Summary
Objectives
Falls among elderly are a well-recognised public health problem. The purpose of the present study was to explore the relation between dementia, number of depressive symptoms, activities of daily living, setting, and risk of falling.
Methods
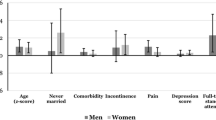
Data for the analysis came from a cross-sectional study about dementia, depression, and disabilities, carried out 1995/96 in Zurich and Geneva. The random sample stratified, by age and gender consisted of 921 subjects aged 65 and more. The interview was conducted by means of the Canberra Interview for the Elderly, extended by short questionnaire. The subject was classified as a faller if the subject and/or the informant had reported a fall within the last 12 months prior to the interview. Logistic-regression analysis was used to determine the independent impact of dementia, depressive symptoms, and ADL-score on risk of falling.
Results
The stepwise logistic regression analysis has revealed a statistically significant association between dementia (OR 2.14, 95% Cl 1.15–3.96), two resp. three depressive symptoms (OR 1.64, 95% Cl 1.04–2.60) as well as four or more depressive symptoms (OR 2.64, 95% Cl 1.39–5.02) and the risk of falling. There was no statistically significant relationship between studied risk factors and the risk of being one-time faller. However, we found a strong positive association between dementia (OR 3.92, 95% Cl 1.75–8.79), four or more depressive symptoms (OR 3.90, 95% Cl 1.55–9.83) and the risk of being recurrent faller. Moreover, residents of nursing homes (OR 8.50, 95% Cl 2.18–33.22) and elderly aged 85 or more (OR 2.29, 95% Cl 1.08–4.87) were under statistically significant higher risk of sustaining recurrent falls.
Conclusions
The results of the present study confirm that dementia and depression substantially increase the risk of falling.
Zusammenfassung
Fragestellung
Stürze bei Betagten werden als bedeutendes Public-Health-Problem anerkannt. Im Mittelpunkt der Studie steht das Ziel, anhand eines repräsentativen Kollektivs von Betagten der Städte Zürich und Genf die Beziehungen zwischen Demenz, Anzahl der depressiven Symptome, Aktivitätten des täglichen Lebens sowie der Wohnsituation und dem Sturzrisiko zu eruieren.
Methoden
Ausgangspunkt der Analysen waren Daten aus einer Querschnittsstudie über Demenz, Depressionen und Behinderungen im Alter, die 1995/96 in Zürich und Genf durchgeführt wurde. Die nach Alter und Geschlecht geschichtete Stichprobe bestand aus 921 Probanden. Bei der Befragung wurde das Canberra Interview for the Elderly (CIE) verwendet, ergänzt durch einen kurzen Fragebogen. Ein Proband wurde als Gestürzter klassifiziert, wenn er und/oder der jeweilige Informant einen Sturz innerhalb der letzten 12 Monate angab. Die statistischen Auswertungen erfolgten mittels der multivariaten logistischen Regressionsanalyse.
Ergebnisse
Die Analysen zeigen eine statistisch signifikante Assoziation zwischen Demenz (OR 2,14; 95%-KI 1,15–3,96), zwei bzw. drei depressiven Symptomen (OR 1,64; 95%-KI 1,04–2,60) sowie vier oder mehr depressiven Symptomen (OR 2,64; 95%-KI 1,39–5,02) und dem Sturzrisiko. Es ergeben sich einerseits keine signifikante Relationen zwischen Demenz, Anzahl der depressiven Symptome sowie ADL und einmaligem Sturz. Anderseits besteht in der schrittweisen logistischen Analyse eine starke statistisch signifikante positive Assoziation zwischen Demenz (OR 3,92; 95%-KI 1,75–8,79), vier oder mehr depressiven Symptomen (OR 3,90; 95%-Kl 1,55–9,83) und rezidivierenden Stürzen. Bewohner der Pflegeheime (OR 8,50; 95%-Kl 2,18–33,22) und Betagte über 85 Jahre alt (OR 2,29; 95%-Kl 1,08–4,87) haben ein erhöhtes Risiko, rezidivierende Stürze zu erleiden.
Schlussfolgerungen
Die Resultate der Studie bestätigen, dass Demenz und Depressionen das Sturzrisiko bei Betagten wesentlich zu erhöhen vermögen.
Résumé
Objectifs
Les chutes parmi âgé sont un problème de santé publique bien reconnu. Le but de l'étude présente était d'explorer la relation entre la démence, le numéro de symptômes dépressifs, les activités de vie quotidienne, l'arrangement et le risque de chute.
Méthodes
Les données pour l'analyse sont venues d'une étude mutuelle-à éléments de la démence, la dépression et des handicaps, effectués 1995/96 à Zurich et Genève. Un échantillon aléatoire stratifié, à l'âge et le genre a consisté en 921 sujets âgé 65 et plus. L'interview a été conduit au moyen de Canberra l'Interview pour l'Âgé, prolongé par le questionnaire court. Le sujet a été classifié comme un chuteur si le sujet et-ou l'informateur avaient annoncé une chute dans les 12 derniers mois avant l'interview. L'analyse de régressions logistiques multiple a été employée pour déterminer l'impact indépendant de démence, des symptômes dépressifs et l'ADL-score en risque de chute.
