Abstract
During the past 200 years, most countries in the world have experienced a great increase in life expectancy. The timing of the onset of this decrease in mortality and corresponding increase in life expectance has vastly differed between different countries, and this is true for the pace of the development as well. Some countries have still not achieved the life expectancy experienced by the most developed countries already 100 years ago or even earlier. Some countries have even experienced a backlash in the form of declining life expectancy in the 1990s due to, for instance, unemployment and alcohol consumption in some eastern European countries, and the HIV/AIDS epidemic in some African countries. Nevertheless, the general picture of improvement remains massively impressive, and in Sweden life expectancy has increased continuously for more than 200 years.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
During the past 200 years, most countries in the world have experienced a great increase in life expectancy. The timing of the onset of this decrease in mortality and corresponding increase in life expectance has vastly differed between different countries, and this is true for the pace of the development as well. Some countries have still not achieved the life expectancy experienced by the most developed countries already 100 years ago or even earlier. Some countries have even experienced a backlash in the form of declining life expectancy in the 1990s due to, for instance, unemployment and alcohol consumption in some eastern European countries, and the HIV/AIDS epidemic in some African countries. Nevertheless, the general picture of improvement remains massively impressive, and in Sweden life expectancy has increased continuously for more than 200 years.
The secular mortality decline may be explained by a multitude of causes rather than one single cause. These causes may be categorised in different ways and from varying perspectives. Some causal effects (exposure leading to disease) are direct or short-term effects, others are long-term effects. The causes do not only include direct, period effects on mortality and survival such as the immediate effects of outbreaks of infectious diseases, the presence of endemic infections, as well as current hygiene, income, nutrition, housing and health care conditions. The causes also include long-term, sometimes very long-term, effects. The latter group of long-term causal mechanisms by which risk factors and protective factors affect health and disease many years later are often referred to as cohort effects, because different birth cohorts are exposed to different sets of risk factors as well as protective factors during their childhood and adolescense that affect their health in later life.
This contribution will deal with long-term cohort or early life effects on disease in later life, their biological mechanisms in general (not only in Sweden) and their implications for socioeconomic differences in mortality, with particular reference to Sweden. It will also shortly deal with the possibility of making predictions concerning future mortality based on cohort mortality and its indicators in Sweden and in other countries. In the following sections, we will discuss the early life effects and then their biological mechanisms without particular reference to Sweden.
1 The Secular Mortality Decline: Early Life and Cohort Explanations and Their Indicators
By the term period effect, we mean effects on health and survival caused by health determinants (see above) with a short time period between exposure and health/disease outcome (exposure factors which affect the risk of disease may promote either salutogenesis or pathogenesis). For instance, most infectious diseases give rise to symptoms in the very short term (hours-days-weeks) after the initial exposure to infection. However, for some infectious diseases such as tuberculosis (caused by mycobacterium tuberculosis) and leprosy (caused by mycobacterium leprae), the time interval from exposure to disease/symptoms may be much longer (months-years) due to the slow pace of multiplication of the pathogen in the infected human host. Other diseases, especially non-infectious chronic diseases such as many cancers and forms of cardiovascular disease, may have much longer latent periods, i.e. time intervals from exposure of determinants to disease amounting to several decades.
For some diseases, the time lag between exposure and disease may even range from early life (intra-uterine or first year(s) of life) exposure resulting in old-age morbidity and mortality. This set of factors is causally related to the mortality decline and concerns the effects of cohort or early life events on mortality in later life. The general idea behind the notion of cohort effects is that varying forms of stress or heavy disease load on the different organs or organ systems in the human body experienced in early life, most importantly during pregnancy and the first year(s) of life after birth, may “program” the organs to increased susceptibility to various diseases much later in life. However, the notion of cohort or early life causes of disease in later life is not restricted to purely biological mechanisms. Early life events of psychological significance experienced in early life may also give rise to psychological problems or certain persistent personality traits in adulthood (Suomi 1997).
The cohort or early life explanation was proposed by Kermack et al. 1934 (see also Davey Smith and Kuh 2001). They studied age-specific mortality in England, Wales, Scotland and Sweden. Their conclusion was that reductions attained at any particular time in the death rates of the various age groups depended primarily on the date of birth of the individuals, and only secondarily on the actual year of death. The essential beneficial effects on health and survival among adults and older persons were mainly caused by a decrease in disease load achieved in these birth cohorts during early childhood several decades earlier, according to Kermack et al. (1934).
