Abstract
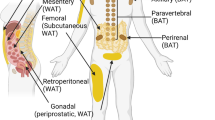
Adipose tissue is located in discrete depots that are differentially associated with elevated risk of metabolic complications, with fat accretion in visceral depots being most detrimental to metabolic health. Currently, the regulation of specific adipose depot expansion, by adipocyte hypertrophy and hyperplasia and consequently fat distribution, is not well understood. However, a growing body of evidence from in vitro investigations indicates that mature adipocytes secrete factors that modulate the proliferation and differentiation of progenitor, adipose-derived stem cells (ADSCs). It is therefore plausible that endocrine communication between adipocytes and ADSCs located in different depots influences fat distribution, and may therefore contribute to the adverse health outcomes associated with visceral adiposity. This review will explore the available evidence of paracrine and endocrine crosstalk between mature adipocytes and ADSCs that affects adipogenesis, as a better understanding of the regulatory roles of the extracellular signalling mechanisms within- and between adipose depots may profoundly change the way we view adipose tissue growth in obesity and related comorbidities.

Similar content being viewed by others
References
Gregg EW, Shaw JE (2017) Global health effects of overweight and obesity. N Engl J Med 377:80–81. https://doi.org/10.1056/NEJMe1706095
Bianchini F, Kaaks R, Vainio H (2002) Overweight, obesity, and cancer risk. Lancet Oncol 3:565–574
Després J-P, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444:881–887. https://doi.org/10.1038/nature05488
Booth A, Magnuson A, Foster M (2014) Detrimental and protective fat: body fat distribution and its relation to metabolic disease. Horm Mol Biol Clin Investig 17:13–27. https://doi.org/10.1515/hmbci-2014-0009
Sun K, Kusminski CM, Scherer PE (2011) Adipose tissue remodeling and obesity. J Clin Invest 121:2094–2101. https://doi.org/10.1172/JCI45887
Sethi JK, Vidal-Puig AJ (2007) Thematic review series: adipocyte biology. Adipose tissue function and plasticity orchestrate nutritional adaptation. J Lipid Res 48:1253–1262. https://doi.org/10.1194/jlr.R700005-JLR200
Wood IS, de Heredia FP, Wang B, Trayhurn P (2009) Cellular hypoxia and adipose tissue dysfunction in obesity. Proc Nutr Soc 68:370–377. https://doi.org/10.1017/S0029665109990206
Rosen ED, MacDougald OA (2006) Adipocyte differentiation from the inside out. Nat Rev Mol Cell Biol 7:885–896. https://doi.org/10.1038/nrm2066
Wajchenberg BL (2000) Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev 21:697–738. https://doi.org/10.1210/edrv.21.6.0415
Neeland IJ, Ayers CR, Rohatgi AK et al (2013) Associations of visceral and abdominal subcutaneous adipose tissue with markers of cardiac and metabolic risk in obese adults. Obes Silver Spring Md 21:E439–E447. https://doi.org/10.1002/oby.20135
Ibrahim MM (2010) Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev Off J Int Assoc Study Obes 11:11–18. https://doi.org/10.1111/j.1467-789X.2009.00623.x
Roca-Rivada A, Alonso J, Al-Massadi O et al (2011) Secretome analysis of rat adipose tissues shows location-specific roles for each depot type. J Proteom 74:1068–1079. https://doi.org/10.1016/j.jprot.2011.03.010
Sam S, Mazzone T (2014) Adipose tissue changes in obesity and the impact on metabolic function. Transl Res J Lab Clin Med 164:284–292. https://doi.org/10.1016/j.trsl.2014.05.008
McGown C, Birerdinc A, Younossi ZM (2014) Adipose tissue as an endocrine organ. Clin Liver Dis 18:41–58. https://doi.org/10.1016/j.cld.2013.09.012
