Abstract
Osteoporosis is now increasingly recognized in children due to the increased prevalence of disorders associated with bone loss. Fragility fractures represent the cardinal clinical features of pediatric osteoporosis and children presenting with fragility fractures deserve an accurate assessment to rule out a secondary cause. Indeed, in the pediatric population, a low bone mass is often a consequence of a chronic disease or its treatment; genetic bone disorders represent the cause of only a small fraction of cases. The position statement of the International Society for Clinical Densitometry guides physicians in interpreting densitometric data and making diagnoses of osteoporosis in children. Once a diagnosis of osteoporosis has been made, the aim is to identify children in whom bone status may deteriorate if left untreated. To date, bisphosphonates have represented the mainstay of treatment for pediatric osteoporosis. However, due to the peculiar pathophysiology of osteoporosis in this age group, a pharmacological agent with an anabolic effect on bone may provide clinicians with other therapeutic options in children. Multicenter studies are needed to optimize treatments and define optimal clinical response in treated children.

Similar content being viewed by others
References
Alos N, et al. High incidence of vertebral fractures in children with acute lymphoblastic leukemia 12 months after the initiation of therapy. J Clin Oncol. 2012;30(22):2760–7.
Mok CC, Wong SN, Ma KM. Childhood-onset disease carries a higher risk of low bone mineral density in an adult population of systemic lupus erythematosus. Rheumatology. 2012;51(3):468–75.
Bailey DA, Mckay HA, Mirwald RL, Faulkner RA. A six-year longitudinal study of the relationship of physical activity to bone mineral accrual in growing children: The University of Saskatchewan Bone Mineral. 1999;14(10):1672–9.
Rizzoli R, Bianchi ML, Garabédian M, McKay HA, Moreno LA. Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone. 2010;46(2):294–305.
Christoffersen T, Ahmed LA, Winther A, et al. Fracture incidence rates in Norwegian children, The Tromsø Study, fit futures. Arch Osteoporos. 2016;11(1):40.
Leaman LA, Hennrikus WL, Bresnahan JJ. Identifying non-accidental fractures in children aged <2 years. J Child Orthop. 2016;10(4):335–41.
Paddock M, Sprigg A, Offiah AC. Imaging and reporting considerations for suspected physical abuse (non-accidental injury) in infants and young children. Part 2: axial skeleton and differential diagnoses. Clin Radiol. 2017;72(3):189–201. doi:10.1016/j.crad.2016.11.015.
Krug EG, Dahlberg LL, Mercy JA, Zwi AB. World report on violence and health. Lancet. 2002;360(9339):1083–8.
Marini JC, Blissett AR. New genes in bone development: what’s new in osteogenesis imperfecta. J Clin Endocrinol Metab. 2013;98(8):3095–103.
Lindahl K, Åström E, Rubin CJ, et al. Genetic epidemiology, prevalence, and genotype–phenotype correlations in the Swedish population with osteogenesis imperfecta. Eur J Hum Genet. 2015;23(8):1042–50.
Zacharin M, Cundy T. Osteoporosis pseudoglioma syndrome: treatment of spinal osteoporosis with intravenous bisphosphonates. J Pediatr. 2000;137(3):410–5.
Bacchetta J, Wesseling-Perry K, Gilsanz V, Gales B, Pereira RC, Salusky IB. Idiopathic juvenile osteoporosis: a cross-sectional single-centre experience with bone histomorphometry and quantitative computed tomography. Pediatr Rheumatol. 2013;11(1):6.
Dent CE, Friedman M. Idiopathic juvenile osteoporosis. Q J Med. 1965;34:177–210.
Mäkitie RE, et al. Skeletal characteristics of WNT1 osteoporosis in children and young adults. J Bone Miner Res. 2016;31(9):1734–42.
Bishop N, et al. Dual-energy X-ray aborptiometry assessment in children and adolescents with diseases that may affect the skeleton: the 2007 ISCD pediatric official positions. J Clin Densitom. 2008;11(1):29–42.
Buckner JL, Bowden SA, Mahan JD. Optimizing bone health in duchenne muscular dystrophy. Int J Endocrinol. 2015;2015:928385.
Joseph S, McCarrison S, Wong SC. Skeletal fragility in children with chronic disease. Horm Res Paediatr. 2016;86(2):71–82.
Boyce BF, Schwarz EM, Xing L. Osteoclast precursors: cytokine-stimulated immunomodulators of inflammatory bone disease. Curr Opin Rheumatol. 2006;18(4):427–32.