The past decades have witnessed a renewed interest in the cohort or early life approach to disease in Sweden (Bengtsson and Lindström 2000, 2003) as well as in other countries (Preston et al. 1998), particularly in chronic disease epidemiology (Kuh and Ben-Shlomo 1997, 2004; Galobardes et al. 2004). This approach has been heavily supported particularly by the work of Barker and colleagues. They have both hypothesised and investigated the early life preconditions for later life development of cardiovascular diseases and the metabolic syndrome, i.e. coronary/ischaemic heart disease, hypertension, adverse levels of blood cholesterol and lipids, stroke, type II diabetes mellitus, and overweight/obesity (i.e. the components of what some call the “metabolic syndrome”). The causal mechanism behind these diseases induced in early life is suggested to be inadequate cellular development in utero due to lack of sufficient nutrition (Barker 1994, 1995, 1997, 1998, 2001). The concept of down-regulation of fetal growth has been developed further into the nutritional programming (or fetal origins) hypothesis. According to this hypothesis the development of cardiovascular and other diseases in later life depends on whether fetal growth retardation due to insufficient nutrition is “proportionate” or “disproportionate”. The “disproportionate” growth retardation induced by insufficient nutrition during the mid and late trimesters of pregnancy seems to be responsible for cardiovascular diseases later in life, while the “proportionate” growth retardation of the first trimester is not (Barker 1995), although this distinction has later been tuned down by Barker (1998).
Not all evidence suggests an exclusive or even important role of malnutrition in the fetal origins hypothesis. For instance, maternal tuberculosis also impairs fetal growth (Riley 2001). The famine in rural Finland from 1866 to 1868 tripled death rates but did not alter the survivors’ lifespans (Kannisto et al. 1997).
The original disease load mechanism proposed by Kermack et al. has been developed and further investigated. Later Fridlizius (1989) suggested that the development of diseases in later life might be due to exposure to certain infectious diseases. For example exposure to smallpox in the late eighteenth century and exposure to scarlet fever in the mid nineteenth century, in the first 5 years after birth, resulted in reduced immunity against other diseases throughout life and thus a higher susceptibility to getting other infectious diseases in later life. In neither case did susceptibility to disease in adulthood seem to have been connected with nutrition in early life, because the risks of being infected with for instance smallpox and scarlet fever are to a high extent independent of nutrition (Rotberg and Rabb 1985). However, some findings of recent empirical investigations have suggested an association between nutrition and morbidity and mortality of scarlet fever epidemics in the Sundsvall region in northern Sweden (Curtis 2004). In contrast to nutrition, Fridlizius suggested deranged immunological balance between some specific infectious agents and the human host, which has implications for later life experiences of disease (Fridlizius 1989).
In recent years, the rather unspecified mechanisms suggested by Fridlizius have received some support from the bio-medical literature. Chronic inflammatory mechanisms may drive much of the influence of early life infections on later morbidity and mortality. Populations living in high mortality contexts are highly exposed to a wide variety of infectious diseases. Such populations also have high risks of acquiring chronic infectious diseases such as tuberculosis (Lawn et al. 2000) and infections caused by escherichia coli and helicobacter pylori (Cadwgan et al. 2000). These diseases lead to chronically elevated levels of inflammatory markers such as C-reactive protein, interleukin-6, tumour necrosis factor-α and fibrinogen that may mediate between early life infection and later life chronic disease morbidity and mortality (Finch and Crimmins 2004). Thus, reduced morbidity and mortality from infectious diseases in populations experiencing the great mortality decline could produce decreases in exposure to these markers of inflammation. Whether these inflammatory mediators actually have causal influence on chronic disease risk is not established (Timpson et al. 2005).
Helicobacter pylori is an established cause of peptic ulcers, and is associated (although maybe not causally) with coronary heart disease (Harvey et al. 2002). Infections caused by helicobacter pylori are most commonly contracted in infancy and childhood and they persist throughout life. Helicobacter pylori infections are now declining in most low-mortality countries due to improvements in public health and hygiene (Li et al. 2000).
Exposure to infections during the fetal, perinatal and postnatal stages may affect both anatomical/organ development and development of the immune system. The effects of infections during the fetal stage depend on a number of fetal and maternal factors such as nutrition, genetic factors, fetal development stage and anatomical factors. Other examples of such infections are influenza and rubella. One example of a causal association between postnatal infection and adult disease is the association between Hepatitis B and primary liver cancer (Hall and Peckham 1997). A contemporary study from the USA on Americans aged 55–65 years shows that infectious disease during childhood multipled the incidence of lung conditions, such as emphysema and bronchitis, by four in the 55–65-year age group. Non-infectious diseases showed much weaker associations with adult disease (Blackwell et al. 2001). It thus seems plausible that the prenatal and postnatal development of the lungs and the immune system are sensitive to critical events which may influence susceptibility to infections, allergic reactions or toxic exposures, but the exact and specific timing and critical periods for such early life influence on health later in life remain to be disentangled (Strachan 1997). A study of children born in 1921–1935 in Scotland also shows reduced lung capacity (in 1986) for those who experienced pneumonia before the age of 2 years (Shaheen 1997). Factors in utero and during the first years of life may affect the development of asthma later in childhood and adulthood (von Mutius 2001). A review of the effects on human lifespans of the inflammation/infection exposure in early life has proposed a “cohort morbidity phenotype” which represents inflammatory processes that persist from early age into adult life (Finch and Crimmins 2004). Early life experience of diarrhoea with subsequent dehydration may plausibly lead to higher blood pressure, a risk factor for cardiovascular diseases in general and haemorrhagic stroke in particular in later childhood and adulthood, a hypothesis which has been found to be supported by some empirical findings (Davey Smith et al. 2006; Lawlor et al. 2006).