Résultats
L'analyse de régression point par point logistique a révélé l'association statistiquement significative entre la démence (OU 2,14; 95% CI 1,15–3,96), deux resp. trois symptômes dépressifs (OU 1,64; 95% CI 1,04–2,60) aussi bien que quatre symptômes ou plus dépressifs (OU 2,64; 95% CI 1,39–5,02) et le risque de chute. Il n'y avait pas statistiquement le rapport significatif entre des facteurs de risque étudiés et le risque d'être le chuteur jetable. Cependant, nous avons découvert une association forte positive entre la démence (OU 3,92; 95% CI 1,75–8,79), quatre symptômes ou plus dépressifs (OU 3,90; 95% CI 1,55–9,83) et le risque d'être le chuteur récurrent. De plus, les résidants de maisons de repos (OU 8,50; 95% CI 2,18–33,22) et âgé 85 ou plus (OU 2,29; 95% CI 1,08–4,87) étaient statistiquement significatifs plus haut le risque de supporter des chutes récurrentes.
Conclusions
Les résultats de l'étude présente ont confirmé que la démence et la dépression augmentent considérablement le risque de chute.
Similar content being viewed by others
Literaturverzeichnis
Sattin RW. Falls among older persons: a public health perspective. Annu Rev Public Health 1992;13:489–508.
Kannus P, Parkkari J, Koskinen S, et al. Fall-induced injuries and deaths among older adults. JAMA 1999;281:1895–9.
Hill K, Schwarz J, Flicker L, et al. Falls among healthy, community-dwelling, older women: a prospective study of frequency, circumstances, consequences and prediction accuracy. Aust N Z J Public Health 1999;23: 41–8.
Morris JC, Rubin EH, Morris EJ, et al. Senile dementia of the Alzheimer's type: an important risk factor for serious falls. J Gerontol 1987;42:412–7.
Van Dijk PTM, Meulenberg OGRM, van de Sande HJ, et al. Falls in dementia patients. Gerontologist 1993;33:200–4.
Oleske DM, Wilson RS, Bernard BA, et al. Epidemiology of injury in people with Alzheimer's disease. J Am Geriatr Soc 1995;43: 741–6.
Asada T, Kariya T, Kinoshita T, et al. Predictors of fall-related injuries among community-dwelling elderly people with dementia. Age Ageing 1996;25:22–8.
Buchner DM, Larson EB. Falls and fractures in patients with Alzheimer-type dementia. JAMA 1987;257:1492–5.
Brody EM, Kleban MH, Moss MS, et al. Predictors of falls among institutionalized women with Alzheimer's disease. J Am Geriatr Soc 1984;32:877–82.
Thapa PB, Gideon P, Fought RL, et al. Psychotropic drugs and risk of recurrent falls in ambulatory nursing home residents. Am J Epidemiol 1995; 142: 202–11.
Granek E, Baker SP, Abbey H, et al. Medications and diagnoses in relation to falls in a long-term care facility. J Am Geriatr Soc 1987;35:503–11.
Nevitt MC, Cummings SR, Kidd S, et al. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 1989;261: 2663–8.
Whooley M, Kevin E, Cauley J, et al. Depression, falls, and risk of fracture in older women. Arch Intern Med 1999;159: 484–90.
Myers AH, Young Y, Langlois JA. Prevention of falls in the elderly. Bone 1996;18 (1 Suppl): 87S-101S.
Chan KM, Pang WS, Ee CH, et al. Epidemiology of falls among the elderly community dwellers in Singapore. Singapore Med J 1997;38:427–31.
Stevens JA, Powell KE, Smith SM, et al. Physical activity, functional limitations, and the risk of fall-related fractures in community-dwelling elderly. Ann Epidemiol 1997;7:54–61.
Close J, Ellis M, Hooper R, et al. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet 1999;353: 93–7.
Gostynski M, Ajdacic-Gross V, Gutzwiller F, et al. Epidemiologische Analyse der Stürze bei Betagten in Zürich und Genf. Schweiz Med Wochenschr 1999;129:270–5.
The Canberra Interview for the Elderly: a new field instrument for the diagnosis of dementia and depression by ICD-10 and DSM-III-R. Social Psychiatry Research Unit. Acta Psychiatr Scand 1992;85:105–13.
Jorm A, Mackinnon A, Henderson A, et al. The Psychogeriatric Assessment Scales: a multi-dimensional alternative to categorical diagnosis of dementia and depression in the elderly. Canberra: Social Psychiatry Research Unit, The Australian National University, 1993.
Mahoney F, Barthel D. Functional evaluation: the Barthel index. Md State Med J 1965;14:61–5.