Devlin RD, Reddy SV, Savino R, Ciliberto G, Roodman GD. IL-6 mediates the effects of IL-1 or TNF, but not PTHrP or 1,25(OH)2D3, on osteoclast-like cell formation in normal human bone marrow cultures. J Bone Miner Res. 1998;13(3):393–9.
Huber AM, Ward LM. The impact of underlying disease on fracture risk and bone mineral density in children with rheumatic disorders: a review of current literature. Semin Arthritis Rheum. 2016;46(1):49–63.
Huber AM, et al. Prevalent vertebral fractures among children initiating glucocorticoid therapy for the treatment of rheumatic disorders. Arthritis Care Res (Hoboken). 2010;62(4):516–26.
Stagi S, et al. Bone mass and quality in patients with juvenile idiopathic arthritis: longitudinal evaluation of bone-mass determinants by using dual-energy X-ray absorptiometry, peripheral quantitative computed tomography, and quantitative ultrasonography. Arthritis Res Ther. 2014;16(2):R83.
Sylvester FA, et al. Natural history of bone metabolism and bone mineral density in children with inflammatory bowel disease. Inflamm Bowel Dis. 2007;13(1):42–50.
Gokhale R, Favus MJ, Karrison T, Sutton MM, Rich B, Kirschner BS. Bone mineral density assessment in children with inflammatory bowel disease. Gastroenterology. 1998;114(5):902–11.
Boot AM, Bouquet J, Krenning EP, de Muinck Keizer-Schrama SM. Bone mineral density and nutritional status in children with chronic inflammatory bowel disease. Gut. 1998;42(2):188–94.
Burnham JM, et al. Whole body BMC in pediatric crohn disease: independent effects of altered growth, maturation, and body composition. J Bone Miner Res. 2004;19(12):1961–8.
Bernstein CN, Blanchard JF, Leslie W, Wajda A, Yu BN. The incidence of fracture among patients with inflammatory bowel disease. A population-based cohort study. Ann Intern Med. 2000;133(10):795–9.
Semeao EJ, Stallings VA, Peck SN, Piccoli DA. Vertebral compression fractures in pediatric patients with Crohn’s disease. Gastroenterology. 1997;112(5):1710–3.
Ward LM, Rauch F, Matzinger MA, Benchimol EI, Boland M, Mack DR. Iliac bone histomorphometry in children with newly diagnosed inflammatory bowel disease. Osteoporos Int. 2010;21(2):331–7.
Canalis E, Mazziotti G, Giustina A, Bilezikian JP. Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int. 2007;18(10):1319–28.
Pereira RM, Delany AM, Canalis E. Cortisol inhibits the differentiation and apoptosis of osteoblasts in culture. Bone. 2001;28(5):484–90.
Delany AM, Gabbitas BY, Canalis E. Cortisol downregulates osteoblast alpha 1 (I) procollagen mRNA by transcriptional and posttranscriptional mechanisms. J Cell Biochem. 1995;57(3):488–94.
Weinstein RS, et al. Promotion of osteoclast survival and antagonism of bisphosphonate-induced osteoclast apoptosis by glucocorticoids. J Clin Invest. 2002;109(8):1041–8.
Umławska W, Prusek-Dudkiewicz A. Growth retardation and delayed puberty in children and adolescents with juvenile idiopathic arthritis. Arch Med Sci. 2010;1(1):19–23.
Wang S-J, Yang Y-H, Lin Y-T, Yang C-M, Chiang B-L. Attained adult height in juvenile rheumatoid arthritis with or without corticosteroid treatment. Clin Rheumatol. 2002;21(5):363–8.
Rüegsegger P, Medici TC, Anliker M. Corticosteroid-induced bone loss. A longitudinal study of alternate day therapy in patients with bronchial asthma using quantitative computed tomography. Eur J Clin Pharmacol. 1983;25(5):615–20.
Hansen KE, Kleker B, Safdar N, Bartels CM. A systematic review and meta-analysis of glucocorticoid-induced osteoporosis in children. Semin Arthritis Rheum. 2014;44(1):47–54.
Rodd C, et al. Incident vertebral fractures among children with rheumatic disorders 12 months after glucocorticoid initiation: a national observational study. Arthritis Care Res. (Hoboken). 2012;64(1):122–31.
LeBlanc CM, et al. Incident vertebral fractures and risk factors in the first three years following glucocorticoid initiation among pediatric patients with rheumatic disorders. J Bone Miner Res. 2015;30(9):1667–75.
van Staa T, Cooper C, Leufkens H, Bishop N. Children and the risk of fractures caused by oral corticosteroids. J Bone Miner Res. 2003;18(5):913–8.