There is also some support in the literature of an effect of both nutrition and disease load (particularly infectious diseases) in early life. Unfavourable early life conditions generally seem to cause permanent biological damage, resulting in higher mortality in later life (Doblhammer and Vaupel 2001). The results of a large sample study of 15 million US deaths between 1989 and 1997 has also suggested effects of season of birth on mortality risk in later life. Being born during a season of hardships is associated with higher mortality in later life (Doblhammer 1999; Doblhammer 2008). Seasonal differences in exposure to infectious disease in early life are associated with mortality in adult life. Seasonal differences in the nutrition of the mother during pregnancy also seem to affect mortality in later life (Doblhammer 2002). A study from contemporary rural Gambia has shown that higher mortality levels are explained by permanently damaging effects during early life of disease exposure as well as malnutrition during the yearly dry-season. Both the damaging effects of disease load and malnutrition during the fetal stage of development are by some authors (Moore et al. 1997) attributed to effects on the immune system, a conclusion that may be supported by historical data (Bengtsson and Lindström 2000, 2003). Several recent studies, however, have cast doubt on this conclusion (Simondon et al. 2004; Moore et al. 2004).
Finch and Crimmins (2004) have recently argued that the inflammatory infection and nutrition hypotheses are not competing or contradictory but complementary in linking two mechanisms of morbidity in early and later life. For example, childhood diarrheas impair cardiac muscle synthesis (Hunter et al. 2001), which could explain associations of infant diarrhea with later cardiovacular disease (Blackwell et al. 2001). Slowed infant growth in the Barker hypothesis might consequently hypothetically be explained by inflammatory reactions in combination with impaired nutrient absorption. There is growing evidence from historical data (1766–1894) in Sweden in support of the disease load (particularly infectious diseases) mechanism suggested in two articles by Bengtsson and Lindström (2000, 2003).
There is also a rapidly accumulating amount of evidence in support of the early life conditions or life course approach in general from modern data (Kuh and Ben-Shlomo 2004; Kuh and Hardy 2002; Davey Smith 2003). The relative abundance (compared to historical data) and diversity of variables in modern data make it possible to attempt to understand the interactions between different determinants and successive exposures during the life course. It should thus be noted that modern data support not only the critical period model, which may be exemplified by the already referred to fetal-origins hypothesis. Modern data also support models following Omran’s assumptions concerning multicausality and interaction of different causal factors in demography and epidemiology (Omran 1971). In contrast to the simpler mono-causal critical period model and fetal-origins hypothesis, the accumulation of risk model assumes that effects accumulate over the life course, although some particular developmental periods may entail greater susceptibility (Ben-Shlomo and Kuh 2002). Harmful effects on health may increase with the duration and/or number of harmful exposures. Exposure to poor socioeconomic conditions may for instance lead to additive effects of experiencing low socioeconomic position during different parts of the life course, which may influence the risk of several diseases (Heslop et al. 2001). The accumulation of risk may also be due to the clustering of exposures (Ben-Shlomo and Kuh 2002).
In modern times, chronic diseases dominate the disease patterns both when it comes to morbidity and mortality. Such diseases include for instance cardiovascular diseases, cancers, rheumatoid arthritis, thyroiditis, and musculosceletal disorders. Coronary heart disease is a good example (Davey Smith and Lynch 2005). It manifests itself during adulthood and old age, but the disease process starts many years earlier with the gradual development of atherosclerosis. This development begins with fatty streaks in the artery walls of children (Berenson et al. 1987). Arterial lesions are also evident in young men suffering from violent death (Strong et al. 1999). Risk factors for coronary heart disease include blood cholesterol levels, smoking, obesity, diabetes mellitus, hypertension, oral contraceptive use among women, psychosocial factors, mental illness, chronic infection/inflammation, coagulation factors, and air pollution (Marmot and Elliot 2005). Several studies have demonstrated that unfavourable pre-adult measures of cholesterol, blood pressure and adiposity are associated with increased intimal-medial thickness, which is a presymptomatic measure of coronary heart disease (Li et al. 2003; Raitakari et al. 2003; Davey Smith and Lynch 2005). These risk factors do not only affect coronary heart diseases in a mono-causal way, but they may also affect coronary heart disease by interacting with each other in order to increase or attenuate each other’s effects on the disease aetiology leading to coronary heart disease.
