglia
- db/db:
-
Type 2 diabetes mouse model (Leprdb)
- DPN:
-
Diabetic peripheral neuropathy
- DR:
-
Diabetic retinopathy
- DRG:
-
Dorsal root ganglion
- EGC:
-
Enteric glial cells
- ENS:
-
Enteric nervous system
- GDNF:
-
Glial-cell-derived neurotrophic factor
- GFAP:
-
Glial fibrillary acidic protein
- GI:
-
Gastrointestinal tract
- GLAST:
-
Glutamate aspartate transporter
- GLT:
-
Glutamate transporter
- GS:
-
Glutamine synthetase
- ICAM-1:
-
Intercellular adhesion molecule
- IL:
-
Interleukin
- iNOS:
-
Inducible nitric oxide synthase
- Kir4.1:
-
Inward rectifying K+ channel subtype 4.1
- LCN2:
-
Lipocalin-2
- MBP:
-
Myelin basic protein
- MLKL:
-
Mixed lineage kinase domain-like protein
- NG2:
-
Neural/glial antigen 2
- NGF:
-
Nerve growth factor
- NT:
-
Neurotrophin
- NVU:
-
Neurovascular unit
- OPC:
-
Oligodendrocyte progenitor cells
- PDK2:
-
Pyruvate dehydrogenase kinase isoform 2
- PDR:
-
Proliferative diabetic retinopathy
- PDGFR:
-
Platelet-derived growth factor receptor
- PLP:
-
Proteolipid protein
- PNS:
-
Peripheral nervous system
- ROS:
-
Reactive oxidative species
- S100β:
-
S100 calcium binding protein β
- SC:
-
Schwann cell
- SCs:
-
Schwann cells
- scWAT:
-
Subcutaneous white adipose tissue
- Sept9:
-
Septin 9
- SGC:
-
Satellite glial cells
- SREBF-1c:
-
Sterol regulatory element binding factor 1c
- STZ:
-
Streptozotocin
- T1D:
-
Type 1 diabetes
- T2D:
-
Type 2 diabetes
- TGF:
-
Transforming growth factor
- TLR:
-
Toll-like receptors
- TNF:
-
Tumour necrosis factor
- VCAM-1:
-
Vascular adhesion molecule
- VEGF:
-
Vascular endothelial growth factor
References
Collaborators G 2019 B and VI, Adelson JD, Bourne RRA, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Global Heal. 2021;9(2):e144-e160. https://doi.org/10.1016/s2214-109x(20)30489-7.
Sun H, Saeedi P, Karuranga S et al (2022) IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pr 183:109119. https://doi.org/10.1016/j.diabres.2021.109119
Mata-Cases M, Casajuana M, Franch-Nadal J et al (2016) Direct medical costs attributable to type 2 diabetes mellitus: a population-based study in Catalonia. Spain European J Heal Econ 17(8):1001–1010. https://doi.org/10.1007/s10198-015-0742-5
O’Connell JM, Manson SM. Understanding the economic costs of diabetes and prediabetes and what we may learn about reducing the health and economic burden of these conditions. Diabetes Care. 2019; 2019;42(9):1609–1611. https://doi.org/10.2337/dci19-0017.
Seuring T, Archangelidi O, Suhrcke M (2015) The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics 33(8):811–831. https://doi.org/10.1007/s40273-015-0268-9
Rasheed R, Pillai GS, Kumar H, Shajan AT, Radhakrishnan N, Ravindran GC (2021) Relationship between diabetic retinopathy and diabetic peripheral neuropathy—Neurodegenerative and microvascular changes. Indian J Ophthalmol 69(11):3370–3375. https://doi.org/10.4103/ijo.ijo_1279_21
Little K, Llorián-Salvador M, Scullion S et al (2021) Common pathways in dementia and diabetic retinopathy: understanding the mechanisms of diabetes-related cognitive decline. Trends Endocrinol Metabolism 33(1):50–71. https://doi.org/10.1016/j.tem.2021.10.008
Abbott CA, Malik RA, Ross ERE van, Kulkarni J, Boulton AJM. Prevalence and Characteristics of Painful Diabetic Neuropathy in a Large Community-Based Diabetic Population in the U.K. Diabetes Care. 2011;34(10):2220–2224. https://doi.org/10.2337/dc11-1108.