Feber J, et al. Skeletal findings in children recently initiating glucocorticoids for the treatment of nephrotic syndrome. Osteoporos Int. 2012;23(2):751–60.
Mul D, van Suijlekom-Smit LWA, ten Cate R, Bekkering WP, de Muinck Keizer-Schrama SMPF. Bone mineral density and body composition and influencing factors in children with rheumatic diseases treated with corticosteroids. J Pediatr Endocrinol Metab. 2002;15(2):187–92.
Burnham JM, Shults J, Sembhi H, Zemel BS, Leonard MB. The dysfunctional muscle-bone unit in juvenile idiopathic arthritis. J Musculoskelet Neuronal Interact. 2006;6(4):351–2.
Roth J, Palm C, Scheunemann I, Ranke MB, Schweizer R, Dannecker GE. Musculoskeletal abnormalities of the forearm in patients with juvenile idiopathic arthritis relate mainly to bone geometry. Arthritis Rheum. 2004;50(4):1277–85.
Fehlings D, et al. Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: a systematic review. Dev Med Child Neurol. 2012;54(2):106–16.
Gordon CM, Leonard MB, Zemel BS. 2013 Pediatric position development conference: executive summary and reflections. J Clin Densitom. 2014;17(2):219–24.
Bachrach LK, Gordon CM, Section on Endocrinology. Bone densitometry in children and adolescents. Pediatrics. 2016;138(4):e20162398. doi:10.1542/peds.2016-2398.
Kocks J, Ward K, Mughal Z, Moncayo R, Adams J, Högler W. Z-score comparability of bone mineral density reference databases for children. J Clin Endocrinol Metab. 2010;95(10):4652–9.
Bechtold S, Ripperger P, Dalla Pozza R, Schmidt H, Häfner R, Schwarz HP. Musculoskeletal and functional muscle-bone analysis in children with rheumatic disease using peripheral quantitative computed tomography. Osteoporos Int. 2005;16(7):757–63.
Stagi S, et al. Peripheral quantitative computed tomography (pQCT) for the assessment of bone strength in most of bone affecting conditions in developmental age: a review. Ital J Pediatr. 2016;42(1):88.
Cheung AM, et al. High-resolution peripheral quantitative computed tomography for the assessment of bone strength and structure: a review by the Canadian Bone Strength Working Group. Curr Osteoporos Rep. 2013;11(2):136–46.
Adams JE, Engelke K, Zemel BS, Ward KA, International Society of Clinical Densitometry. Quantitative computer tomography in children and adolescents: the 2013 ISCD pediatric official positions. J Clin Densitom. 2014;17(2):258–74.
Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 2009;8(9):1137–48.
DiVasta AD, Feldman HA, Gordon CM. Vertebral fracture assessment in adolescents and young women with anorexia nervosa: a case series. J Clin Densitom. 2014;17(1):207–11.
Lentle B, et al. The radiology of vertebral fractures in childhood osteoporosis related to glucocorticoid administration. J Clin Densitom. 2016;19(1):81–8.
Ward LM, Konji VN, Ma J. The management of osteoporosis in children. Osteoporos Int. 2016;27(7):2147–79.
Cooper C, Westlake S, Harvey N, Javaid K, Dennison E, Hanson M. Review: developmental origins of osteoporotic fracture. Osteoporos Int. 2006;17(3):337–47.
Simonini G, Giani T, Stagi S, de Martino M, Falcini F. Bone status over 1 yr of etanercept treatment in juvenile idiopathic arthritis. Rheumatology (Oxford). 2005;44(6):777–80.
Billiau AD, et al. Etanercept improves linear growth and bone mass acquisition in MTX-resistant polyarticular-course juvenile idiopathic arthritis. Rheumatology. 2010;49(8):1550–8.
Soo J, et al. Use of exclusive enteral nutrition is just as effective as corticosteroids in newly diagnosed pediatric Crohn’s disease. Dig Dis Sci. 2013;58(12):3584–91.
Werkstetter KJ, Schatz SB, Alberer M, Filipiak-Pittroff B, Koletzko S. Influence of exclusive enteral nutrition therapy on bone density and geometry in newly diagnosed pediatric Crohn’s disease patients. Ann Nutr Metab. 2013;63(1–2):10–6.
Behringer M, Gruetzner S, McCourt M, Mester J. Effects of weight-bearing activities on bone mineral content and density in children and adolescents: a meta-analysis. J Bone Miner Res. 2014;29(2):467–78.