2 Historical Trends and Socioeconomic Mortality Differences in a Life Course and Cohort Perspective
The research area that concerns the mortality decline entails a number of important issues that can each contribute to the understanding of the modern mortality decline and its complexity. The eradication of smallpox mortality (Sköld 1996a, b) and the variations in sex differences in mortality (Willner 1999) have been thoroughly investigated and discussed. Another issue concerns socioeconomic mortality differences and socioeconomic differences in the short term as well as secular mortality decline. This socioeconomic gradient to this day remains apparent, despite the development of the modern welfare state and active policies to redistribute income in many countries, e.g. Sweden. In fact, during the past two decades, Sweden has witnessed a continuous decline in age specific mortality rates in most age intervals and a corresponding increase in life expectancy. This mortality decrease is observed in all socioeconomic groups in Swedish society. However, the decrease has been more pronounced in higher socioeconomic strata (high education, high income, non-manual employees in higher positions according to occupational status) than in lower socioeconomic strata, which has resulted in increasing socioeconomic differences in life expectancy in Sweden during the late 1980s, 1990s and early 2000s (National Public Health Report 2001, 2005).
It is often stated that socioeconomic mortality gradients, with the poor having worse health and increased risk of death compared to the rich, are ubiquitous phenomena, having always existed everywhere. This is an erroneous assumption, however (Davey Smith 2003). Reviewers (e.g., Macintyre 1998) often start with well-known historical examples, such as when Chadwick assembled data from different areas of Great Britain, and generalise to all situations. Chadwick’s data, however, did suggest large socioeconomic differences in mortality in the first decades of the nineteenth century in Britain. The socioeconomic differences existed within many UK locales, although the high socioeconomic position gentry and professional population only lived on average 35 years in Liverpool compared to 55 years in Bath. The corresponding average for the labourer and artisan class was 15 and 25 years, respectively (Chadwick 1842; Wohl 1983). Although data from Geneva indicate presence of socioeconomic mortality differences in pre-modern society (sixteenth century) (Perrenoud 1975) and data from an English township 1650–1830 also suggest permanent presence of socioeconomic mortality differences (King 1997), the generalisation by MacIntyre concerning the presence throughout history of socioeconomic differentials in mortality contrasts to important extent with the observation by Livi-Bacci (1991). According to Livi-Bacci, rudimentary older data from England suggest the absence of socioeconomic differentials in mortality in England from approximately 1550 to ca. 1750 (Livi-Bacci 1991). The data that Livi-Bacci refers to are calculations of life expectancy from demographic data on English peers (Hollingsworth 1977) compared with life expectancy of the total English population calculated from the Wrigley and Schofield reconstitution data (Wrigley and Schofield 1981). In fact, the ducal families in England seem to have had a somewhat lower life expectancy than peers in general as well as the general population during the period prior to 1750. This pattern remains even after the increased risk of violent causes of death (including the “Agincourt” factor, i.e. the death-in-combat factor) are taken into account (Hollingsworth 1957). Furthermore, the reigning families of Europe seem to have had a life expectancy of 34 years in the sixteenth century, 30.9 years in the seventeenth and 37.1 years in the eighteenth century, i.e. life expectancies which fairly well correspond with the life expectancies of the general population in the corresponding countries during the same period. In the city of Rouen, fluctuations in grain prices during the ancien régime had a similar effect in various social classes (Galloway 1987).
A similar pattern has been observed in the parishes in the Scanian Demographic Database in southern Sweden, where fluctuations in grain prices also had strong and similar effects in all social classes before the agrarian revolution in the early nineteenth century. In contrast, the onset and progress of the agrarian revolution resulted in both weaker associations between short-term fluctuations in grain prices and mortality. It also resulted in increasing socioeconomic differentials in the mortality response to fluctuations in grain prices, as the more prosperous segment of the population seems to have become much less exposed to the effects of the fluctuations (Bengtsson 2000, 2004). These observations seem to constitute further proof in support of the notion that social differences in mortality were small or absent. Furthermore, the observations support the notion that socioeconomic differences in mortality increased during the eighteenth century because of the agrarian revolution.
Sweden started to gather and record demographic and socioeconomic data (including mortality), different measures of socioeconomic position and, in many parishes, causes of death for the whole country already in 1749. Hence, it is possible to go further back in time in Sweden than in probably any other country in the investigation of reliable demographic and socioeconomic data in order to better understand the dynamics of socioeconomic differences in longevity.
