Abstract
Introduction
The posterior malleolus (PM) is affected in around the 40% of ankle fractures. Anatomical reduction of the articular surface and fibular notch are essential for ankle stability and functional outcomes. These facts justify the increasing interest in the surgical treatment of PM in ankle fractures. Within this context, pre-operative computed tomography (CT) images and posterior approaches to the ankle play a crucial role. The aim of this paper is to make an accurate description of the literature and describe, according to authors’ experience, the best surgical approach to the PM based on the CT findings while assessing their advantages and disadvantages.
Methods
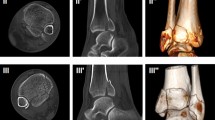
The fracture pattern of PM is classified according to Haraguchi or Bartoníček classification, both based on pre-operative CT scan images. The posterolateral (PLA) and posteromedial (PMA) approaches to the ankle and their corresponding modifications are described. We propose a decision-making algorithm for posterior malleolus fractures to facilitate treatment selection.
Results
Posterolateral approach should be the election for Haraguchi I or III and Bartoníček 1, 2, or 4 fractures. Percutaneous PLA might be adequate in Haraguchi I and Bartoníček 1 to improve syndesmotic stability. In PL approaches, the fibula fracture may be addressed and fixed with a posterolateral plate or through a subcutaneous window that allows lateral reduction and fixation. Posteromedial approach should be the election for Haraguchi II and Bartoníček 3 fractures. A modified PMA might be the election to reduce and fix any fragment dependent on the anterior inferior tibiofibular ligament (AITFL). The modified PMA is performed in a supine position and allows us to check the articular reduction under direct vision. Both PMA are associated with a lateral fibular approach.
Conclusion
To address the posterior malleolus when treating ankle fractures, surgeons should choose the most adequate approach based on the fracture pattern and their own experience. Anatomical reduction and stable fixation are critical to improve outcomes.









Similar content being viewed by others
References
Court-Brown CM, McBirnie J, Wilson G (1998) Adult ankle fractures - an increasing problem? Acta Orthop Scand 69(1):43–47
Drijjfhout van Hooff CC, Verhage SM, Hoogendoorn JM (2015) Influence of fragment size and postoperative joint congruency on long-term outcome of posterior malleolar fractures. Foot Ankle Int 36(6):673–678
De Vries J, Wijgman A, Sierevelt I, Schaap G (2005) Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg 44(3):211–217
Hartford JM, Gorczyca JT, McNamara JL, Mayor B (1995) Tibiotalar contact area. Contribution of posterior malleolus and deltoid ligament. Clin Orthop Relat Res 320:182–187
Assal M, Dalmau-Pastor M, Ray A, Stern R (2017) How to get to the distal posterior tibial malleolus? A cadaveric anatomic study defining the access corridors through 3 different approaches. J Orthop Trauma 31(4):127–129
White TO (2018) In defence of the posterior malleolus. Bone Jt J 100B(5):566–569
Haraguchi N, Haruyama H, Toga H, Kato F (2006) Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Jt Surg 88(5):1085–1092
Bartoníček J, Rammelt S, Kostlivý K, Vaněček V, Klika D, Trešl I (2015) Anatomy and classification of the posterior tibial fragment in ankle fractures. Arch Orthop Trauma Surg 135(4):505–516
Donohoe S, Alluri RK, Hill JR, Fleming M, Tan E, Marecek G (2017) Impact of computed tomography on operative planning for ankle fractures involving the posterior malleolus. Foot Ankle Int 38(12):1337–1342
Kumar A, Mishra P, Tandon A, Arora R, Chadha M (2018) Effect of CT on management plan in malleolar ankle fractures. Foot Ankle Int 39(1):59–66
Verhage SM, Hoogendoorn JM, Krijnen P, Schipper IB (2018) When and how to operate the posterior malleolus fragment in trimalleolar fractures: a systematic literature review. Arch Orthop Trauma Surg 138(9):1213–1222
Abdelgawad AA, Kadous A, Kanlic E (2011) Posterolateral approach for treatment of posterior malleolus fracture of the ankle. J Foot Ankle Surg 50(5):607–611
Ruokun H, Ming X, Zhihong X, Zhenhua F, Jingjing Z, Kai X et al (2014) Postoperative radiographic and clinical assessment of the treatment of posterior tibial plafond fractures using a posterior lateral incisional approach. J Foot Ankle Surg 53(6):678–682