Omori CH, Silva CA, Sallum AM, et al. Exercise training in juvenile dermatomyositis. Arthritis Care Res (Hoboken). 2012;64(8):1186–94.
Gannotti ME, et al. Can exercise influence low bone mineral density in children with juvenile rheumatoid arthritis? Pediatr Phys Ther. 2007;19(2):128–39.
Benchimol EI, et al. Effect of calcium and vitamin d supplementation on bone mineral density in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2007;45(5):538–45.
Winzenberg T, Powell S, Shaw KA, Jones G. Effects of vitamin D supplementation on bone density in healthy children: systematic review and meta-analysis. BMJ. 2011;342(1):c7254–c7254.
Edouard T, Glorieux FH, Rauch F. Predictors and correlates of vitamin D status in children and adolescents with osteogenesis imperfecta. J Clin Endocrinol Metab. 2011;96(10):3193–8.
Winzenberg T, Shaw K, Fryer J, Jones G. Effects of calcium supplementation on bone density in healthy children: meta-analysis of randomised controlled trials. BMJ. 2006;333(7572):775.
di N. Umana SI. Livelli di Assunzione di Riferimento di Nutrienti ed energia per la popolazione italiana—IV Revisione. 2014. http://www.sinu.it/html/pag/tabelle_larn_2014_rev.asp.
Cosman F, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359–81.
Russell RGG. Bisphosphonates: mode of action and pharmacology. Pediatrics. 2007;119(Supplement):S150–62.
Ebetino FH, et al. The relationship between the chemistry and biological activity of the bisphosphonates. Bone. 2011;49(1):20–33.
Soares AP, et al. Bisphosphonates: Pharmacokinetics, bioavailability, mechanisms of action, clinical applications in children, and effects on tooth development. Environ Toxicol Pharmacol. 2016;42:212–7.
Gertz BJ, Holland SD, Kline WF, Matuszewski BK, Porras AG. Clinical pharmacology of alendronate sodium. Osteoporos Int. 1993;3(Suppl 3):S13–6.
Baroncelli GI, Bertelloni S. The use of bisphosphonates in pediatrics. Horm Res Paediatr. 2014;82(5):290–302.
Bishop N, et al. Risedronate in children with osteogenesis imperfecta: a randomised, double-blind, placebo-controlled trial. Lancet. 2013;382(9902):1424–32.
DiMeglio LA, Peacock M. Two-year clinical trial of oral alendronate versus intravenous pamidronate in children with osteogenesis imperfecta. J Bone Miner Res. 2006;21(1):132–40.
Sakkers R, et al. Skeletal effects and functional outcome with olpadronate in children with osteogenesis imperfecta: a 2-year randomised placebo-controlled study. Lancet. 2004;363(9419):1427–31.
Rauch F, Munns CF, Land C, Cheung M, Glorieux FH. Risedronate in the treatment of mild pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Bone Miner Res. 2009;24(7):1282–9.
Ward LM, et al. Alendronate for the treatment of pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Clin Endocrinol Metab. 2011;96(2):355–64.
Land C, Rauch F, Munns CF, Sahebjam S, Glorieux FH. Vertebral morphometry in children and adolescents with osteogenesis imperfecta: effect of intravenous pamidronate treatment. Bone. 2006;39(4):901–6.
Zeitlin L, Rauch F, Plotkin H, Glorieux FH. Height and weight development during four years of therapy with cyclical intravenous pamidronate in children and adolescents with osteogenesis imperfecta types I, III, and IV. Pediatrics. 2003;111(5 Pt 1):1030–6.
Munns CF, Rauch F, Travers R, Glorieux FH. Effects of intravenous pamidronate treatment in infants with osteogenesis imperfecta: clinical and histomorphometric outcome. J Bone Miner Res. 2005;20(7):1235–43.
DiMeglio LA, Ford L, McClintock C, Peacock M. Intravenous pamidronate treatment of children under 36 months of age with osteogenesis imperfecta. Bone. 2004;35(5):1038–45.
Kusumi K, Ayoob R, Bowden SA, Ingraham S, Mahan JD. Beneficial effects of intravenous pamidronate treatment in children with osteogenesis imperfecta under 24 months of age. J Bone Miner Metab. 2015;33(5):560–8.
Lin CH, et al. Cyclic pamidronate infusion for neonatal-onset osteogenesis imperfecta. Pediatr Neonatol. 2014;55(4):306–11.