One explanation for the lack of socioeconomic differences in mortality in the rudimentary data presented by, for example, Livi-Bacci for England, may be that epidemic and endemic infectious diseases dominated the disease and mortality panorama in the general population, which is certainly not the case today. In many pre-modern societies, population density seems to have been positively associated with mortality due to increased risk of disease (i.e. infectious disease) exposure in densely populated areas. For instance, the remarkable healthiness of many frontier settlements in colonial North America in spite of their comparatively primitive material living conditions must have been partly due to the infrequent contact with others (Wrigley et al. 1997). The virulence of many such epidemic and endemic infectious diseases, e.g. smallpox, malaria, plague, typhoid, tetanus, yellow fever, encephalitis and poliomyelitis, are not at all influenced (or only minimally affected) by nutritional factors such as total energy intake, nutritional contents of the food and physical habitus. Other infectious diseases such as typhus, diphteria, staphylococcus infections, streptococcus infections, influenza, syphilis and systemic worm infections are only affected by such nutritional factors to a limited or variable extent (Rotberg and Rabb 1985). This means that the upper socioeconomic strata (i.e. the nobility) must have been exposed to risks of disease and death from common infections prevailing at that time to the same extent as members of the lower social strata. In fact, as social contacts and networks of the upper strata most likely were more extensive than among the lower classes, the exposure in those groups may even have been higher than in the lower strata. As many of the infectious diseases mentioned above decreased in importance during the time period studied, all age-specific mortality rates declined and life expectancy increased. Consequently, other diseases and diagnoses more related to nutritional status and the protecting effects of higher socioeconomic position increased in relative importance as causes of morbidity and mortality, which would have served to increase socioeconomic differences in morbidity and mortality during the period under study. The result would be an increase in socioeconomic mortality differences and thus increased socioeconomic differentials in life expectancy.
In modern times, chronic diseases with long latent, asymptomatic phases between the induction/onset of the disease and the first symptoms dominate the patterns of morbidity and mortality in developed countries. Socioeconomic differences according to social characteristics such as occupational status, education and income are well-known and have been described extensively both in Sweden (National Public Health Report 2005) and other countries (Marmot 2004; Davey Smith et al. 1990; Kaplan and Keil 1993) regarding morbidity and mortality in a wide variety of diseases. A recent review of the literature on the association between socioeconomic circumstances during childhood and cause-specific mortality during adulthood shows similar results. Adverse socioeconomic conditions during childhood were positively associated with increased all-cause mortality (in 18 of 22 studies), overall cardiovascular mortality (in 5 of 9), coronary heart disease mortality (in 7 of 10), stroke (in 4 of 6), and accidents and violence (in 3 of 5 studies). No such associations were found for rheumatic heart disease mortality (only 1 study) and overall cancer mortality. For lung- and smoking-related cancer mortality, respiratory disease mortality, suicides, alcohol- and illegal drug-related mortality only few studies showing no associations or studies showing diverse results concerning the association between childhood socioeconomic circumstances and cause-specific mortality were demonstrated (Galobardes et al. 2004). It thus seems that the association between childhood socioeconomic circumstances and risk of cardiovascular diseases in adulthood is particularly important in explaining life course effects on adult mortality (Galobardes et al. 2006a, b).
In Sweden only a few studies concerning socioeconomic conditions in childhood and health in adulthood have been conducted, but new data sets have been developed (Stenberg et al. 2007). Birth order position within the same family had statistically significant consequences for the health and survival (overall mortality) over the life course (Modin 2002). Socioeconomic inequities in overweight seem to reflect the cumulative influence of multiple adverse circumstances experienced from adolescence to young adulthood (Novak et al. 2006). Several Swedish studies demonstrate statistically significant associations between disadvantaged socioeconomic conditions during childhood as well as adverse socioeconomic mobility, and aspects of cardiovascular diseases such as all-cause and overall cardiovascular mortality (Rosvall et al. 2006), coronary heart disease (Wamala et al. 2001), myocardial infarction (Hallqvist et al. 2004), and carotid atheroschlerosis (Rosvall et al. 2002). In one Swedish study, IQ in early childhood was found to be unrelated to adult cancer mortality (Batty et al. 2007). Childhood conditions such as family disruption and child abuse were found to be unrelated to adult sense of coherence (Krantz and Östergren 2004). The markedly few results from Sweden thus still seem to be consistent with other findings from the international literature.
3 Cohort Effects on Mortality and Mortality Predictions: Indicators and Models
A number of models exist to forecast future mortality in populations (Bengtsson and Keilman 2003). There are several reasons why these models should include a historical and long-term perspective on mortality and the development of age-specific mortality. First, living conditions, i.e. living standards and diet, public health institutions and medicine and other areas relevant for the physical well-being of the population, improve from one period to the next. Such changes in living conditions are termed period effects. Second, the health and remaining lifespan of people living today are determined not only by contemporary period factors but also by living conditions earlier in life. Living conditions during childhood may affect health in later life through cohort effects on mortality. Third, the prediction of future mortality calls for a multivariate approach, including not one but a multitude of factors to predict mortality. These factors include long-term early life factors (Bengtsson 2003).