Teo ZL, Tham YC, Yu M et al (2021) Global Prevalence of Diabetic Retinopathy and Projection of Burden through 2045 Systematic Review and Meta-analysis. Ophthalmology 128(11):1580–1591. https://doi.org/10.1016/j.ophtha.2021.04.027
Andersson E, Persson S, Hallén N et al (2020) Costs of diabetes complications: hospital-based care and absence from work for 392,200 people with type 2 diabetes and matched control participants in Sweden. Diabetologia 63(12):2582–2594. https://doi.org/10.1007/s00125-020-05277-3
Dyck PJ, Kratz KM, Karnes JL et al (1993) The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: The Rochester Diabetic Neuropathy Study. Neurology 43(4):817–817. https://doi.org/10.1212/wnl.43.4.817
Feldman EL, Callaghan BC, Pop-Busui R et al (2019) Diabetic neuropathy. Nat Rev Dis Primers 5(1):41. https://doi.org/10.1038/s41572-019-0092-1
Jensen TS, Karlsson P, Gylfadottir SS et al (2020) Painful and non-painful diabetic neuropathy, diagnostic challenges and implications for future management. Brain J Neurol 144(6):1632–1645. https://doi.org/10.1093/brain/awab079
Ciudin A, Espinosa A, Simó-Servat O et al (2017) Type 2 diabetes is an independent risk factor for dementia conversion in patients with mild cognitive impairment. J Diabetes Complicat 31(8):1272–1274. https://doi.org/10.1016/j.jdiacomp.2017.04.018
Zhang J, Chen C, Hua S et al (2017) An updated meta-analysis of cohort studies: Diabetes and risk of Alzheimer’s disease. Diabetes Res Clin Pr 124:41–47. https://doi.org/10.1016/j.diabres.2016.10.024
Koekkoek PS, Janssen J, Kooistra M et al (2016) Case-finding for cognitive impairment among people with Type 2 diabetes in primary care using the Test Your Memory and Self-Administered Gerocognitive Examination questionnaires: the Cog-ID study. Diabet Med 33(6):812–819. https://doi.org/10.1111/dme.12874
Kandimalla R, Thirumala V, Reddy PH (2017) Is Alzheimer’s disease a Type 3 Diabetes? A critical appraisal. Biochimica Et Biophysica Acta Mol Basis Dis 1863(5):1078–1089. https://doi.org/10.1016/j.bbadis.2016.08.018
Moran C, Beare R, Phan TG et al (2015) Type 2 diabetes mellitus and biomarkers of neurodegeneration. Neurology 85(13):1123–1130. https://doi.org/10.1212/wnl.0000000000001982
Ramos-Rodriguez JJ, Ortiz O, Jimenez-Palomares M et al (2013) Differential central pathology and cognitive impairment in pre-diabetic and diabetic mice. Psychoneuroendocrino 38(11):2462–2475. https://doi.org/10.1016/j.psyneuen.2013.05.010
Rom S, Zuluaga-Ramirez V, Gajghate S et al (2019) Hyperglycemia-driven neuroinflammation compromises BBB leading to memory loss in both diabetes mellitus (DM) type 1 and type 2 mouse models. Mol Neurobiol 56(3):1883–1896. https://doi.org/10.1007/s12035-018-1195-5
Villarroel M, Ciudin A, Hernández C, Simó R (2010) Neurodegeneration: an early event of diabetic retinopathy. World J Diabetes 1(2):57. https://doi.org/10.4239/wjd.v1.i2.57
Simó R, Stitt AW, Gardner TW (2018) Neurodegeneration in diabetic retinopathy: does it really matter? Diabetologia 61(9):1902–1912. https://doi.org/10.1007/s00125-018-4692-1
Palavicini JP, Chen J, Wang C et al (2020) Early disruption of nerve mitochondrial and myelin lipid homeostasis in obesity-induced diabetes. JCI insight 5(21):300. https://doi.org/10.1172/jci.insight.137286
Stitt AW, Curtis TM, Chen M et al (2016) The progress in understanding and treatment of diabetic retinopathy. Prog Retin Eye Res 51:156–186. https://doi.org/10.1016/j.preteyeres.2015.08.001
Gonçalves NP, Vægter CB, Pallesen LT (2018) Peripheral glial cells in the development of diabetic neuropathy. Front Neurol 9:268. https://doi.org/10.3389/fneur.2018.00268
Yao L, Yang C, Zhang W et al (2021) A multimodal meta-analysis of regional structural and functional brain alterations in type 2 diabetes. Front Neuroendocrin 62:100915. https://doi.org/10.1016/j.yfrne.2021.100915
Oh DJ, Jung J-J, Shin SA, Kim H, Park S, Sohn BK et al (2021) Brain structural alterations, diabetes biomarkers, and cognitive performance in older adults with dysglycemia. Front Neurol 12:766216
Paisley CE, Kay JN (2021) Seeing stars: development and function of retinal astrocytes. Dev Biol 478:144–154. https://doi.org/10.1016/j.ydbio.2021.07.007
Khakh BS, Deneen B (2019) The emerging nature of astrocyte diversity. Annu Rev Neurosci 42(1):187–207. https://doi.org/10.1146/annurev-neuro-070918-05044
Bringmann A, Wiedemann P (2011) Müller glial cells in retinal disease. Ophthalmologica 227(1):1–19. https://doi.org/10.1159/000328979
Ly A, Yee P, Vessey KA, Phipps JA, Jobling AI, Fletcher EL (2011) Early inner retinal astrocyte dysfunction during diabetes and development of hypoxia, retinal stress, and neuronal functional loss. Investigative Opthalmology Vis Sci 52(13):9316. https://doi.org/10.1167/iovs.11-7879
Küser-Abali G, Ozcan F, Ugurlu A, Uysal A, Fuss SH, Bugra-Bilge K (2013) SIK2 Is involved in the negative modulation of insulin-dependent müller cell survival and implicated in hyperglycemia-induced cell death. Investigative Opthalmology Vis Sci 54(5):3526. https://doi.org/10.1167/iovs.12-10729
Trueblood KE, Mohr S, Dubyak GR (2011) Purinergic regulation of high-glucose-induced caspase-1 activation in the rat retinal Müller cell line rMC-1. Am J Physiol-cell Ph 301(5):C1213–C1223. https://doi.org/10.1152/ajpcell.00265.2011