Gandrud LM, Cheung JC, Daniels MW, Bachrach LK. Low-dose intravenous pamidronate reduces fractures in childhood osteoporosis. J Pediatr Endocrinol Metab. 16(6):887–92.
Steelman J, Zeitler P. Treatment of symptomatic pediatric osteoporosis with cyclic single-day intravenous pamidronate infusions. J Pediatr. 2003;142(4):417–23.
Maines E, Monti E, Doro F, Morandi G, Cavarzere P, Antoniazzi F. Children and adolescents treated with neridronate for osteogenesis imperfecta show no evidence of any osteonecrosis of the jaw. J Bone Miner Metab. 2012;30(4):434–8.
Barros ER, Saraiva GL, de Oliveira TP, Lazaretti-Castro M. Safety and efficacy of a 1-year treatment with zoledronic acid compared with pamidronate in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab. 2012;25(5–6):485–91.
Ooi HL, Briody J, Biggin A, Cowell CT, Munns CF. Intravenous zoledronic acid given every 6 months in childhood osteoporosis. Horm Res Paediatr. 2013;80(3):179–84.
George S, Weber DR, Kaplan P, Hummel K, Monk HM, Levine MA. Short-term safety of zoledronic acid in young patients with bone disorders: an extensive institutional experience. J Clin Endocrinol Metab. 2015;100(11):4163–71.
Al-Agha A, Hayatalhazmi R. Osteoporosis treatment with zoledronic acid in pediatric population at a university hospital in Western Saudi Arabia. A 13-year experience. Saudi Med J. 2015;36(11):1312–8.
Robins SP, New SA. Markers of bone turnover in relation to bone health. Proc Nutr Soc. 1997;56(3):903–14.
Wheater G, Elshahaly M, Tuck SP, et al. The clinical utility of bone marker measurements in osteoporosis. J Transl Med. 2013;11:201.
Parfitt AM, Simon LS, Villanueva AR, Krane SM. Procollagen type I carboxy-terminal extension peptide in serum as a marker of collagen biosynthesis in bone. Correlation with Iliac bone formation rates and comparison with total alkaline phosphatase. J Bone Miner Res. 1987;2(5):427–36.
Minkin C. Bone acid phosphatase: tartrate-resistant acid phosphatase as a marker of osteoclast function. Calcif Tissue Int. 1982;34(3):285–90.
Risteli L, Risteli J. Products of bone collagen metabolism. In: Seibel MJ, Robins SP, Bilezikian JP, editors. Dynamics of bone and cartilage metabolism: principles and clinical applications. London: Academic Press; 1999. p. 275–87.
Vasikaran S, Cooper C, Eastell R, et al. International Osteoporosis Foundation and International Federation of Clinical Chemistry and Laboratory Medicine Position on bone marker standards in osteoporosis. Clin Chem Lab Med. 2011;49(8):1271–4.
Rauchenzauner M, et al. Sex- and age-specific reference curves for serum markers of bone turnover in healthy children from 2 months to 18 years. J Clin Endocrinol Metab. 2007;92(2):443–9.
Bayer M. Reference values of osteocalcin and procollagen type I N-propeptide plasma levels in a healthy Central European population aged 0–18 years. Osteoporos Int. 2014;25(2):729–36.
Rauch F, Plotkin H, Travers R, Zeitlin L, Glorieux FH. Osteogenesis imperfecta types I, III, and IV: effect of pamidronate therapy on bone and mineral metabolism. J Clin Endocrinol Metab. 2003;88(3):986–92.
Kennel KA, Drake MT. Adverse effects of bisphosphonates: implications for osteoporosis management. Mayo Clin Proc. 2009;84(7):632–8.
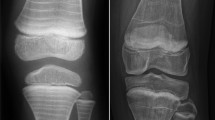
Sarraf KM. Radiographic zebra lines from cyclical pamidronate therapy. N Engl J Med. 2011;365(5):2015.
Silva EC, Terreri MT, de Castro TC, et al. Sclerotic metaphyseal lines in children and adolescents treated with alendronate. Rev Bras Reumatol. 2010;50(3):283–90.
Land C, Rauch F, Glorieux FH. Cyclical intravenous pamidronate treatment affects metaphyseal modeling in growing patients with osteogenesis imperfecta. J Bone Miner Res. 2005;21(3):374–9.
Abrahamsen B. Bisphosphonate adverse effects, lessons from large databases. Curr Opin Rheumatol. 2010;22(4):404–9.