Hoppenfeld S, DeBoer P (1994) Surgical exposures in orthopaedics. The anatomic approach, 2nd edn. Lippincott, Williams &Wilkins, Philadelphia
Tornetta P, Ricci W, Nork S, Collinge C, Steen B (2011) The posterolateral approach to the tibia for displaced posterior malleolar injuries. J Orthop Trauma 25(2):123–126
Mason LW, Marlow WJ, Widnall J, Molloy AP (2017) Pathoanatomy and associated injuries of posterior malleolus fracture of the ankle. Foot Ankle Int 38(11):1229–1235
Ramakrishnan P, Henry B, Vikse J (2015) Anatomical variations of the formation and course of the sural nerve: a systematic review and meta-analysis. Ann Anat 202:36–44
LeBus GF, Collinge C (2008) Vascular abnormalities as assessed with CT angiography in high-energy tibial plafond fractures. J Orthop Trauma 22(1):16–22
Sandelin H, Tukiainen E, Ovaska M (2017) Amputation following internal fixation of an ankle fracture via the posterolateral approach–a case report. Acta Orthop 88(3):358–360
Lidder S, Masterson S, Dreu M, Clement H, Grechenig S (2014) The risk of injury to the peroneal artery in the posterolateral approach to the distal tibia: a cadaver study. J Orthop Trauma 28(9):534–537
Choi JY, Kim JH, Ko HT, Suh JS (2015) Single oblique posterolateral approach for open reduction and internal fixation of posterior malleolar fractures with an associated lateral malleolar fracture. J Foot Ankle Surg 54(4):559–564
Gardner MJ, Brodsky A, Briggs SM, Nielson JH, Lorich DG (2006) Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 447:165–171
Gatellier J, Chastang P (1924) Access to fractured malleolus with piece chipped off at back. J Chir 24:513
Rammelt S, Zwipp H, Mittlmeier T (2013) Operative treatment of pronation fracture–dislocations of the ankle. Oper Orthop Traumatol 25(3):273–293
Kim MB, Lee YH, Kim JH, Lee JE, Baek GH (2015) Lateral transmalleolar approach and miniscrews fixation for displaced posterolateral fragments of posterior malleolus fractures in adults: a consecutive study. J Orthop Trauma 29(2):105–109
Hoekstra H, Rosseels W, Rammelt S, Nijs S (2017) Direct fixation of fractures of the posterior pilon via a posteromedial approach. Injury 48(6):1269–1274
Liporace FA, Mehta S, Rhorer AS, Yoon RS, Reilly MC (2012) Staged treatment and associated complications of pilon fractures. Instr Course Lect 61:53–70
Wang Y, Wang J, Luo CF (2016) Modified posteromedial approach for treatment of posterior pilon variant fracture. BMC Musculoskelet Disord 17(1):1–8
Bois AJ, Dust W (2008) Posterior fracture dislocation of the ankle: technique and clinical experience using a posteromedial surgical approach. J Orthop Trauma 22(9):629–636
Nielson JH, Sallis JG, Potter HG (2004) Correlation of interosseous membrane tears to the level of the fibular fracture. J Orthop Trauma 18(2):68–74
Macko V, Matthews L, Zwirkoski P, Goldstein S (1991) The joint-contact area of the ankle. The contribution of the posterior malleolus. J Bone Jt Surg Am Vol 73(3):347–351
Meijer DT, Doornberg JN, Sierevelt IN, Mallee WH, Van Dijk CN, Kerkhoffs GM et al (2015) Guesstimation of posterior malleolar fractures on lateral plain radiographs. Injury 46(10):2024–2029
Minihane KP, Lee C, Ahn C, Zhang LQ, Merk BR (2006) Comparison of lateral locking plate and antiglide plate for fixation of distal fibular fractures in osteoporotic bone: a biomechanical study. J Orthop Trauma 20(8):562–566
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
1 Anatomical reduction and stable fixation of posterior malleolus in ankle fractures are critical to improve outcomes.
2 The posterior malleolus should be addressed via posterolateral or posteromedial approach based on pre-operative CT scan images.
3. Haraguchi I or III and Bartonicek 1, 2, or 4 fractures are suitable for a posterolateral approach.
4. Haraguchi II or Bartonicek 3 fractures are suitable for a posteromedial approach.
5. A careful study of the pre-operative CT scan images allows the surgeon to choose between the classical posterolateral and posteromedial approaches and their modifications as well as the best approach to the fibula.
Rights and permissions
About this article
Cite this article
Vacas-Sánchez, E., Olaya-González, C., Abarquero-Diezhandino, A. et al. How to address the posterior malleolus in ankle fractures? A decision-making model based on the computerised tomography findings. International Orthopaedics (SICOT) 44, 1177–1185 (2020). https://doi.org/10.1007/s00264-020-04481-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04481-5