Coughlin BA, Feenstra DJ, Mohr S (2017) Müller cells and diabetic retinopathy. Vision Res 139:93–100. https://doi.org/10.1016/j.visres.2017.03.013
Ly CH, Lynch GS, Ryall JG (2020) A Metabolic Roadmap for Somatic Stem Cell Fate. Cell Metab 31(6):1052–1067. https://doi.org/10.1016/j.cmet.2020.04.022
Wang J, Xu X, Elliott MH, Zhu M, Le YZ (2010) Müller cell-derived VEGF is essential for diabetes-induced retinal inflammation and vascular leakage. Diabetes 59(9):2297–2305. https://doi.org/10.2337/db09-1420
Amin RH, Frank RN, Kennedy A, Eliott D, Puklin JE, Abrams GW (1997) Vascular endothelial growth factor is present in glial cells of the retina and optic nerve of human subjects with nonproliferative diabetic retinopathy. Invest Ophth Vis Sci 38:36–47
Busik JV, Mohr S, Grant MB (2008) Hyperglycemia-induced reactive oxygen species toxicity to endothelial cells is dependent on paracrine mediators. Diabetes 57(7):1952–1965. https://doi.org/10.2337/db07-1520
Qiu AW, Bian Z, Mao PA, Liu QH (2016) IL-17A exacerbates diabetic retinopathy by impairing Müller cell function via Act1 signaling. Exp Mol Medicine 48(12):e280–e280. https://doi.org/10.1038/emm.2016.117
Abcouwer SF (2017) Müller cell-microglia cross talk drives neuroinflammation in diabetic retinopathy. Diabetes 66(2):261–263. https://doi.org/10.2337/dbi16-0047
Byrne EM, Llorián-Salvador M, Tang M, Margariti A, Chen M, Xu H (2021) IL-17A damages the blood-retinal barrier through activating the janus kinase 1 pathway. Biomed 9(7):831. https://doi.org/10.3390/biomedicines9070831
Liu X, Ye F, Xiong H et al (2015) IL-1β Induces IL-6 production in retinal Müller cells predominantly through the activation of P38 MAPK/NF-κB signaling pathway. Exp Cell Res 331(1):223–231. https://doi.org/10.1016/j.yexcr.2014.08.040
Liu Y, Li L, Pan N et al (2021) TNF-α released from retinal Müller cells aggravates retinal pigment epithelium cell apoptosis by upregulating mitophagy during diabetic retinopathy. Biochem Bioph Res Co 561:143–150. https://doi.org/10.1016/j.bbrc.2021.05.027
Bringmann A, Wiedemann P (2009) Involvement of Müller glial cells in epiretinal membrane formation. Graefe’s Archive Clin Exp Ophthalmol 247(7):865–883. https://doi.org/10.1007/s00417-009-1082-x
Roy S, Amin S, Roy S (2016) Retinal fibrosis in diabetic retinopathy. Exp Eye Res 142:71–75. https://doi.org/10.1016/j.exer.2015.04.004
Wu D, Kanda A, Liu Y, Noda K, Murata M, Ishida S (2020) Involvement of Müller glial autoinduction of TGF-β in diabetic fibrovascular proliferation via glial-mesenchymal transition. Invest Ophth Vis Sci 61(14):29. https://doi.org/10.1167/iovs.61.14.29
Nagele RG, Wegiel J, Venkataraman V, Imaki H, Wang KC, Wegiel J (2004) Contribution of glial cells to the development of amyloid plaques in Alzheimer’s disease. Neurobiol Aging 25(5):663–674. https://doi.org/10.1016/j.neurobiolaging.2004.01.007
Nagayach A, Patro N, Patro I (2014) Experimentally induced diabetes causes glial activation, glutamate toxicity and cellular damage leading to changes in motor function. Front Cell Neurosci 8:355. https://doi.org/10.3389/fncel.2014.00355
Yu XJ, Chen YM, Liu XJ et al (2022) Beneficial effects of metformin supplementation in hypothalamic paraventricular nucleus and arcuate nucleus of type 2 diabetic rats. Toxicol Appl Pharm 437:115893. https://doi.org/10.1016/j.taap.2022.115893
Coleman E, Judd R, Hoe L, Dennis J, Posner P. Effects of diabetes mellitus on astrocyte GFAP and glutamate transporters in the CNS. Glia. 2004;48:166–78.
Li W, Choudhury GR, Winters A et al (2018) Hyperglycemia alters astrocyte metabolism and inhibits astrocyte proliferation. Aging Dis 9(4):674–684. https://doi.org/10.14336/ad.2017.1208
Dauch JR, Yanik BM, Hsieh W, Oh SS, Cheng HT (2012) Neuron–astrocyte signaling network in spinal cord dorsal horn mediates painful neuropathy of type 2 diabetes. Glia 60(9):1301–1315. https://doi.org/10.1002/glia.22349
Liao YH, Zhang GH, Jia D et al (2011) Spinal astrocytic activation contributes to mechanical allodynia in a mouse model of type 2 diabetes. Brain Res 1368:324–335. https://doi.org/10.1016/j.brainres.2010.10.044
Kasimu A, Apizi X, Talifujiang D, Ma X, Fang L, Zhou X (2022) miR-125a-5p in astrocytes attenuates peripheral neuropathy in type 2 diabetic mice through targeting TRAF6. Endocrinol Diabetes and Nutrition 69(1):43–51. https://doi.org/10.1016/j.endinu.2021.01.007
Wang G, Wang F, He Y, Lin J (2022) Plasticity of the spinal glymphatic system in male SD rats with painful diabetic neuropathy induced by type 2 diabetes mellitus. J Neurosci Res 100(10):1908–1920. https://doi.org/10.1002/jnr.25104
Pajarillo E, Rizor A, Lee J, Aschner M, Lee E (2019) The role of astrocytic glutamate transporters GLT-1 and GLAST in neurological disorders: Potential targets for neurotherapeutics. Neuropharmacology 161:107559. https://doi.org/10.1016/j.neuropharm.2019.03.002
Mookherjee P, Green PS, Watson GS et al (2011) GLT-1 loss accelerates cognitive deficit onset in an alzheimer’s disease animal model. J Alzheimer’s Dis 26(3):447–455. https://doi.org/10.3233/jad-2011-110503
Rivera-Aponte DE, Méndez-González MP, Rivera-Pagán AF, et al. Hyperglycemia reduces functional expression of astrocytic Kir4.1 channels and glial glutamate uptake. Neuroscience. 2015;310:216–223. https://doi.org/10.1016/j.neuroscience.2015.09.044.