Hennedige AA, Jayasinghe J, Khajeh J, Macfarlane TV. Systematic review on the incidence of bisphosphonate related osteonecrosis of the jaw in childrendiagnosed with osteogenesis imperfecta. J Oral Maxillofac Res. 2014;4(4):e1.
Ruggiero SL, et al. American association of oral and maxillofacial surgeons position paper on bisphosphonate-related osteonecrosis of the jaw—2009 update. Aust Endod J. 2009;35(3):119–30.
Frost HM. The mechanostat: a proposed pathogenic mechanism of osteoporoses and the bone mass effects of mechanical and nonmechanical agents. Bone Miner. 1987;2:73–85.
Munns CF, Rauch F, Zeitlin L, Fassier F, Glorieux FH. Delayed osteotomy but not fracture healing in pediatric osteogenesis imperfecta patients receiving pamidronate. J Bone Miner Res. 2004;19(11):1779–86.
Anam EA, Rauch F, Glorieux FH, Fassier F, Hamdy R. Osteotomy healing in children with osteogenesis imperfecta receiving bisphosphonate treatment. J Bone Miner Res. 2015;30(8):1362–8.
Bubbear JS. Atypical femur fractures in patients treated with bisphosphonates: identification, management, and prevention. Rambam Maimonides Med J. 2016;7(4):e0032.
van de Laarschot DM, Zillikens MC. Atypical femur fracture in an adolescent boy treated with bisphosphonates for X-linked osteoporosis based on PLS3 mutation. Bone. 2016;91:148–51.
Etxebarria-Foronda I, Carpintero P. An atypical fracture in male patient with osteogenesis imperfecta. Clin Cases Miner Bone Metab. 2015;12(3):278–81.
Whyte MP, Wenkert D, Clements KL, McAlister WH, Mumm S. Bisphosphonate-induced osteopetrosis. N Engl J Med. 2003;349(5):457–63.
Heczey A, Louis C. Images in clinical medicine. Osteopetrosis and erlenmeyer-flask deformity. N Engl J Med. 2015;373(10):e12.
Whyte MP, McAlister WH, Novack DV, Clements KL, Schoenecker PL, Wenkert D. Bisphosphonate-induced osteopetrosis: novel bone modeling defects, metaphyseal osteopenia, and osteosclerosis fractures after drug exposure ceases. J Bone Miner Res. 2008;23(10):1698–707.
Ward K, Cowell CT, Little DG. Quantification of metaphyseal modeling in children treated with bisphosphonates. Bone. 2005;36(6):999–1002.
Rauch F, Cornibert S, Cheung M, Glorieux FH. Long-bone changes after pamidronate discontinuation in children and adolescents with osteogenesis imperfecta. Bone. 2007;40(4):821–7.
Biggin A, Zheng L, Briody JN, Coorey CP, Munns CF. The long-term effects of switching from active intravenous bisphosphonate treatment to low-dose maintenance therapy in children with osteogenesis imperfecta. Horm Res Paediatr. 2015;83(3):183–9.
McKenzie AF, Budd RS, Yang C, Shapiro B, Hicks RJ. Technetium-99 m-methylene diphosphonate uptake in the fetal skeleton at 30 weeks gestation. J Nucl Med. 1994;35(8):1338–41.
Patlas N, Golomb G, Yaffe P, Pinto T, Breuer E, Ornoy A. Transplacental effects of bisphosphonates on fetal skeletal ossification and mineralization in rats. Teratology. 1999;60(2):68–73.
Green SB, Pappas AL. Effects of maternal bisphosphonate use on fetal and neonatal outcomes. Am J Heal Pharm. 2014;71(23):2029–36.
Ioannis SP, et al. The use of bisphosphonates in women prior to or during pregnancy and lactation. 2011;10(4):280–91.
Papapoulos SE, Cremers SCLM. Prolonged bisphosphonate release after treatment in children. N Engl J Med. 2007;356(10):1075–6.
Glorieux FH, Bishop NJ, Plotkin H, Chabot G, Lanoue G, Travers R. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med. 1998;339(14):947–52.
Marom R, Lee Y-C, Grafe I, Lee B. Pharmacological and biological therapeutic strategies for osteogenesis imperfecta. Am J Med Genet Part C Semin Med Genet. 2016;172(4):367–83.
Dwan K, Phillipi CA, Steiner RD, Basel D. Bisphosphonate therapy for osteogenesis imperfecta. In: Basel D, editor. Cochrane database of systematic reviews. Chichester: Wiley; 2016.
Seikaly MG, Kopanati S, Salhab N, et al. Impact of alendronate on quality of life in children with osteogenesis imperfecta. J Pediatr Orthop. 2005;25(6):786–91.