Cook KS, Min HY, Johnson D et al (1987) Adipsin: a circulating serine protease homolog secreted by adipose tissue and sciatic nerve. Science 237:402–405
Zhang Y, Proenca R, Maffei M et al (1994) Positional cloning of the mouse obese gene and its human homologue. Nature 372:425–432. https://doi.org/10.1038/372425a0
Scherer PE, Williams S, Fogliano M et al (1995) A novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem 270:26746–26749
Goralski KB, McCarthy TC, Hanniman EA et al (2007) Chemerin, a novel adipokine that regulates adipogenesis and adipocyte metabolism. J Biol Chem 282:28175–28188. https://doi.org/10.1074/jbc.M700793200
Dahlman I, Elsen M, Tennagels N et al (2012) Functional annotation of the human fat cell secretome. Arch Physiol Biochem 118:84–91. https://doi.org/10.3109/13813455.2012.685745
Roca-Rivada A, Bravo SB, Pérez-Sotelo D et al (2015) CILAIR-based secretome analysis of obese visceral and subcutaneous adipose tissues reveals distinctive ECM remodeling and inflammation mediators. Sci Rep 5:12214. https://doi.org/10.1038/srep12214
Deng Y, Scherer PE (2010) Adipokines as novel biomarkers and regulators of the metabolic syndrome. Ann N Y Acad Sci 1212:E1–E19. https://doi.org/10.1111/j.1749-6632.2010.05875.x
Nakamura K, Fuster JJ, Walsh K (2014) Adipokines: a link between obesity and cardiovascular disease. J Cardiol 63:250–259. https://doi.org/10.1016/j.jjcc.2013.11.006
Spalding KL, Arner E, Westermark PO et al (2008) Dynamics of fat cell turnover in humans. Nature 453:783–787. https://doi.org/10.1038/nature06902
Armani A, Mammi C, Marzolla V et al (2010) Cellular models for understanding adipogenesis, adipose dysfunction, and obesity. J Cell Biochem 110:564–572. https://doi.org/10.1002/jcb.22598
Lee M-J, Fried SK (2014) Optimal protocol for the differentiation and metabolic analysis of human adipose stromal cells. Methods Enzymol 538:49–65. https://doi.org/10.1016/B978-0-12-800280-3.00004-9
Wang QA, Scherer PE, Gupta RK (2014) Improved methodologies for the study of adipose biology: insights gained and opportunities ahead. J Lipid Res 55:605–624. https://doi.org/10.1194/jlr.R046441
Cristancho AG, Lazar MA (2011) Forming functional fat: a growing understanding of adipocyte differentiation. Nat Rev Mol Cell Biol 12:722–734. https://doi.org/10.1038/nrm3198
Kuk JL, Saunders TJ, Davidson LE, Ross R (2009) Age-related changes in total and regional fat distribution. Ageing Res Rev 8:339–348. https://doi.org/10.1016/j.arr.2009.06.001
Shillabeer G, Forden JM, Lau DC (1989) Induction of preadipocyte differentiation by mature fat cells in the rat. J Clin Invest 84:381–387
Pairault J, Green H (1979) A study of the adipose conversion of suspended 3T3 cells by using glycerophosphate dehydrogenase as differentiation marker. Proc Natl Acad Sci USA 76:5138–5142
Shillabeer G, Forden JM, Russell JC, Lau DC (1990) Paradoxically slow preadipocyte replication and differentiation in corpulent rats. Am J Physiol-Endocrinol Metab 258:E368–E376. https://doi.org/10.1152/ajpendo.1990.258.2.E368
Carraro R, Li ZH, Johnson JE, Gregerman RI (1992) Adipocytes of old rats produce a decreased amount of differentiation factor for preadipocytes derived from adipose tissue islets. J Gerontol 47:B198–B201
Li Z-H, Carraro R, Gregerman RI, Lau DCW (1998) Adipocyte differentiation factor (adf): a protein secreted by mature fat cells that induces preadipocyte differentiation in culture. Cell Biol Int 22:253–270. https://doi.org/10.1006/cbir.1998.0237
Li J, Qiao X, Yu M et al (2014) Secretory factors from rat adipose tissue explants promote adipogenesis and angiogenesis. Artif Organs 38:E33–E45. https://doi.org/10.1111/aor.12162
