Abstract
Background
Postoperative ileus (POI) is common after gastrointestinal surgery and is associated with significant morbidity and costs. However, POI is poorly defined. The I-FEED score is a novel outcome measure for POI, developed by expert consensus. It contains five elements (intake, response to nausea treatment, emesis, exam, and duration, each scored with 0, 1, or 3 points) and classifies patients into normal, postoperative gastrointestinal intolerance (POGI), and postoperative gastrointestinal dysfunction (POGD). However, it has not yet been validated in a clinical context. The objective was to provide validity evidence for the I-FEED score to measure the construct of POI in patients undergoing colorectal surgery.
Methods
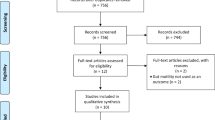
Data previously collected from a clinical trial investigating the impact of different perioperative fluid management strategies on primary POI in patients undergoing elective laparoscopic colectomy (2013–2015) were analyzed. Patients were managed by a longstanding Enhanced Recovery program (expected length of stay (LOS): 3 days). Daily I-FEED scores were generated (normal 0–2, POGI 3–5, POGD 6+ points) up to hospital discharge or postoperative day 7. Validity was assessed by testing the hypotheses that I-FEED score was higher (1) in patients with longer time to GI3 (tolerating diet + flatus/bowel movement), (2) with longer LOS (> 3 days vs shorter), (3) in patients with complications vs without, (4) in patients with poorer recovery (measured by Quality of Recovery-9 questionnaire).
Results
A total of 128 patients were included for analysis (mean age 61.7 years (SD 15.2), 57% male, 71% malignancy, and 39.1% rectal resection). Median LOS was 4 days [IQR3–5], and 32% experienced postoperative in-hospital morbidity. Overall, 48% of patients were categorized as normal, 22% POGI, and 30% POGD. The data supported all 4 hypotheses.
Conclusions
This study contributes preliminary validity evidence for the I-FEED score as a measure for POI after colorectal surgery.


Similar content being viewed by others
References
Augestad KM, Delaney CP (2010) Postoperative ileus: impact of pharmacological treatment, laparoscopic surgery and enhanced recovery pathways. World J Gastroenterol 16:2067–2074
Kehlet H, Holte K (2001) Review of postoperative ileus. Am J Surg 182:3S–10S
Vather R, Trivedi S, Bissett I (2013) Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg 17:962–972
Iyer S, Saunders WB, Stemkowski S (2009) Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm 15:485–494
Wolthuis AM, Bislenghi G, Fieuws S, de Buck van Overstraeten A, Boeckxstaens G, Dhoore A (2016) Incidence of prolonged postoperative ileus after colorectal surgery: a systematic review and meta-analysis. Colorectal Dis 18:1–9
Hedrick TL, McEvoy MD, Mythen MG, Bergamaschi R, Gupta R, Holubar SD, Senagore AJ, Gan TJ, Shaw AD, Thacker JKM, Miller TE, Wischmeyer PE, Carli F, Evans DC, Guilbert S, Kozar R, Pryor A, Thiele RH, Everett S, Grocott M, Abola RE, Bennett-Guerrero E, Kent ML, Feldman LS, Fiore JF Jr, Perioperative Quality Initiative (POQI) 2 Workgroup (2017) American Society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg 126(6):1896–1907
Gomez-Izquierdo JC, Trainito A, Mirzakandov D, Stein BL, Liberman S, Charlebois P, Pecorelli N, Feldman LS, Carli F, Baldini G (2017) Goal-directed fluid therapy does not reduce primary postoperative ileus after elective laparoscopic colorectal surgery: a randomized controlled trial. Anesthesiology 127:36–49
Lee L, Mata J, Ghitulescu GA, Boutros M, Charlebois P, Stein B, Liberman AS, Fried GM, Morin N, Carli F, Latimer E, Feldman LS (2015) Cost-effectiveness of enhanced recovery versus conventional perioperative management for colorectal surgery. Ann Surg 262:1026–1033