Senthilnathan S, Walker E, Bishop NJ. Two doses of pamidronate in infants with osteogenesis imperfecta. Arch Dis Child. 2008;93(5):398–400.
Shi CG, Zhang Y, Yuan W. Efficacy of bisphosphonates on bone mineral density and fracture rate in patients with osteogenesis imperfecta. Am J Ther. 2016;23(3):e894–904.
Šumník Z, Land C, Rieger-Wettengl G, Körber F, Stabrey A, Schoenau E. Effect of pamidronate treatment on vertebral deformity in children with primary osteoporosis. Horm Res Paediatr. 2004;61(3):137–42.
Melchior R, Zabel B, Spranger J, Schumacher R. Effective parenteral clodronate treatment of a child with severe juvenile idiopathic osteoporosis. Eur J Pediatr. 2005;164(1):22–7.
Kauffman RP, Overton TH, Shiflett M, Jennings JC. Osteoporosis in children and adolescent girls: case report of idiopathic juvenile osteoporosis and review of the literature. Obstet Gynecol Surv. 2001;56(8):492–504.
Baroncelli GI, Vierucci F, Bertelloni S, Erba P, Zampollo E, Giuca MR. Pamidronate treatment stimulates the onset of recovery phase reducing fracture rate and skeletal deformities in patients with idiopathic juvenile osteoporosis: comparison with untreated patients. J Bone Miner Metab. 2013;31(5):533–43.
Bellido T, Plotkin LI. Novel actions of bisphosphonates in bone: preservation of osteoblast and osteocyte viability. Bone. 2011;49(1):50–5.
Lara-Castillo N, Johnson ML. LRP receptor family member associated bone disease. Rev Endocr Metab Disord. 2015;16(2):141–8.
Tüysüz B, Bursalı A, Alp Z, Suyugül N, Laine CM, Mäkitie O. Osteoporosis-pseudoglioma syndrome: three novel mutations in the LRP5 gene and response to bisphosphonate treatment. Horm Res Paediatr. 2012;77(2):115–20.
Bayram F, et al. Effects of 3 years of intravenous pamidronate treatment on bone markers and bone mineral density in a patient with osteoporosis-pseudoglioma syndrome (OPPG). J Pediatr Endocrinol Metab. 2006;19(3):275–9.
Barros ER, Dias da Silva MR, Kunii IS, Lazaretti-Castro M. Three years follow-up of pamidronate therapy in two brothers with osteoporosis-pseudoglioma syndrome (OPPG) carrying an LRP5 mutation. J Pediatr Endocrinol Metab. 2008;21(8):811–8.
Streeten EA, et al. Osteoporosis-pseudoglioma syndrome: description of 9 new cases and beneficial response to bisphosphonates. Bone. 2008;43(3):584–90.
Streeten EA, et al. Fractures on bisphosphonates in osteoporosis pseudoglioma syndrome (OPPG): pQCT shows poor bone density and structure. Bone. 2015;77:17–23.
Leonard MB. Glucocorticoid-induced osteoporosis in children: impact of the underlying disease. Pediatrics. 2007;119(Supplement):S166–74.
Allen CS, Yeung JH, Vandermeer B, Homik J. Bisphosphonates for steroid-induced osteoporosis. In: Homik J, editor. Cochrane database of systematic reviews. Chichester: Wiley; 2016.
Jayasena A, Atapattu N, Lekamwasam S. Treatment of glucocorticoid-induced low bone mineral density in children: a systematic review. Int J Rheum Dis. 2015;18(3):287–93.
Bianchi ML, et al. Efficacy and safety of alendronate for the treatment of osteoporosis in diffuse connective tissue diseases in children: a prospective multicenter study. Arthritis Rheum. 2000;43(9):1960–6.
Acott PD, Wong JA, Lang BA, Crocker JFS. Pamidronate treatment of pediatric fracture patients on chronic steroid therapy. Pediatr Nephrol. 2005;20(3):368–73.
Ozel S, Switzer L, Macintosh A, Fehlings D. Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: an update. Dev Med Child Neurol. 2016;58(9):918–23.
Guo Z, et al. The efficacy and safety of bisphosphonates for osteoporosis or osteopenia in Crohn’s disease: a meta-analysis. Dig Dis Sci. 2013;58(4):915–22.
Bachrach LK, Ward LM. Clinical review: bisphosphonate use in childhood osteoporosis. J Clin Endocrinol Metab. 2009;94(2):400–9.