Ailhaud G, Amri E, Bardon S et al (1990) The adipocyte: relationships between proliferation and adipose cell differentiation. Am Rev Respir Dis 142:S57–S59. https://doi.org/10.1164/ajrccm/142.6_Pt_2.S57
Stacey DH, Hanson SE, Lahvis G et al (2009) In vitro adipogenic differentiation of preadipocytes varies with differentiation stimulus, culture dimensionality, and scaffold composition. Tissue Eng Part A 15:3389–3399. https://doi.org/10.1089/ten.TEA.2008.0293
Janderová L, McNeil M, Murrell AN et al (2003) Human mesenchymal stem cells as an in vitro model for human adipogenesis. Obes Res 11:65–74. https://doi.org/10.1038/oby.2003.11
Sarkanen J-R, Kaila V, Mannerström B et al (2012) Human adipose tissue extract induces angiogenesis and adipogenesis in vitro. Tissue Eng Part A 18:17–25. https://doi.org/10.1089/ten.tea.2010.0712
Song K, Li W, Wang H et al (2012) Investigation of coculture of human adipose-derived stem cells and mature adipocytes. Appl Biochem Biotechnol 167:2381–2387. https://doi.org/10.1007/s12010-012-9764-y
Janke J, Engeli S, Gorzelniak K et al (2002) Mature adipocytes inhibit in vitro differentiation of human preadipocytes via angiotensin type 1 receptors. Diabetes 51:1699–1707. https://doi.org/10.2337/diabetes.51.6.1699
Ailhaud G, Fukamizu A, Massiera F et al (2000) Angiotensinogen, angiotensin II and adipose tissue development. Int J Obes Relat Metab Disord J Int Assoc Study Obes 24(Suppl 4):S33–S35
Pinterova L, Krizanova O, Zorad S (2000) Rat epididymal fat tissue express all components of the renin-angiotensin system. Gen Physiol Biophys 19:329–334
Frigolet ME, Torres N, Tovar AR (2013) The renin–angiotensin system in adipose tissue and its metabolic consequences during obesity. J Nutr Biochem 24:2003–2015. https://doi.org/10.1016/j.jnutbio.2013.07.002
Townsend RR (2001) The effects of angiotensin-II on lipolysis in humans. Metabolism 50:468–472. https://doi.org/10.1053/meta.2001.21021
Considine RV, Nyce MR, Morales LM et al (1996) Paracrine stimulation of preadipocyte-enriched cell cultures by mature adipocytes. Am J Physiol-Endocrinol Metab 270:E895–E899. https://doi.org/10.1152/ajpendo.1996.270.5.E895
Hirsch J, Batchelor B (1976) Adipose tissue cellularity in human obesity. Clin Endocrinol Metab 5:299–311
Maumus M, Sengenès C, Decaunes P et al (2008) Evidence of in situ proliferation of adult adipose tissue-derived progenitor cells: influence of fat mass microenvironment and growth. J Clin Endocrinol Metab 93:4098–4106. https://doi.org/10.1210/jc.2008-0044
Valet P, Pagès C, Jeanneton O et al (1998) Alpha2-adrenergic receptor-mediated release of lysophosphatidic acid by adipocytes. A paracrine signal for preadipocyte growth. J Clin Invest 101:1431–1438. https://doi.org/10.1172/JCI806
Wagoner B, Hausman DB, Harris RBS (2006) Direct and indirect effects of leptin on preadipocyte proliferation and differentiation. Am J Physiol Regul Integr Comp Physiol 290:R1557–R1564. https://doi.org/10.1152/ajpregu.00860.2005
Blaber SP, Webster RA, Hill CJ et al (2012) Analysis of in vitro secretion profiles from adipose-derived cell populations. J Transl Med 10:172. https://doi.org/10.1186/1479-5876-10-172
Blagovic K, Kim LY, Voldman J (2011) Microfluidic perfusion for regulating diffusible signaling in stem cells. PLoS One 6:e22892. https://doi.org/10.1371/journal.pone.0022892
Hemmingsen M, Vedel S, Skafte-Pedersen P et al (2013) The role of paracrine and autocrine signaling in the early phase of adipogenic differentiation of adipose-derived stem cells. PLoS One. https://doi.org/10.1371/journal.pone.0063638