Shi J, Jiang K, Li Z (2016) Involvement of spinal glutamate transporter-1 in the development of mechanical allodynia and hyperalgesia associated with type 2 diabetes. J Pain Res 9:1121–1129. https://doi.org/10.2147/jpr.s118412
Chen SR, Pan HL (2003) Spinal GABAB receptors mediate antinociceptive actions of cholinergic agents in normal and diabetic rats. Brain Res 965(1–2):67–74. https://doi.org/10.1016/s0006-8993(02)04123-9
L Lewis GP, Erickson PA, Guérin CJ, Anderson DH, Fisher SK. Changes in the expression of specific Müller cell proteins during long-term retinal detachment. Exp Eye Res. 1989;49(1):93–111. https://doi.org/10.1016/0014-4835(89)90079-1
Li Q, Puro DG (2002) Diabetes-induced dysfunction of the glutamate transporter in retinal Müller cells. Invest Ophth Vis Sci 43(9):3109–3116
Pannicke T, Iandiev I, Wurm A et al (2006) Diabetes alters osmotic swelling characteristics and membrane conductance of glial cells in rat retina. Diabetes 55(3):633–639. https://doi.org/10.2337/diabetes.55.03.06.db05-1349
Bogdanov P, Corraliza L, Villena JA et al (2014) The db/db Mouse: A Useful Model for the Study of Diabetic Retinal Neurodegeneration. PLoS ONE 9(5):e97302. https://doi.org/10.1371/journal.pone.0097302
Lieth E, LaNoue KF, Antonetti DA, Ratz M, Group TPSRR. Diabetes Reduces Glutamate Oxidation and Glutamine Synthesis in the Retina. Exp Eye Res. 2000;70(6):723–730. https://doi.org/10.1006/exer.2000.0840
Ambati J, Chalam KV, Chawla DK et al (1997) Elevated γ-aminobutyric acid, glutamate, and vascular endothelial growth factor levels in the vitreous of patients with proliferative diabetic retinopathy. Arch Ophthalmol-chic 115(9):1161–1166. https://doi.org/10.1001/archopht.1997.01100160331011
Li X, Lv J, Li J, Ren X. Kir4.1 may represent a novel therapeutic target for diabetic retinopathy (Review). Exp Ther Med. 2021;22(3):1021. https://doi.org/10.3892/etm.2021.10453
Méndez-González MP, Rivera-Aponte DE, Benedikt J, et al. Downregulation of Astrocytic Kir4.1 Potassium Channels Is Associated with Hippocampal Neuronal Hyperexcitability in Type 2 Diabetic Mice. Brain Sci. 2020;10(2):72. https://doi.org/10.3390/brainsci10020072
Llorián-Salvador M, Barabas P, Byrne EM et al (2020) VEGF-B is an autocrine gliotrophic factor for müller cells under pathologic conditions. Invest Ophth Vis Sci 61(11):35. https://doi.org/10.1167/iovs.61.11.35
Guo Y-Z, Ma Y-M, Zhang X-P, Dong L-D, Jing L, Zhang J-Z (2021) Region-specific changes in aquaporin 4 induced by hyperglycemia underlie the differences in cell swelling in the cortex and striatum after cerebral ischemia-reperfusion. Neurosci Lett 754:135885. https://doi.org/10.1016/j.neulet.2021.135885
Vujosevic S, Micera A, Bini S, Berton M, Esposito G, Midena E (2015) Aqueous humor biomarkers of müller cell activation in diabetic eyes. Investigative Opthalmol Vis Sci 56(6):3913. https://doi.org/10.1167/iovs.15-16554
Cui B, Sun J-H, Xiang F-F, Liu L, Li W-J (2012) Aquaporin 4 knockdown exacerbates streptozotocin-induced diabetic retinopathy through aggravating inflammatory response. Exp Eye Res 98:37–43. https://doi.org/10.1016/j.exer.2012.02.013
Oosuka S, Kida T, Oku H, Horie T, Morishita S, Fukumoto M et al (2020) Effects of an Aquaporin 4 Inhibitor, TGN-020, on Murine Diabetic Retina. Int J Mol Sci 21(7):2324. https://doi.org/10.3390/ijms21072324
Silva I, Silva J, Ferreira R, Trigo D (2021) Glymphatic system, AQP4, and their implications in Alzheimer’s disease. Neurological Res Pract 3(1):5. https://doi.org/10.1186/s42466-021-00102-7
Nwaobi SE, Cuddapah VA, Patterson KC, Randolph AC, Olsen ML. The role of glial-specific Kir4.1 in normal and pathological states of the CNS. Acta Neuropathol. 2016;132(1):1–21. https://doi.org/10.1007/s00401-016-1553-1
Jiang Q, Zhang L, Ding G, Davoodi-Bojd E, Li Q, Li L et al (2016) Impairment of the glymphatic system after diabetes. J Cereb Blood Flow Metab 37(4):1326–1337. https://doi.org/10.1177/0271678x16654702
Kim Y-K, Nam KI, Song J (2018) The glymphatic system in diabetes-induced dementia. Front Neurol 9:867. https://doi.org/10.3389/fneur.2018.00867
Xu C, Wang F, Su C, Guo X, Li J, Lin J (2023) Restoration of aquaporin-4 polarization in the spinal glymphatic system by metformin in rats with painful diabetic neuropathy. NeuroReport 34(3):190–197. https://doi.org/10.1097/wnr.0000000000001880
Foster SL, Talbot S, Woolf CJ (2015) CNS Injury: IL-33 Sounds the Alarm. Immunity 42(3):403–405. https://doi.org/10.1016/j.immuni.2015.02.019
Vidal-Itriago A, Radford RAW, Aramideh JA, Maurel C, Scherer NM, Don EK et al (2022) Microglia morphophysiological diversity and its implications for the CNS. Front Immunol 13:997786. https://doi.org/10.3389/fimmu.2022.997786
Kinuthia UM, Wolf A, Langmann T (2020) Microglia and inflammatory responses in diabetic retinopathy. Front Immunol 11:564077. https://doi.org/10.3389/fimmu.2020.564077