Ward L, et al. Bisphosphonate therapy for children and adolescents with secondary osteoporosis. In: Ward L, editor. Cochrane database of systematic reviews. Chichester: Wiley; 2007.
Suda T, Takahashi N, Udagawa N, Jimi E, Gillespie MT, Martin TJ. Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocr Rev. 1999;20(3):345–57.
Arai F, et al. Commitment and differentiation of osteoclast precursor cells by the sequential expression of c-Fms and receptor activator of nuclear factor kappaB (RANK) receptors. J Exp Med. 1999;190(12):1741–54.
Canalis E. Mechanisms of glucocorticoid action in bone. Curr Osteoporos Rep. 2005;3(3):98–102.
Suresh E, Abrahamsen B. Denosumab: a novel antiresorptive drug for osteoporosis. Cleve Clin J Med. 2015;82(2):105–14.
Semler O, Netzer C, Hoyer-Kuhn H, Becker J, Eysel P, Schoenau E. First use of the RANKL antibody denosumab in osteogenesis imperfecta type VI. J Musculoskelet Neuronal Interact. 2012;12(3):183–8.
Hoyer-Kuhn H, Netzer C, Koerber F, Schoenau E, Semler O. Two years’ experience with denosumab for children with Osteogenesis imperfecta type VI. Orphanet J Rare Dis. 2014;9(1):145.
Hoyer-Kuhn H, et al. Safety and efficacy of denosumab in children with osteogenesis imperfect—a first prospective trial. J Musculoskelet Neuronal Interact. 2016;16(1):24–32.
Wang HD, et al. Effects of denosumab treatment and discontinuation on human growth plates. J Clin Endocrinol Metab. 2014;99(3):891–7.
Scheinberg MA, Golmia RP, Sallum AME, et al. Bone health in cerebral palsy and introduction of a novel therapy. Einstein (Sao Paulo) 2015;13(4):555–9.
Farrier AJ, et al. New anti-resorptives and antibody mediated anti-resorptive therapy. Bone Joint J. 2016;98-B(2):160–165.
Duong LT, Leung AT, Langdahl B. Cathepsin K inhibition: a new mechanism for the treatment of osteoporosis. Calcif Tissue Int. 2016;98(4):381–97.
Mukherjee K, Chattopadhyay N. Pharmacological inhibition of cathepsin K: a promising novel approach for postmenopausal osteoporosis therapy. Biochem Pharmacol. 2016;117:10–9.
Rizzoli R, et al. Continuous treatment with odanacatib for up to 8 years in postmenopausal women with low bone mineral density: a phase 2 study. Osteoporos Int. 2016;27(6):2099–107.
Lindsay R, Krege JH, Marin F, Jin L, Stepan JJ. Teriparatide for osteoporosis: importance of the full course. Osteoporos Int. 2016;27(8):2395–410.
Vahle JL, Sato M, Long GG, et al. Skeletal changes in rats given daily subcutaneous injections of recombinant human parathyroid hormone (1–34) for 2 years and relevance to human safety. Toxicol Pathol. 2002;30(3):312–21.
Cipriani C, Capriani C, Irani D, Bilezikian JP. Safety of osteoanabolic therapy: a decade of experience. J Bone Miner Res. 2012;27(12):2419–28.
McClung MR, et al. Romosozumab in postmenopausal women with low bone mineral density. N Engl J Med. 2014;370(5):412–20.
Genant HK, Engelke K, Bolognese MA, et al. Effects of romosozumab compared with teriparatide on bone density and mass at the spine and hip in postmenopausal women with low bone mass. J Bone Miner Res. 2017;32(1):181–7.
Li X. Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling. J Biol Chem. 2005;280(20):19883–7.
Semenov M, Tamai K, He X. SOST is a ligand for LRP5/LRP6 and a Wnt signaling inhibitor. J Biol Chem. 2005;280(29):26770–5.
Kedlaya R, et al. Sclerostin inhibition reverses skeletal fragility in an Lrp5-deficient mouse model of OPPG syndrome. Sci Transl Med. 2013;5(211):211ra158–211ra158.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Edoardo Marrani, Teresa Giani, Gabriele Simonini, and Rolando Cimaz declare no conflicts of interest.
Funding
No funding was used for this manuscript.
Rights and permissions
About this article
Cite this article
Marrani, E., Giani, T., Simonini, G. et al. Pediatric Osteoporosis: Diagnosis and Treatment Considerations. Drugs 77, 679–695 (2017). https://doi.org/10.1007/s40265-017-0715-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-017-0715-3