Ferland-McCollough D, Masseli D, Spinetti G et al (2018) MCP-1 Feedback Loop Between adipocytes and mesenchymal stromal cells causes fat accumulation and contributes to hematopoietic stem cell rarefaction in the bone marrow of diabetic patients. Diabetes. https://doi.org/10.2337/db18-0044
Younce C, Kolattukudy P (2012) MCP-1 induced protein promotes adipogenesis via oxidative stress, endoplasmic reticulum stress and autophagy. Cell Physiol Biochem Int J Exp Cell Physiol Biochem Pharmacol 30:307–320. https://doi.org/10.1159/000339066
Panee J (2012) Monocyte chemoattractant protein 1 (MCP-1) in obesity and diabetes. Cytokine 60:1–12. https://doi.org/10.1016/j.cyto.2012.06.018
Green H, Meuth M (1974) An established pre-adipose cell line and its differentiation in culture. Cell 3:127–133
Zebisch K, Voigt V, Wabitsch M, Brandsch M (2012) Protocol for effective differentiation of 3T3-L1 cells to adipocytes. Anal Biochem 425:88–90. https://doi.org/10.1016/j.ab.2012.03.005
Huang W-C, Chang W-T, Wu S-J et al (2013) Phloretin and phlorizin promote lipolysis and inhibit inflammation in mouse 3T3-L1 cells and in macrophage-adipocyte co-cultures. Mol Nutr Food Res 57:1803–1813. https://doi.org/10.1002/mnfr.201300001
Lai N, Sims JK, Jeon NL, Lee K (2012) Adipocyte induction of preadipocyte differentiation in a gradient chamber. Tissue Eng Part C Methods 18:958–967. https://doi.org/10.1089/ten.tec.2012.0168
Chang C-C, Chen C-Y, Wen H-C et al (2017) Caveolin-1 secreted from adipose tissues and adipocytes functions as an adipogenesis enhancer. Obesity 25:1932–1940. https://doi.org/10.1002/oby.21970
Wei Y-T, Xia D-S, Yang W-K et al (2014) Secretion of adipocytes and macrophages under conditions of inflammation and/or insulin resistance and effect of adipocytes on preadipocytes under these conditions. Biochem Mosc 79:663–671. https://doi.org/10.1134/S0006297914070086
Bacakova L, Zarubova J, Travnickova M et al (2018) Stem cells: their source, potency and use in regenerative therapies with focus on adipose-derived stem cells—a review. Biotechnol Adv 36:1111–1126. https://doi.org/10.1016/j.biotechadv.2018.03.011
Green H, Kehinde O (1979) Formation of normally differentiated subcutaneous fat pads by an established preadipose cell line. J Cell Physiol 101:169–171
Kimura Y, Ozeki M, Inamoto T, Tabata Y (2003) Adipose tissue engineering based on human preadipocytes combined with gelatin microspheres containing basic fibroblast growth factor. Biomaterials 24:2513–2521. https://doi.org/10.1016/S0142-9612(03)00049-8
Tsuji W, Inamoto T, Yamashiro H et al (2009) Adipogenesis induced by human adipose tissue-derived stem cells. Tissue Eng Part A 15:83–93. https://doi.org/10.1089/ten.tea.2007.0297
Wong JC, Krueger KC, Costa MJ et al (2016) A glucocorticoid- and diet-responsive pathway toggles adipocyte precursor cell activity in vivo. Sci Signal 9:ra103. https://doi.org/10.1126/scisignal.aag0487
Lee M-J, Pramyothin P, Karastergiou K, Fried SK (2014) Deconstructing the roles of glucocorticoids in adipose tissue biology and the development of central obesity. Biochim Biophys Acta 1842:473–481. https://doi.org/10.1016/j.bbadis.2013.05.029
Wu L, Wang T, Ge Y et al (2012) Secreted factors from adipose tissue increase adipogenic differentiation of mesenchymal stem cells. Cell Prolif 45:311–319. https://doi.org/10.1111/j.1365-2184.2012.00823.x
Rinker TE, Hammoudi TM, Kemp ML et al (2014) Interactions between mesenchymal stem cells, adipocytes, and osteoblasts in a 3D tri-culture model of hyperglycemic conditions in the bone marrow microenvironment. Integr Biol Quant Biosci Nano Macro 6:324–337. https://doi.org/10.1039/c3ib40194d