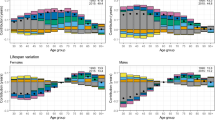
It thus seems obvious that early life and cohort factors should be included in the models when making predictions concerning future mortality. The crucial question is what indicators to use in order to assess how early life and cohort factors influence future mortality. The original work by Kermack and colleagues (1934) analysed the relationship between early life mortality, including infant (0–1 year) mortality, and its association with the age-specific mortality of different birth cohorts later during their life courses. Age-specific mortality is now commonly used as an indicator of mortality trends (United Nations 1999). Given the plausibility and scientific evidence for early life effects on cohort mortality presented earlier in this paper, age-specific mortality seems to be an obvious choice of indicator for making predictions concerning future mortality in a population when considering early life cohort effects. Infant mortality seems to be the most crucial measure of all age-specific mortality intervals in this respect (Bengtsson et al. 1998).
Fogel (1994) has used height as an indicator of early life effects on life expectancy and health in later life. In fact, recently both age-specific early life mortality (including infant mortality) and height have been demonstrated to be associated with mortality in later life using historical data from birth cohorts born before the twentieth century in four North European countries (Crimmins and Finch 2006).
Timing and specificity are key factors in life course epidemiology. Davey Smith and Lynch (2004) have pointed out that the mortality decrease in the three specific diseases respiratory tuberculosis, haemorrhagic stroke and bronchitis may have accounted for approximately two-thirds of the total decline in mortality for men and women aged 15–64 from the middle of the nineteenth century to the first decade of the twentieth century in Britain. Some other specific diseases including stomach cancer and rheumatic heart disease may account for some of the residual decline. These diseases have demonstrable influences from infancy and childhood, which have already been discussed. The timing for this time period when it comes to early life/cohort effects is also very good. Underlying factors such as decrease of child labour, increase in real wages, improved nutrition and increased height, a decrease in the proportion of working mothers, a decrease in family size, and improved housing conditions are also present for this period (Davey Smith and Lynch 2004). There is often a lack of such a high degree of specificity and timing in modern data. Specific exposures and outcomes should always be identified as well as the exact timing. The high availability of data in Sweden will plausibly make this task possible to accomplish in the years to come.
References
Barker, D. J. P. (1994). Mothers, babies, and disease in later life. London: British Medical Journal Publishing Group.
Barker, D. J. P. (1995). Fetal origins of coronary heart disease. British Medical Journal, 311, 171–174.
Barker, D. J. P. (1997). Fetal nutrition and cardiovascular disease in later life. In M. G. Marmot & M. E. J. Wadsworth (Eds.), Fetal and early childhood environment: Long-term health implications. British Medical Bulletin 53(1), 96–108.
Barker, D. J. P. (1998). Mothers, babies, and health in later life. London: Churchill Livingstone.
Barker, D. J. P. (2001). The malnourished baby and infant. British Medical Bulletin, 60, 69–80.
Batty, G. D., Modig Wennerstad, K., Davey Smith, G., Gunnell, D., Deary, I. J., Tynelius, P., & Rasmussen, F. (2007). IQ in early adulthood and later cancer risk: Cohort study of one million Swedish men. Annals of Oncology, 18(1), 21–28.
Bengtsson, T. (2000). Inequality in death: Effects of the agricultural revolution in southern Sweden, 1765–1865. In T. Bengtsson & O. Saito (Eds.), Population and economy. From hunger to modern economic growth (pp. 301–334). Oxford: Oxford University Press.
Bengtsson, T. (2003). The need for looking back in time when predicting future mortality trends. In T. Bengtsson & N. Keilman (Eds.), Perspectives on mortality forecasting (Social Insurance Studies, No. 1: Current Practice) (pp. 87–97). Stockholm: Swedish National Insurance Board.
Bengtsson, T. (2004). Mortality and social class in four Scanian Parishes, 1766–1865. In T. Bengtsson, C. Campbell, J. Z. Lee, et al. (Eds.), Life under pressure. Mortality and living standards in Europe and Asia, 1700–1900 (pp. 135–172). Cambridge, MA: MIT Press.
Bengtsson, T., & Keilman, N. (Eds.). (2003). Perspectives on mortality forecasting (Social Insurance Studies, No. 1: Current Practice). Stockholm: Swedish National Insurance Board.
Bengtsson, T., & Lindström, M. (2000). Childhood misery and disease in later life: The effects on mortality in old age of hazards experienced in early life, southern Sweden, 1760–1894. Population Studies, 54, 263–277.
Bengtsson, T., & Lindström, M. (2003). Airborne infectious diseases during infancy and mortality in later life in southern Sweden, 1766–1894. International Journal of Epidemiology, 32, 286–294.