Kellog International Work Group on the Prevention of Falls by the Elderly. The prevention of falls in later life. Dan Med Bull 1987;34 (Suppl 4): 1–24.
SPSS User's Guide. Chicago, IL: SPSS, 1989.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988;319: 1701–7.
Shaw FE, Richardson DA, Bond J, et al. Social and clinical characteristics of patients with dementia and cognitive impairment attending a casualty department with falls. Lancet Conference “The Challenge of the Dementias”. Edinburgh, UK, April 1996 (unpubl.).
Mossey JM. Social and psychologic factors related to falls among the elderly. Clin Geriatr Med 1985;1:541–53.
Cumming RG, Miller PJ, Kelsey JL, et al. Medications and multiple falls in elderly people: The St Louis OASIS study. Age Ageing 1991;20:455–60.
Weiner MF, Risser RC, Cullum CM, et al. Alzheimer's disease and its Lewy body variant: a clinical analysis of postmortem verified cases. Am J Psychiatry 1996;153:1269–73.
Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 1999;47:30–9.
Stäubli M. Iatrogenic falls. Schweiz Med Wochenschr 1996;126:576–83.
Weyerer S, Schäufele M. Psychotropic drugs and accidental falls in the elderly. Fortschr Med 1998;116:29–31.
Tinetti ME, Williams F, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med 1986;80:429–34.
Ray W. Psychotropic drugs and injuries among the elderly: a review. J Clin Psychopharmacol 1992;12:386–96.
Glassman A, Bigger JJ. Cardiovascular effects of therapeutic doses of tricyclic antidepressants: a review. Arch Gen Psychiatry 1981;38:815–20.
Glassman A, Walsh B, Roose S, et al. Factors related to orthostatic hypotension associated with tricyclic antidepressants. J Clin Psychopharmacol 1982;43:35–8.
Manone M, Avorn J. Medications and falls, correlation, and prevention. Clin Geriat Med 1996;12:847–58.
Myers AH, Baker SP, Van NM, et al. Risk factors associated with falls and injuries among elderly institutionalized persons. Am J Epidemiol 1991;133:1179–90.
Liu B, Anderson G, Mittmann N, et al. Use of selective serotonin-reuptake inhibitors or tricyclic antidepressants and risk of hip fractures in elderly people. Lancet 1998;351: 1303–7.
Cumming RG. Epidemiology of medication-related falls and fractures in the elderly. Drugs Aging 1998;12:43–53.
Mustard CA. Case-control study of exposure to medication and risk of injurious falls requiring hospitalization among nursing home residents. Am J Epidemiol 1997;145:738–45.
Dealberto M, Seeman T, McAvay G, et al. Factors related to current and subsequent psychotropic drug use in an elderly cohort. J Clin Epidemiol 1997;50:357–64.
Ray WA, Griffin MR, Schaffner W, et al. Psychotropic drug use and the risk of hip fracture. N Engl J Med 1987;316:363–9.
Gialloreti LE, Marazzi MC. Risk for falls in the elderly. Role of activities of daily living and of the subjective assessment of health status. A case-control study. Recent Prog Med 1996;87:405–11.
Palmore E, Cleveland W. Aging, terminal decline, and terminal drop. J Gerontol 1976;33:76–81.
Gryfe CI, Amies A, Ashley MJ. A longitudinal study of falls in an elderly population: I. Incidence and Morbidity. Age Ageing 1977;6:201–10.
Gostynski M. Falls among the elderly. Lancet 1991;337:8735.
Wild D, Nayak U, Isaacs B. Prognosis of falls in old people at home. J Epidemiol Community Health 1981;35:200–4.
Tinetti ME, Speechley M. Prevention of falls among the elderly. N Engl J Med 1989;320:1055–59.
O'Loughlin JL, Robitaille Y, Boivin JF. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 1993;137:342–54.
Graafmans WC, Ooms ME, Hofstee HM, et al. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol 1996;143:1129–36.
Sattin RW, Rodriguez JG, DeVito CA, et al. Home environmental hazards and the risk of fall injury events among community-dwelling older persons: Study to Assess Falls among the Elderly (SAFE) Group. J Am Geriatr Soc 1998;46: 669–76.
Wettstein A. Sturz als Nebenwirkung von Medikamenten. Schweiz Rundschau Med Prax 1992;81:1383–6.
Cummings SR, Nevitt MC, Kidd S. Forgetting falls: the limited accuracy of recall of falls in the elderly. J Am Geriatr Soc 1988;36:613–6.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gostynski, M., Ajdacic-Gross, V., Heusser-Gretler, R. et al. Demenz, Depressionen und Aktivitäten des täglichen Lebens als Risikofaktoren von Stürzen bei Betagten. Soz Präventivmed 46, 123–130 (2001). https://doi.org/10.1007/BF01299729
Issue Date:
DOI: https://doi.org/10.1007/BF01299729