Challa TD, Straub LG, Balaz M et al (2015) Regulation of de novo adipocyte differentiation through cross talk between adipocytes and preadipocytes. Diabetes 64:4075–4087. https://doi.org/10.2337/db14-1932
Schwalie PC, Dong H, Zachara M et al (2018) A stromal cell population that inhibits adipogenesis in mammalian fat depots. Nature 559:103–108. https://doi.org/10.1038/s41586-018-0226-8
Williams GA, Wang Y, Callon KE et al (2009) In vitro and in vivo effects of adiponectin on bone. Endocrinology 150:3603–3610. https://doi.org/10.1210/en.2008-1639
Kudoh A, Satoh H, Hirai H et al (2018) Preliminary evidence for adipocytokine signals in skeletal muscle glucose uptake. Front Endocrinol 9:295. https://doi.org/10.3389/fendo.2018.00295
Seo K, Suzuki T, Kobayashi K, Nishimura T (2018) Adipocytes suppress differentiation of muscle cells in a co-culture system. Anim Sci J Nihon Chikusan Gakkaiho. https://doi.org/10.1111/asj.13145
Maenhaut N, Van de Voorde J (2011) Regulation of vascular tone by adipocytes. BMC Med 9:25. https://doi.org/10.1186/1741-7015-9-25
Huh JY, Park YJ, Ham M, Kim JB (2014) Crosstalk between adipocytes and immune cells in adipose tissue inflammation and metabolic dysregulation in obesity. Mol Cells 37:365–371. https://doi.org/10.14348/molcells.2014.0074
Lim J-M, Sherling D, Teo CF et al (2008) Defining the regulated secreted proteome of rodent adipocytes upon the induction of insulin resistance. J Proteome Res 7:1251–1263. https://doi.org/10.1021/pr7006945
Lehr S, Hartwig S, Lamers D et al (2012) Identification and validation of novel adipokines released from primary human adipocytes. Mol Cell Proteomics MCP 11(M111):010504. https://doi.org/10.1074/mcp.M111.010504
Chen X, Hunt D, Cushman SW, Hess S (2009) Proteomic characterization of thiazolidinedione regulation of obese adipose secretome in Zucker obese rats. Proteomics Clin Appl 3:1099–1111. https://doi.org/10.1002/prca.200900026
Krey G, Braissant O, L’Horset F et al (1997) Fatty acids, eicosanoids, and hypolipidemic agents identified as ligands of peroxisome proliferator-activated receptors by coactivator-dependent receptor ligand assay. Mol Endocrinol Baltim Md 11:779–791. https://doi.org/10.1210/mend.11.6.0007
Hutley LJ, Newell FM, Joyner JM et al (2003) Effects of rosiglitazone and linoleic acid on human preadipocyte differentiation. Eur J Clin Invest 33:574–581
Massiera F, Saint-Marc P, Seydoux J et al (2003) Arachidonic acid and prostacyclin signaling promote adipose tissue development: a human health concern? J Lipid Res 44:271–279. https://doi.org/10.1194/jlr.M200346-JLR200
Mathivanan S, Ji H, Simpson RJ (2010) Exosomes: extracellular organelles important in intercellular communication. J Proteomics 73:1907–1920. https://doi.org/10.1016/j.jprot.2010.06.006
Dai M, Yu M, Zhang Y, Tian W (2017) Exosome-like vesicles derived from adipose tissue provide biochemical cues for adipose tissue regeneration. Tissue Eng Part A 23:1221–1230. https://doi.org/10.1089/ten.tea.2017.0045
Sano S, Izumi Y, Yamaguchi T et al (2014) Lipid synthesis is promoted by hypoxic adipocyte-derived exosomes in 3T3-L1 cells. Biochem Biophys Res Commun 445:327–333. https://doi.org/10.1016/j.bbrc.2014.01.183
Hartwig S, De Filippo E, Göddeke S et al (2018) Exosomal proteins constitute an essential part of the human adipose tissue secretome. Biochim Biophys Acta BBA Proteins Proteom. https://doi.org/10.1016/j.bbapap.2018.11.009
Rui L (2017) Brown and beige adipose tissues in health and disease. In: Terjung R (ed) Comprehensive physiology. Wiley, Hoboken, pp 1281–1306