Paolicelli RC, Sierra A, Stevens B, Tremblay M-E, Aguzzi A, Ajami B et al (2022) Microglia states and nomenclature: a field at its crossroads. Neuron 110(21):3458–3483. https://doi.org/10.1016/j.neuron.2022.10.020
Lehrman EK, Wilton DK, Litvina EY, Welsh CA, Chang ST, Frouin A et al (2018) CD47 protects synapses from excess microglia-mediated pruning during development. Neuron 100(1):120-134.e6. https://doi.org/10.1016/j.neuron.2018.09.017
Zhao X, Eyo UB, Murugan M, Wu L (2018) Microglial interactions with the neurovascular system in physiology and pathology. Dev Neurobiol 78(6):604–617. https://doi.org/10.1002/dneu.22576
Vargas-Soria M, García-Alloza M, Corraliza-Gómez M (2023) Effects of diabetes on microglial physiology: a systematic review of in vitro, preclinical and clinical studies. J Neuroinflamm 20(1):57. https://doi.org/10.1186/s12974-023-02740-x
Arroba AI, Alcalde-Estevez E, García-Ramírez M, Cazzoni D, de la Villa P, Sánchez-Fernández EM et al (2016) Modulation of microglia polarization dynamics during diabetic retinopathy in db/db mice. Biochimica Et Biophysica Acta Bba - Mol Basis Dis 1862(9):1663–1674. https://doi.org/10.1016/j.bbadis.2016.05.024
Tsuda M. Microglia in the spinal cord and neuropathic pain. 2016;1862(9):1663-1674. https://doi.org/10.1016/j.bbadis.2016.05.024
Zeng H, Green WR, Tso MOM (2008) Microglial activation in human diabetic retinopathy. Arch Ophthalmol-chic 126(2):227–232. https://doi.org/10.1001/archophthalmol.2007.65
Vujosevic S, Bini S, Midena G, Berton M, Pilotto E, Midena E (2013) Hyperreflective intraretinal spots in diabetics without and with nonproliferative diabetic retinopathy: an in vivo study using spectral domain OCT. J Diabetes Res 2013:491835. https://doi.org/10.1155/2013/491835
Altmann C, Schmidt MHH (2018) The role of microglia in diabetic retinopathy: inflammation, microvasculature defects and neurodegeneration. Int J Mol Sci 19(1):110. https://doi.org/10.3390/ijms19010110
Funatsu H, Yamashita H, Noma H, Mimura T, Yamashita T, Hori S. Increased levels of vascular endothelial growth factor and interleukin-6 in the aqueous humor of diabetics with macular edema. Am J Ophthalmol. ):70–77. https://doi.org/10.1016/s0002-9394(01)01269-7.
Mondo E, Becker SC, Kautzman AG, Schifferer M, Baer CE, Chen J et al (2020) A Developmental analysis of juxtavascular microglia dynamics and interactions with the vasculature. J Neurosci 40(34):6503–6521. https://doi.org/10.1523/jneurosci.3006-19.2020
Gardiner TA, Stitt AW (2022) Juxtavascular microglia scavenge dying pericytes and vascular smooth muscle cells in diabetic retinopathy. Int J Transl Medicine 2(1):41–50. https://doi.org/10.3390/ijtm2010004
Wang M, Wong WT (2014) Retinal degenerative diseases, mechanisms and experimental therapy. Adv Exp Med Biol 801:333–338. https://doi.org/10.1007/978-1-4614-3209-8_42
Portillo J-AC, Corcino YL, Miao Y, Tang J, Sheibani N, Kern TS, et al. CD40 in retinal müller cells induces P2X7-dependent cytokine expression in macrophages/microglia in diabetic mice and development of early experimental diabetic retinopathy. Diabetes. 2017;66(2):483–493. https://doi.org/10.2337/db16-0051
Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L et al (2017) Neurotoxic reactive astrocytes are induced by activated microglia. Nature 541(7638):481–487. https://doi.org/10.1038/nature21029
Cheng K-I, Wang H-C, Chuang Y-T, Chou C-W, Tu H-P, Yu Y-C et al (2014) P-p38 MAP kinase activation in microglia and allodynia. Eur J Pain 18(2):162–173. https://doi.org/10.1002/j.1532-2149.2013.00356.x
Xu X, Chen H, Ling B-Y, Xu L, Cao H, Zhang Y-Q (2014) Extracellular signal-regulated protein kinase activation in spinal cord contributes to pain hypersensitivity in a mouse model of type 2 diabetes. Neurosci Bull 30:53–66
Thornton PDJ, Gerke MB, Plenderleith MB (2005) Histochemical localisation of a galactose-containing glycoconjugate expressed by sensory neurones innervating different peripheral tissues in the rat. J Peripher Nerv Syst 10(1):47–57. https://doi.org/10.1111/j.1085-9489.2005.10108.x
Rajchgot T, Thomas SC, Wang J-C, Ahmadi M, Balood M, Crosson T et al (2019) Neurons and microglia; a sickly-sweet duo in diabetic pain neuropathy. Front Neurosci 13:25. https://doi.org/10.3389/fnins.2019.00025
Ma S, Bi W, Liu X, Li S, Qiu Y, Huang C et al (2022) Single-cell sequencing analysis of the db/db mouse hippocampus reveals cell-type-specific insights into the pathobiology of diabetes-associated cognitive dysfunction. Front Endocrinol 13:891039. https://doi.org/10.3389/fendo.2022.891039
Infante-Garcia C, Ramos-Rodriguez JJ, Galindo-Gonzalez L, Garcia-Alloza M (2016) Long-term central pathology and cognitive impairment are exacerbated in a mixed model of Alzheimer’s disease and type 2 diabetes. Psychoneuroendocrino 65:15–25. https://doi.org/10.1016/j.psyneuen.2015.12.001
Natunen T, Martiskainen H, Marttinen M, Gabbouj S, Koivisto H, Kemppainen S et al (2020) Diabetic phenotype in mouse and humans reduces the number of microglia around β-amyloid plaques. Mol Neurodegener 15(1):66. https://doi.org/10.1186/s13024-020-00415-2