Kolozsvari NO, Capretti G, Kaneva P, Neville A, Carli F, Liberman S, Charlebois P, Stein B, Vassiliou MC, Fried GM, Feldman LS (2013) Impact of an enhanced recovery program on short-term outcomes after scheduled laparoscopic colon resection. Surg Endosc 27:133–138
Carli F, Charlebois P, Baldini G, Cachero O, Stein B (2009) An integrated multidisciplinary approach to implementation of a fast-track program for laparoscopic colorectal surgery. Can J Anaesth 56:837–842
Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, Bouter LM, de Vet HC (2010) The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol 10:22
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC (2010) The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 19:539–549
Myles PS, Hunt JO, Nightingale CE, Fletcher H, Beh T, Tanil D, Nagy A, Rubinstein A, Ponsford JL (1999) Development and psychometric testing of a quality of recovery score after general anesthesia and surgery in adults. Anesth Analg 88:83–90
Terwee CB, Mokkink LB, Knol DL, Ostelo RW, Bouter LM, de Vet HC (2012) Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res 21:651–657
Chapman SJ, Pericleous A, Downey C, Jayne DG (2018) Postoperative ileus following major colorectal surgery. Br J Surg 105:797–810
Kellum JA, Bellomo R, Ronco C (2008) Acute dialysis quality initiative (ADQI): methodology. Int J Artif Organs 31:90–93
Barbieux J, Hamy A, Talbot MF, Casa C, Mucci S, Lermite E, Venara A (2017) Does enhanced recovery reduce postoperative ileus after colorectal surgery? J Visc Surg 154:79–85
Grass F, Slieker J, Jurt J, Kummer A, Sola J, Hahnloser D, Demartines N, Hubner M (2017) Postoperative ileus in an enhanced recovery pathway—a retrospective cohort study. Int J Colorectal Dis 32:675–681
Chapuis PH, Bokey L, Keshava A, Rickard MJ, Stewart P, Young CJ, Dent OF (2013) Risk factors for prolonged ileus after resection of colorectal cancer: an observational study of 2400 consecutive patients. Ann Surg 257:909–915
Nadler A, Pearsall EA, Victor JC, Aarts MA, Okrainec A, McLeod RS (2014) Understanding surgical residents’ postoperative practices and barriers and enablers to the implementation of an Enhanced Recovery After Surgery (ERAS) Guideline. J Surg Educ 71:632–638
Thacker JK, Mountford WK, Ernst FR, Krukas MR, Mythen MM (2016) Perioperative fluid utilization variability and association with outcomes: considerations for enhanced recovery efforts in sample US surgical populations. Ann Surg 263:502–510
Pecorelli N, Hershorn O, Baldini G, Fiore JF Jr, Stein BL, Liberman AS, Charlebois P, Carli F, Feldman LS (2017) Impact of adherence to care pathway interventions on recovery following bowel resection within an established enhanced recovery program. Surg Endosc 31:1760–1771
Lee L, Li C, Landry T, Latimer E, Carli F, Fried GM, Feldman LS (2014) A systematic review of economic evaluations of enhanced recovery pathways for colorectal surgery. Ann Surg 259:670–676
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Nourah Alsharqawi, Dr. Mohsen Alhashemi, Ms. Pepa Kaneva, and Dr. Gabriele Baldini have no conflicts of interest to disclose or financial ties to disclose. Dr. Lawrence Lee is the recipient of an investigator-initiated grant from Johnson & Johnson. Dr. Liane Feldman and Dr. Julio Fiore Jr. are the recipients of an investigator-initiated grant from Merck.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alsharqawi, N., Alhashemi, M., Kaneva, P. et al. Validity of the I-FEED score for postoperative gastrointestinal function in patients undergoing colorectal surgery. Surg Endosc 34, 2219–2226 (2020). https://doi.org/10.1007/s00464-019-07011-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07011-6