Scheideler M, Herzig S, Georgiadi A (2017) Endocrine and autocrine/paracrine modulators of brown adipose tissue mass and activity as novel therapeutic strategies against obesity and type 2 diabetes. Horm Mol Biol Clin Investig. https://doi.org/10.1515/hmbci-2017-0043
Ali Khan A, Hansson J, Weber P et al (2018) Comparative secretome analyses of primary murine white and brown adipocytes reveal novel adipokines. Mol Cell Proteom 17:2358–2370. https://doi.org/10.1074/mcp.RA118.000704
Gnad T, Scheibler S, von Kügelgen I et al (2014) Adenosine activates brown adipose tissue and recruits beige adipocytes via A2A receptors. Nature 516:395–399. https://doi.org/10.1038/nature13816
Tseng Y-H, Kokkotou E, Schulz TJ et al (2008) New role of bone morphogenetic protein 7 in brown adipogenesis and energy expenditure. Nature 454:1000–1004. https://doi.org/10.1038/nature07221
Whittle AJ, Carobbio S, Martins L et al (2012) BMP8B increases brown adipose tissue thermogenesis through both central and peripheral actions. Cell 149:871–885. https://doi.org/10.1016/j.cell.2012.02.066
Klepac K, Kilić A, Gnad T et al (2016) The Gq signalling pathway inhibits brown and beige adipose tissue. Nat Commun 7:10895. https://doi.org/10.1038/ncomms10895
Villarroya F, Cereijo R, Villarroya J, Giralt M (2017) Brown adipose tissue as a secretory organ. Nat Rev Endocrinol 13:26–35. https://doi.org/10.1038/nrendo.2016.136
Poulos SP, Dodson MV, Hausman GJ (2010) Cell line models for differentiation: preadipocytes and adipocytes. Exp Biol Med 235:1185–1193. https://doi.org/10.1258/ebm.2010.010063
Chusyd DE, Wang D, Huffman DM, Nagy TR (2016) Relationships between rodent white adipose fat pads and human white adipose fat depots. Front Nutr 3:10. https://doi.org/10.3389/fnut.2016.00010
Steppan CM, Bailey ST, Bhat S et al (2001) The hormone resistin links obesity to diabetes. Nature 409:307–312. https://doi.org/10.1038/35053000
Patel L, Buckels AC, Kinghorn IJ et al (2003) Resistin is expressed in human macrophages and directly regulated by PPAR gamma activators. Biochem Biophys Res Commun 300:472–476. https://doi.org/10.1016/s0006-291x(02)02841-3
Blaszkiewicz M, Willows JW, Johnson CP, Townsend KL (2019) The importance of peripheral nerves in adipose tissue for the regulation of energy balance. Biology. https://doi.org/10.3390/biology8010010
Wang QA, Scherer PE (2014) The AdipoChaser mouse: a model tracking adipogenesis in vivo. Adipocyte 3:146–150. https://doi.org/10.4161/adip.27656
Wolfrum C, Straub LG (2019) Lessons from cre-mice and indicator mice. In: Pfeifer A, Klingenspor M, Herzig S (eds) Brown adipose tissue. Springer International Publishing, Cham, pp 37–54
Rydén M, Uzunel M, Hård JL et al (2015) Transplanted bone marrow-derived cells contribute to human adipogenesis. Cell Metab 22:408–417. https://doi.org/10.1016/j.cmet.2015.06.011
Arner E, Westermark PO, Spalding KL et al (2010) Adipocyte turnover: relevance to human adipose tissue morphology. Diabetes 59:105–109. https://doi.org/10.2337/db09-0942
Acknowledgements
This work is based on the research supported wholly/in part by the National Research Foundation of South Africa (Grant Numbers 118565 and 118990), the South African Sugar Association (Project 257) and The Harry Crossley Foundation; WLH is supported by the Faculty of Medicine and Health Sciences, Stellenbosch University, South Africa.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haylett, W.L., Ferris, W.F. Adipocyte–progenitor cell communication that influences adipogenesis. Cell. Mol. Life Sci. 77, 115–128 (2020). https://doi.org/10.1007/s00018-019-03256-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-019-03256-5