Bengtsson, T., Saito, O., Reher, D., & Campbell, C. (1998). Population and the economy: From hunger to modern economic growth. In C.-E. Núñez (Ed.), Debates and controversies in economic history (pp. 69–143). Madrid: Editorial de Estudios Ramon Areces, SA.
Ben-Shlomo, Y., & Kuh, D. (2002). A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology, 31, 285–293.
Berenson, G. S., Srinivasan, S. R., Freedman, D. S., Radhakrishnamurthy, B., & Jr Dalferes, E. R. (1987). Atheroschlerosis and its evolution in children. American Journal of Medical Science, 294, 429–440.
Blackwell, D. L., Hayward, M. D., & Crimmins, E. M. (2001). Does childhood health affect chronic morbidity in later life? Social Science and Medicine, 52, 1269–1284.
Cadwgan, A. M., Watson, W. A., Laing, R. B., MacKenzie, A. R., Smith, C. C., & Douglas, J. G. (2000). Presenting clinical features and C-reactive protein in the prediction of a positive stool culture in patients with diarrhoea. Journal of Infection, 41(2), 159–161.
Chadwick, E. (1842). Report of an enquiry into the sanitary conditions of the Labouring population of Great Britain. London: Poor Law Commission.
Crimmins, E. M., & Finch, C. E. (2006). Infection, inflammation, height and longevity. Proceedings of the National Academy of Sciences of the United States of America, 103(2), 498–503.
Curtis, S. M. (2004). Nutrition and scarlet fever mortality during the epidemics of 1860–1890: The Sundsvall region. Social History of Medicine, 17(2), 199–221.
Davey Smith, G. (2003). Health inequalities: Lifecourse approaches. Bristol: Policy Press.
Davey Smith, G., & Kuh, D. (2001). William Ogilvy Kermack and the childhood origins of adult health and disease. International Journal of Epidemiology, 30, 696–703.
Davey Smith, G., & Lynch, J. (2004). Commentary: Social capital, social epidemiology and disease aetiology. International Journal of Epidemiology, 33, 691–700.
Davey Smith, G., & Lynch, J. (2005). Lifecourse influences on coronary heart disease. In M. Marmot & P. Elliott (Eds.), Coronary heart disease epidemiology: From aetiology to public health. Oxford: Oxford University Press.
Davey Smith, G., Shipley, M. J., & Rose, G. (1990). Magnitude and causes of socioeconomic differentials in mortality: Further evidence from the Whitehall Study. Journal of Epidemiology and Community Health, 44, 265–270.
Davey Smith, G., Leary, S., & Ness, A. (2006). Could dehydration in infancy lead to high blood pressure? Journal of Epidemiology and Community Health, 60, 142–143.
Doblhammer, G. (1999). Longevity and month of birth: Evidence from Austria and Denmark (Demographic Research, Vol. 1(3)). Rostock: Max Planck Institute for Demographic Research.
Doblhammer, G. (2002). Differences in life-span by month of birth for the United States: The impact of early life events and conditions on late life mortality (MPIDR Working Paper WP 2002–019). Rostock: Max-Planck Institute for Demographic Research.
Doblhammer, G. (2008). The month of birth: Evidence for declining but persistent cohort effects in lifespan. In T. Bengtsson (Ed.), Perspectives on mortality forecasting (Social Insurance Studies, No. 5: Cohort factors: How conditions in early life influence mortality later in life). Stockholm: Swedish Social Insurance Agency.
Doblhammer, G., & Vaupel, J. W. (2001). Lifespan depends on month of birth. Proceedings of the National Academy of Sciences of the United States of America, 98(5), 2934–2939.
Finch, C. E., & Crimmins, E. M. (2004). Inflammatory exposure and historical changes in human life-spans. Science, 305, 1736–1739.
Fogel, R. W. (1994). The relevance of Malthus for the study of mortality today: Long-run influences on health, mortality, labour-force participation and population growth. In K. Lindvall & H. Landberg (Eds.), Population, economic development and the environment. The making of our common future (pp. 231–284). Oxford/New York: Oxford University Press.
Fridlizius, G. (1989). The deformation of cohorts. Nineteenth-century mortality in a generational perspective. Scandinavian Economic History Review, 37(3), 3–17.
Galloway, P. R. (1987). Population, prices and weather in preindustrial Europe. Berkeley: University of California.
Galobardes, B., Lynch, J. W., & Davey Smith, G. (2004). Childhood socioeconomic circumstances and cause-specific mortality in adulthood: Systematic review and interpretation. Epidemiologic Reviews, 26, 7–21.
Galobardes, B., Davey Smith, G., Jeffreys, M., & McCarron, P. (2006a). Childhood socioeconomic circumstances predict specific causes of death in adulthood: The Glasgow student cohort study. Journal of Epidemiology and Community Health, 60, 527–529.
