Abstract
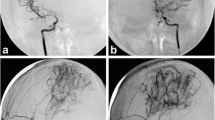
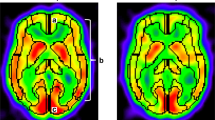
The distribution pattern of cerebral blood flow (CBF) was evaluated in 13 children with moyamoya disease after revascularization. Combined surgery involving encephaloduroarteriosynangiosis and encephalomyosynangiosis was performed in 21 hemispheres. CBF was assessed by dynamic imaging using N-isopropyl-p[123I]iodoamphetamine-single photon emission CT (IMP-SPECT) at 46 months on average after revascularization. None of the patients suffered recurrent ischemic attacks after the bilateral combined surgery, and 62% showed excellent active daily life. However, 70% showed poor school performance with impaired cognitive function. Although the superficial temporal artery was dilated in follow-up angiograms, the revascularized area was confined to the craniotomy field. CBF images disclosed a low-perfusion state with a noninfarcted ischemic pattern in 71% of the revascularized hemispheres, especially in the frontal lobe. These findings show that although potentially beneficial effects can be expected following revascularization, it should be recognized that, in most patients, increased blood flow is gained only in a limited area around the surgical field. For patients who show progressive reduction of regional CBF, additional revascularization procedures are recommended.
Similar content being viewed by others
References
Astrup J, Siesjö BK, Symon L (1981) Thresholds in cerebral ischemia — the ischemic penumbra. Stroke 12:723–725
Baron JC, Rey A, Guillard A, Bousser MG, Comar D, Castaigne P (1981) Noninvasive tomographic imaging of cerebral blood flow and oxygen extraction fraction in superficial temporal artery to middle cerebral artery anastomosis. In: Meyre JS, Lechner H, Reivich M, Ott EO, Aranibar A (eds) Cerebrovascular disease 3. Excerpta Medica, Amsterdam, pp 58–64
Carlson CB, Harvey FH, Loop J (1973) Progressive alternating hemiplegia in early childhood with basal arterial stenosis and teleangiectasia (moyamoya syndrome). Neurology 23:734–744
Creutzig H, Schober O, Gielow R, Friedrich H, Becker H, Dietz H, Hundeshagen H (1986) Cerebral dynamics of N-isopropyl-[123I]p-iodoamphetamine. J Nucl Med 27:178–183
Fujita K, Tamaki N, Matsumoto S (1986) Surgical treatment of moyamoya disease in children: which is more effective procedure, EDAS or EMS? Child's Nerv Syst 2:134–138
Fukuyama Y, Umezu R (1985) Clinical and cerebral angiographic evaluations of idiopathic progressive occlusive disease of the circle of Willis in children. Brain Dev 7:21–37
Henschen C (1950) Operative Revaskularisation des zirkulatorisch geschädigten Gehirns durch Auflage gestielter Muskellappen (Encephalo-Myo-Synangiose). Langenbecks Arch Klin Chir 264:392–401
Karasawa J, Kikuchi H, Furuse S, Sakaki T, Yoshida Y, Ohnishi H, Taki W (1977) A surgical treatment of “moyamoya” disease: “encephalo-myo-synangiosis.” Neurol Med Chir (Tokyo) 17:29–37
Karasawa J, Kikuchi H, Furuse S, Kawamura J, Sakaki T (1978) Treatment of moyamoya disease with STA-MCA anastomosis. J Neurosurg 49:679–688
Karasawa J, Kikuchi H, Matsumoto A, Ito K, Takahashi N (1981) Surgical treatment of “moyamoya” disease — follow-up study during 3.5 years and over. Proceedings of the 10th Japanese Conference on Surgery of Cerebral Stroke, Maebashi, Japan, 1981, pp 306–312
Kitahara T, Okumura K, Semba A, Yamaura A, Makino H (1979) Genetic and immunological analysis on moya-moya. J Neurol Neurosurg Psychiatry 42:208–214
Krayenbühl HA (1975) The moyamoya syndrome and the neurosurgeon. Surg Neurol 4:353–360
Kudo T (1968) Spontaneous occlusion of the circle of Willis. A disease apparently confined to Japanese. Neurology (Minneap) 18:485–496
Kuhl DE, Wu JL, Lin TH, Selin C, Phelps M (1981) Mapping local cerebral blood flow by means of emission computed tomography of N-isopropyl-p[123I]iodoamphetamine (IMP). J Cereb Blood Flow Metab [Suppl 1]:S25–S26
Kuwabara Y (1986) Evaluation of regional cerebral circulation and metabolism in moyamoya disease using positron emission computed tomography (in Japanese). Kakuigaku 23:1381–1402
Lassen NA (1982) Incomplete cerebral infarction — focal incomplete ischemic tissue necrosis not leading to embolism. Stroke 13:522–523
Lassen NA, Henriksen L, Holm S (1983) Cerebral blood-flow tomography: xenon-133 compared with isopropyl-amphetamine-iodine-123: concise communication. J Nucl Med 24:17–21
Maki Y, Nakada Y, Nose T, Yoshii Y (1976) Clinical and radioisotopic follow-up study of ‘moyamoya’. Child's Brain 2:257–271
Matsushima Y, Fukai N, Tanaka K, Tsuruoka S, Inaba Y, Aoyagi M, Ohno K (1981) A new surgical treatment of moyamoya disease in children: a preliminary report. Surg Neurol 15:313–320
Nishimoto A, Takeuchi S (1968) Abnormal cerebrovascular network related to the internal carotid arteries. J Neurosurg 29:255–260
Nishimoto A, Onobe H, Ueta K (1979) Clinical and cerebral blood flow study in moyamoya disease with TIA. Acta Neurol Scand 60 [Suppl 72]:434–435
Olds MV, Griebel RW, Hoffman HJ, Craven M, Chuang S, Shutz H (1987) The surgical treatment of childhood moyamoya disease. J Neurosurg 66:675–680
Spetzler RF, Roski RA, Kopaniky DR (1980) Alternative superficial temporal artery to middle cerebral artery revascularization procedure. Neurosurgery 7:484–486
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Takeuchi K (1961) Occlusive disease of carotid artery. Recent Adv Res Nerv Syst 5:511–513
Takeuchi S, Tsuchida T, Kobayashi K, Fukuda M, Ishii R, Ito J (1983) Treatment of moyamoya disease by temporal muscle graft ‘encephalo-myo-synangiosis’. Child's Brain 10:1–15
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sato, H., Sato, N., Tamaki, N. et al. Chronic low-perfusion state in children with moyamoya disease following revascularization. Child's Nerv Syst 6, 166–171 (1990). https://doi.org/10.1007/BF00308495
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/BF00308495