Abstract
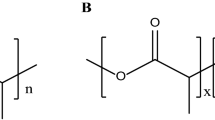
Extended release of immunosuppressive drugs and sustained drug levels are desirable for the treatment of corneal graft rejection and other ocular immune disorders. This experiment was conducted with biodegradable microspheres containing cyclosporine A to assess their suitability for achieving this goal. Microspheres containing cyclosporine A were prepared using a solvent evaporation process. A mixture of poly (lactic) and poly(glycolic) acid polymers (50: 50) and cyclosporine A was dissolved in a mixture of chloroform and acetone. The solution was then emulsified in an aqueous solution of polyvinyl alcohol and stirred for 24 hours to evaporate the organic solvent. The final assayed concentration of cyclosporine A was 15.38 mg/mL. A 0.13 mL aliquot (2.0 mg) of the suspension of the microspheres was injected subconjunctivally in 24 eyes of white New Zealand rabbits. The concentration of cyclosporine A in the aqueous and cornea was measured at 6, 12, 24, 48, 72, and 144 hours after injection (n=4 for each group). Corneal levels of cyclosporine A ranged from 2392±70 ng/mL at 6 hours to 1297±459 ng/mL at 144 hours. The aqueous levels ranged from 110±0 ng/mL at 6 hours to 62±11 ng/mL at 144 hours. These data indicate that a microsphere drug delivery system is an effective means of delivering cyclosporine A to the cornea and anterior chamber, and may provide an alternative for the treatment of ocular immune disorders.
Similar content being viewed by others
References
BenEzra D, Matamoros N, Cohen E. Treatment of severe vernal keratoconjunctivitis with cyclosporine A eyedrops. Transplant Proc 1988; 20 (Suppl 2, No 2): 644–9.
Hoffmann F, Wiederholt M. Local treatment of necrotizing scleritis with cyclosporin A. Cornea 1985; 4: 3–7.
Holland EJ, Chan CC, Kuwabara T, Palestine AG, Rowsey JJ, Nussenblatt RB. Immunohistologic findings and results of treatment with cyclosporine in ligneous conjunctivitis. Am J Ophthalmol 1989; 107: 160–6.
Nussenblatt RB, Palestine AG, Chan CC, Mochizuki M, Yancey K. Effectiveness of cyclosporin therapy for BehÇet's disease. Arthritis Rheum 1985; 28: 671–9.
Chen YF, Gebhardt BM, Reidy JJ, Kaufman HE. Cyclosporinecontaining collagen shields suppress corneal allograft rejection. Am J Ophthalmol 1990; 109: 132–7.
Bell TAG, Easty DL, McCullagh KG. A placebo-controlled blind trial of cyclosporin-A in prevention of corneal graft rejection in rabbits. Br J Ophthalmol 1982; 66: 303–8.
Foets B, Missotten L, Vanderveeren P, Goossens W. Prolonged survival of allogeneic corneal grafts in rabbits treated with topically applied cyclosporin A: systemic absorption and local immunosuppressive effect. Br J Ophthalmol 1985; 69: 600–3.
Newton C, Gebhardt BM, Kaufman HE. Topically applied cyclosporine in azone prolongs corneal allograft survival. Invest Ophthalmol Vis Sci 1988; 29: 208–15.
Salisbury JD, Gebhardt BM. Suppression of corneal allograft rejection by cyclosporin A. Arch Ophthalmol 1981; 99: 1640–3.
Kalsi GS, Gudauskas G, Bussanich N, Freeman DJ, Rootman J. Ocular pharmacokinetics of subconjunctivally administered cyclosporine in the rabbit. Can J Ophthalmol 1991; 26: 200–5.
Mosteller MW, Gebhardt BM, Hamilton AM, Kaufman HE. Penetration of topical cyclosporine into the rabbit cornea, aqueous humor, and serum. Arch Ophthalmol 1985; 103: 101–2.
Wood DA. Biodegradable drug delivery systems. Int J Pharmaceut 1980;7: 1–18.
Kulkarni RK, Pani KC, Neuman C, Leonard F. Polylactic acid for surgical implants. Arch Surg 1966; 93: 839–43.
Kulkarni RK, Moore EG, Hegyeli AF, Leonard F. Biodegradable poly (lactic acid) polymers. J Biomed Mater Res 1971; 5: 169–81.
Khoobehi B, Stradtmann MO, Peyman GA, Aly OM. Clearance of sodium fluorescein incorporated into microspheres from the vitreous after intravitreal injection. Ophthalmic Surg 1991; 22: 175–80.
Khoobehi B, Stradtmann MO, Peyman GA, Aly OM. Clearance of fluorescein incorporated into microspheres from the cornea and aqueous after subconjunctival injection. Ophthalmic Surg 1990; 21: 840–4.
Reidy JJ, Gebhardt BM, Kaufman HE. The collagen shield: a new vehicle for delivery of cyclosporin A to the eye. Cornea 1990; 9: 196–9.
Author information
Authors and Affiliations
Additional information
Supported in part by U.S. Public Health Service grants EY07541 and EY02377 from the National Eye Institute, National Institutes of Health, Bethesda, MD, USA.
Rights and permissions
About this article
Cite this article
Harper, C.A., Khoobehi, B., Peyman, G.A. et al. Bioavailability of microsphere-entrapped cyclosporine A in the cornea and aqueous of rabbits. Int Ophthalmol 17, 337–340 (1993). https://doi.org/10.1007/BF00915740
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00915740