Chen C, Wu S, Hong Z, Chen X, Shan X, Fischbach S et al (2019) Chronic hyperglycemia regulates microglia polarization through ERK5. Aging 11(2):697–706. https://doi.org/10.18632/aging.101770
Hsieh C-F, Liu C-K, Lee C-T, Yu L-E, Wang J-Y (2019) Acute glucose fluctuation impacts microglial activity, leading to inflammatory activation or self-degradation. Sci Rep 9(1):840. https://doi.org/10.1038/s41598-018-37215-0
Franklin RJM, ffrench-Constant C. Regenerating CNS myelin—from mechanisms to experimental medicines. Nat Rev Neurosci. 2017;18(12):753–769. https://doi.org/10.1038/nrn.2017.136
Stadelmann C, Timmler S, Barrantes-Freer A, Simons M (2019) Myelin in the central nervous system: structure, function, and pathology. Physiol Rev 99(3):1381–1431. https://doi.org/10.1152/physrev.00031.2018
Ettle B, Schlachetzki JCM, Winkler J (2016) Oligodendroglia and myelin in neurodegenerative diseases: more than just bystanders? Mol Neurobiol 53(5):3046–3062. https://doi.org/10.1007/s12035-015-9205-3
Thomas PK, Lascelles RG (1965) Schwann-cell abnormalities in diabetic neuropathy. Lancet 285(7400):1355–1357. https://doi.org/10.1016/s0140-6736(65)92154-9
Chopra JS (1969) Electromyography in diabetes mellitus and chronic occlusive peripheral vascular disease. Brain 92(1):97–108. https://doi.org/10.1093/brain/92.1.97
Marseglia A, Fratiglioni L, Kalpouzos G, Wang R, Bäckman L, Xu W (2019) Prediabetes and diabetes accelerate cognitive decline and predict microvascular lesions: a population-based cohort study. Alzheimer’s Dementia 15(1):25–33. https://doi.org/10.1016/j.jalz.2018.06.3060
Vlassara H, Brownlee M, Cerami A (1983) Excessive nonenzymatic glycosylation of peripheral and central nervous system myelin components in diabetic rats. Diabetes 32(7):670–674. https://doi.org/10.2337/diabetes.32.7.670
Cermenati G, Giatti S, Audano M, Pesaresi M, Spezzano R, Caruso D et al (2017) Diabetes alters myelin lipid profile in rat cerebral cortex: protective effects of dihydroprogesterone. J Steroid Biochem Mol Biology 168:60–70. https://doi.org/10.1016/j.jsbmb.2017.02.002
Ma S, Wang J, Wang Y, Dai X, Xu F, Gao X et al (2018) Diabetes mellitus impairs white matter repair and long-term functional deficits after cerebral ischemia. Stroke 49(10):2453–2463. https://doi.org/10.1161/strokeaha.118.021452
Yatomi Y, Tanaka R, Shimada Y, Yamashiro K, Liu M, Mitome-Mishima Y et al (2015) Type 2 diabetes reduces the proliferation and survival of oligodendrocyte progenitor cells in ishchemic white matter lesions. Neuroscience 289:214–223. https://doi.org/10.1016/j.neuroscience.2014.12.054
Wang L-P, Geng J, Liu C, Wang Y, Zhang Z, Yang G-Y (2022) Diabetes mellitus-related neurobehavioral deficits in mice are associated with oligodendrocyte precursor cell dysfunction. Front Aging Neurosci 14:846739. https://doi.org/10.3389/fnagi.2022.846739
Wu H, Chen X, Yu B, Zhang J, Gu X, Liu W, et al. Deficient deposition of new myelin impairs adult optic nerve function in a murine model of diabetes. Glia. 2023. Glia. doi:https://doi.org/10.1002/glia.24341
Neumann B, Baror R, Zhao C, Segel M, Dietmann S, Rawji KS et al (2019) Metformin restores CNS remyelination capacity by rejuvenating aged stem cells. Cell Stem Cell 25(4):473-485.e8. https://doi.org/10.1016/j.stem.2019.08.015
Mizisin AP. Chapter 27 Mechanisms of diabetic neuropathy Schwann cells. Handb Clin Neurology. . 2014;126:401–428. doi:https://doi.org/10.1016/b978-0-444-53480-4.00029-1
Gonçalves NP, Vægter CB, Andersen H, Østergaard L, Calcutt NA, Jensen TS (2017) Schwann cell interactions with axons and microvessels in diabetic neuropathy. Nat Rev Neurol 13(3):135–147. https://doi.org/10.1038/nrneurol.2016.201
Chen CZ, Neumann B, Förster S, Franklin RJM (2021) Schwann cell remyelination of the central nervous system: Why does it happen and what are the benefits? Open Biol 11(1):200352–200412. https://doi.org/10.1098/rsob.200352
Tofaris GK, Patterson PH, Jessen KR, Mirsky R (2002) Denervated schwann cells attract macrophages by secretion of leukemia inhibitory factor (LIF) and monocyte chemoattractant protein-1 in a process regulated by interleukin-6 and lIF. J Neurosci 22:6696–6703. https://doi.org/10.1523/JNEUROSCI.22-15-06696.2002
Zhang Y, Sang R, Bao J, Jiang Z, Qian D, Zhou Y et al (2023) Schwann cell-derived CXCL2 contributes to cancer pain by modulating macrophage infiltration in a mouse breast cancer model. Brain, Behav, Immun 109:308–320. https://doi.org/10.1016/j.bbi.2023.02.004
Selvarajah D, Kar D, Khunti K, Davies MJ, Scott AR, Walker J et al (2019) Diabetic peripheral neuropathy: advances in diagnosis and strategies for screening and early intervention. Lancet Diabetes Endocrinol 7(12):938–948. https://doi.org/10.1016/s2213-8587(19)30081-6
Liu Y, Sebastian B, Liu B, Zhang Y, Fissel JA, Pan B et al (2017) Sensory and autonomic function and structure in footpads of a diabetic mouse model. Sci Rep 7(1):41401. https://doi.org/10.1038/srep41401
