Abstract
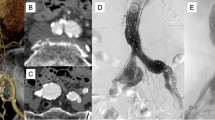
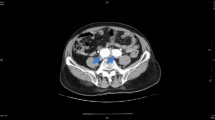
Revascularization of the hypogastric artery often tends to be neglected in aortoiliac reconstructive surgery; however, its incomplete revascularization can result in unfavorable complications such as buttock claudication or necrosis, vascular impotence, and colonic ischemia. Multiple vascular lesions in the abdominal aorta and bilateral iliac arteries were reconstructed using a newly designed double bifurcated graft in five male patients. All five patients demonstrated excellent graft limb patency and postoperative improvement of the ankle-brachial pressure index without any clinical signs of ischemia in regions of the hypogastric artery. Thus, we conclude that an aggressive approach toward hypogastric circulation maintenance is essential in aortoiliac reconstructive surgery. By using this double bifurcated graft, rapid and safe revascularization of the bilateral hypogastric arteries concomitant with the external iliac or femoral arteries can be performed.
Similar content being viewed by others
References
Hodgson KJ, Summer DS (1988) Buttock claudication from isolated bilateral internal iliac arterial stenoses. J Vasc Surg 7:446–448
Virag R, Bouilly P, Frydman D (1985) Is impotence an arterial disorder? A study of arterial risk factors in 440 impotent men. Lancet 1:181–184
Seagraves A, Rutherford RB (1987) Isolated hypogastric artery revascularization after previous bypass for aortoiliac occlusive disease. J Vasc Surg 5:472–474
Queral LA, Whitehouse WM Jr, Flinn WR, Zarins CK, Bergan JJ, Yao JST (1979) Pelvic hemodynamics after aortoiliac reconstruction. Surgery 86:799–809
Lose G, Jørgensen L, Lorentzen JE (1985) Regional ischemia due to compromised collateral circulation after arterial reconstruction. Acta Chir Scand 151:301–303
Picone AL, Green RM, Ricotta JR, May AG, Deweese JA (1986) Spinal cord ischemia following operations on the abdominal aorta. J Vasc Surg 3:94–103
Jablecki CK, Aguilo JJ, Piepgras DG, Zincke H, Goldstein NP (1977) Paraparesis after renal transplantation. Ann Neurol 2:154–155
Bernatz PE (1960) Necrosis of the colon following resection for abdominal aortic aneurysms. Arch Surg 81:373–378
Andriole GL, Sugarbaker PH (1985) Perineal and bladder necrosis following bilateral internal iliac artery ligation. Report of a case. Dis Colon Rectum 28:183–184
Merkel FK, Najarian JS (1971) Rest pain of the buttock after aortofemoral bypass procedure. Report of an unusual case. Am J Surg 121:617–619
Cronenwett JL, Gooch JB, Garrett HE (1982) Internal iliac artery revascularization during aortofemoral bypass. Arch Surg 117:838–839
Iliopoulos JI, Howanitz PE, Pierce GE, Kueshkerian SM, Thomas JH, Hermreck AS (1987) The critical hypogastric circulation. Am J Surg 154:671–675
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Akiyama, K., Takazawa, A., Hirota, J. et al. A double bifurcated graft for abdominal aorta and bilateral iliac artery reconstruction. Surg Today 29, 313–316 (1999). https://doi.org/10.1007/BF02483054
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02483054