Gregorio CD, Contador D, Campero M, Ezquer M, Ezquer F. Characterization of diabetic neuropathy progression in a mouse model of type 2 diabetes mellitus. Biol Open. 2018;7(9):bio036830. https://doi.org/10.1242/bio.036830
Willows JW, Gunsch G, Paradie E, Blaszkiewicz M, Tonniges JR, Pino MF et al (2023) Schwann cells contribute to demyelinating diabetic neuropathy and nerve terminal structures in white adipose tissue. Iscience 26(3):106189. https://doi.org/10.1016/j.isci.2023.106189
Gonçalves NP, Mohseni S, Soury ME, Ulrichsen M, Richner M, Xiao J et al (2019) Peripheral nerve regeneration is independent from schwann cell p75NTR expression. Front Cell Neurosci 13:235. https://doi.org/10.3389/fncel.2019.00235
Gordon T (2009) The role of neurotrophic factors in nerve regeneration. Neurosurg Focus 26(2):E3. https://doi.org/10.3171/foc.2009.26.2.e3
Calcutt NA, Muir D, Powell HC, Mizisin AP (1992) Reduced ciliary neuronotrophic factor-like activity in nerves from diabetic or galactose-fed rats. Brain Res 575(2):320–324. https://doi.org/10.1016/0006-8993(92)90097-s
Dey I, Midha N, Singh G, Forsyth A, Walsh SK, Singh B et al (2013) Diabetic Schwann cells suffer from nerve growth factor and neurotrophin-3 underproduction and poor associability with axons. Glia 61(12):1990–1999. https://doi.org/10.1002/glia.22570
Wagstaff LJ, Gomez-Sanchez JA, Fazal SV, Otto GW, Kilpatrick AM, Michael K, et al. Failures of nerve regeneration caused by aging or chronic denervation are rescued by restoring Schwann cell c-Jun. eLife. 2021;10:239–32. https://doi.org/10.7554/elife.62232
Zhou S, Wan L, Liu X, Hu D, Lu F, Chen X et al (2022) Diminished schwann cell repair responses play a role in delayed diabetes-associated wound healing. Front Physiol 13:814754. https://doi.org/10.3389/fphys.2022.814754
Conti G, Scarpini E, Baron P, Livraghi S, Tiriticco M, Bianchi R et al (2002) Macrophage infiltration and death in the nerve during the early phases of experimental diabetic neuropathy: a process concomitant with endoneurial induction of IL-1β and p75NTR. J Neurol Sci 195(1):35–40. https://doi.org/10.1016/s0022-510x(01)00684-0
Lee H, Jo E-K, Choi S-Y, Oh SB, Park K, Kim JS et al (2006) Necrotic neuronal cells induce inflammatory Schwann cell activation via TLR2 and TLR3: implication in Wallerian degeneration. Biochem Bioph Res Co 350(3):742–747. https://doi.org/10.1016/j.bbrc.2006.09.108
Tang W, Lv Q, Chen X, Zou J, Liu Z, Shi Y (2013) CD8+ T cell-mediated cytotoxicity toward schwann cells promotes diabetic peripheral neuropathy. Cell Physiol Biochem 32(4):827–837. https://doi.org/10.1159/000354485
Li J, Guan R, Pan L (2023) Mechanism of Schwann cells in diabetic peripheral neuropathy: a review. Medicine 102(1):e32653. https://doi.org/10.1097/md.0000000000032653
Sugimoto K, Yasujima M, Yagihashi S (2008) Role of advanced glycation end products in diabetic neuropathy. Curr Pharm Design 14(10):953–961. https://doi.org/10.2174/138161208784139774
Gonçalves NP, Jager SE, Richner M, Murray SS, Mohseni S, Jensen TS et al (2020) Schwann cell p75 neurotrophin receptor modulates small fiber degeneration in diabetic neuropathy. Glia 68(12):2725–2743. https://doi.org/10.1002/glia.2388
Sima AA, Nathaniel V, Bril V, McEwen TA, Greene DA (1988) Histopathological heterogeneity of neuropathy in insulin-dependent and non-insulin-dependent diabetes, and demonstration of axo-glial dysjunction in human diabetic neuropathy. J Clin Invest 81(2):349–364. https://doi.org/10.1172/jci113327
Sugimura K, Dyck PJ (1988) Multifocal fiber loss in proximal sciatic nerve in symmetric distal diabetic neuropathy. J Clin Invest 81(2):349–364. https://doi.org/10.1172/jci113327
Cermenati G, Abbiati F, Cermenati S, Brioschi E, Volonterio A, Cavaletti G et al (2012) Diabetes-induced myelin abnormalities are associated with an altered lipid pattern: protective effects of LXR activation. J Lipid Res 53(2):300–310. https://doi.org/10.1194/jlr.m021188
Guo J, Guo Z, Huang Y, Ma S, Yan B, Pan C et al (2022) Blockage of MLKL prevents myelin damage in experimental diabetic neuropathy. Proc National Acad Sci 119(14):e2121552119. https://doi.org/10.1073/pnas.2121552119
Huang LM, Gu Y, Chen Y (2013) Communication between neuronal somata and satellite glial cells in sensory ganglia. Glia 61(10):1571–1581. https://doi.org/10.1002/glia.22541
Hanani M, Spray DC (2020) Emerging importance of satellite glia in nervous system function and dysfunction. Nat Rev Neurosci 21:485–498. https://doi.org/10.1038/s41583-020-0333-z
Bhusal A, Lee W-H, Suk K (2021) Lipocalin-2 in diabetic complications of the nervous system: physiology, pathology, and beyond. Front Physiol 12:638112. https://doi.org/10.3389/fphys.2021.638112
Hanani M, Blum E, Liu S, Peng L, Liang S (2014) Satellite glial cells in dorsal root ganglia are activated in streptozotocin-treated rodents. J Cell Mol Med 18(12):2367–2371. https://doi.org/10.1111/jcmm.12406
Liu S, Zou L, Xie J, Xie W, Wen S, Xie Q et al (2016) LncRNA NONRATT021972 siRNA regulates neuropathic pain behaviors in type 2 diabetic rats through the P2X7 receptor in dorsal root ganglia. Mol Brain 9(1):44. https://doi.org/10.1186/s13041-016-0226-2
Kan H-W, Ho Y-C, Chang Y-S, Hsieh Y-L (2022) SEPT9 upregulation in satellite glial cells associated with diabetic polyneuropathy in a type 2 diabetes-like rat model. Int J Mol Sci 23(16):9372. https://doi.org/10.3390/ijms23169372
Grubišić V, Verkhratsky A, Zorec R, Parpura V (2018) Enteric glia regulate gut motility in health and disease. Brain Res Bull 136:109–117. https://doi.org/10.1016/j.brainresbull.2017.03.011
Ferri G-L, Probert L, Cocchia D, Michetti F, Marangos PJ, Polak JM (1982) Evidence for the presence of S-100 protein in the glial component of the human enteric nervous system. Nature 297(5865):409–410. https://doi.org/10.1038/297409a
Jessen K, Mirsky R. Astrocyte-like glia in the peripheral nervous system: an immunohistochemical study of enteric glia. J Neurosci. 1983;3:2206–18. https://doi.org/10.1523/jneurosci.03-11-02206.1983
Lasrado R, Boesmans W, Kleinjung J, Pin C, Bell D, Bhaw L et al (2017) Lineage-dependent spatial and functional organization of the mammalian enteric nervous system. Science 356(6339):722–726. https://doi.org/10.1126/science.aam7511
Grubišić V, Gulbransen BD (2017) Enteric glia: the most alimentary of all glia. J Physiology 595(2):557–570. https://doi.org/10.1113/jp271021
Pereira RVF, Tronchini EA, Tashima CM, Alves EPB, Lima MM, Zanoni JN (2011) l-Glutamine Supplementation Prevents Myenteric Neuron Loss and Has Gliatrophic Effects in the Ileum of Diabetic Rats. Digest Dis Sci. 56:3507–16. https://doi.org/10.1007/s10620-011-1806-
Tsai P-H, Liu J-J, Chiu W-C, Pai M-H, Yeh S-L (2011) Effects of dietary glutamine on adhesion molecule expression and oxidative stress in mice with streptozotocin-induced type 1 diabetes. Clin Nutr 30(1):124–129. https://doi.org/10.1016/j.clnu.2010.07.00
Vincent AM, Russell JW, Low P, Feldman EL (2004) Oxidative stress in the pathogenesis of diabetic neuropathy. Endocr Rev 25(4):612–628. https://doi.org/10.1210/er.2003-0019
Iwata-Ichikawa E, Kondo Y, Miyazaki I, Asanuma M, Ogawa N (1999) Glial cells protect neurons against oxidative stress via transcriptional Up-regulation of the glutathione synthesis. J Neurochem 72(6):2334–2344. https://doi.org/10.1046/j.1471-4159.1999.0722334.x
Anitha M, Gondha C, Sutliff R, Parsadanian A, Mwangi S, Sitaraman SV et al (2006) GDNF rescues hyperglycemia-induced diabetic enteric neuropathy through activation of the PI3K/Akt pathway. J Clin Invest 116(2):344–356. https://doi.org/10.1172/jci26295
Liu W, Yue W, Wu R (2010) Effects of diabetes on expression of glial fibrillary acidic protein and neurotrophins in rat colon. Autonomic Neurosci 154(1–2):79–83. https://doi.org/10.1016/j.autneu.2009.12.003
Acknowledgements
Even if we have tried to provide a balanced revision of the current state-of-the-art summarizing the changes observed in glial cells in diabetes, we acknowledge that this work will not be comprehensive, and we have not covered the vast body of the corresponding literature. Thus, the authors would like to apologize to colleagues whose work has not been included here or highlighted through a review due to constraints of space and scope.
Funding
This work was supported by a Miguel Servet Fellowship from the Spanish Health Institute Carlos III (CP21/00032 to AGF), a grant from the Spanish State Research Agency corresponding to “Plan Nacional 2021” (PID2021-124465OA-I00 to AGF), the Maria Zambrano fellowship from Spanish Ministry of Science, Innovation and Universities, financed by European Union “NextGenerationEU” (Universitat Autònoma de Barcelona, to MLS), a Miguel Servet Fellowship from the Spanish Health Institute Carlos III (CP22/00078 to JAGS), a grant from the Spanish State Research Agency corresponding to “Plan Nacional 2022” (PID2022-143269OB-I00 to JAGS) and a grant from the “X Convocatoria Intramural 2023” from ISABIAL (Modality F to AGF).
Author information
Authors and Affiliations
Contributions
MLS: conceptualization, resources, writing—original draft, reviewing and editing. SCF resources, figures, reviewing and editing. JAGS: resources, writing—original draft, reviewing and editing. AGF: conceptualization; resources, writing—original draft, reviewing and editing.
Corresponding authors
Ethics declarations
Conflcit of interest
The authors report no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors have consented the publication of this review and we have included the publication license from BioRender for the graphical abstract and all the figures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Llorián-Salvador, M., Cabeza-Fernández, S., Gomez-Sanchez, J.A. et al. Glial cell alterations in diabetes-induced neurodegeneration. Cell. Mol. Life Sci. 81, 47 (2024). https://doi.org/10.1007/s00018-023-05024-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-023-05024-y