Galobardes, B., Smith, G. D., & Lynch, J. W. (2006b). Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Annals of Epidemiology, 16, 91–104.
Hall, A. J., & Peckham, C. S. (1997). Infections in childhood and pregnancy as a cause of adult disease – Methods and examples. In M. G. Marmot & M. E. J Wadsworth (Eds.), Fetal and early childhood environment: Long-term health implications. British Medical Bulletin, 53(1), 10–23.
Hallqvist, J., Lynch, J. W., Bartley, M., Lang, T., & Blane, D. (2004). Can we disentangle life course processes of accumulation, critical period and social mobility? Social Science and Medicine, 58(8), 1555–1562.
Harvey, R. F., Spence, R. W., Lane, J. A., Nair, P., Murray, L. J., Harvey, I. M., & Donovan, J. (2002). Relationship between the birth cohort pattern of Helicobacter pylori infection and the epidemiology of duodenal ulcer. Quarterly Journal of Medicine, 95(8), 519–525.
Heslop, P., Smith, G. D., Macleod, J., & Hart, C. (2001). The socioeconomic position of women, risk factors and mortality. Social Science and Medicine, 53, 477–485.
Hollingsworth, T. H. (1957). A demographic study of the British ducal families. Population Studies, 11(1), 4–26.
Hollingsworth, T. H. (1977). A note on the medieval longevity of the secular peerage. Population Studies, 29(1), 157.
Hunter, R. J., Patel, V. B., Miell, J. P., Wong, H. J., Marway, J. S., Richardson, P. J., & Preedy, V. R. (2001). Diarrhea reduces the rates of cardiac protein synthesis in myofibrillar protein fractions in rats in vivo. Journal of Nutrition, 131, 1513–1519.
Kannisto, V., Christensen, K., & Vaupel, J. W. (1997). No increased mortality in later life for cohorts born during famine. American Journal of Epidemiology, 145(11), 987–994.
Kaplan, G., & Keil, J. E. (1993). Socioeconomic factors and cardiovascular disease: A systematic review of the literature. Circulation, 88, 1973–1998.
Kermack, W. O., McKendrick, A. G., & McKinlay, P. L. (1934, March). Death rates in Great Britain and Sweden: Some regularities and their significance. Lancet, 223, 698–703.
King, S. (1997). Dying with style: Infant death and its context in a rural industrial township 1650–1830. Social History of Medicine, 10(1), 3–24.
Krantz, G., & Östergren, P. O. (2004). Does it make sense in a coherent way? Determinants of sense of coherence in Swedish women 40 to 50 years of age. International Journal of Behavioral Medicine, 11(1), 18–26.
Kuh, D., & Ben-Shlomo, Y. (1997). A life course approach to chronic disease epidemiology. Tracing the origins of ill-health from early to adult life. Oxford: Oxford University Press.
Kuh, D., & Ben-Shlomo, Y. (2004). A life course approach to chronic disease epidemiology. Tracing the origins of ill-health from early to adult life (2nd ed.). Oxford: Oxford University Press.
Kuh, D., & Hardy, R. (2002). A life course approach to Women’s health. Oxford: Oxford University Press.
Lawlor, D. A., Davey Smith, G., Mitchell, R., & Ebrahim, S. (2006). Adult blood pressure and climate conditions in infancy: A test of the hypothesis that dehydration in infancy is associated with higher adult blood pressure. American Journal of Epidemiology, 163, 608–614.
Lawn, S. D., Obeng, J., Acheampong, J. W., & Griffin, G. E. (2000). Resolution of the acute phase response in West African patients receiving treatment for pulmonary tuberculosis. International Journal of Tuberculosis and Lung Disorders, 4(4), 340–344.
Li, X., Kolltveit, K. M., Tronstad, L., & Olsen, I. (2000). Systemic diseases caused by oral infection. Clinical Microbiology Review, 13(4), 547–558.
Li, S., Chen, W., Srinivasan, R. S. R., Bond, M. G., Tang, R., Urbina, E. M., & Berenson, G. S. (2003). Childhood cardiovascular risk factors and carotid vascular changes in adulthood: The Bogalusa Heart Study. Journal of the American Medical Association, 290, 2271–2276.
Livi-Bacci, M. (1991). Population and nutrition. An essay on European demographic history. Cambridge: Cambridge University Press.
Macintyre, S. (1998). Social inequalities and health in the contemporary world: Comparative overview. In S. Strickland & P. S. Shetty (Eds.), Human biology and social inequality (Symposia of the Society for the Study of Human Biology). Cambridge: Cambridge University Press.
Marmot, M. (2004). Status syndrome. How your social standing directly affects your health. London: Bloomsbury.
Marmot, M., & Elliot, P. (Eds.). (2005). Coronary heart disease epidemiology. From Aetiology to public health (2nd ed.). Oxford: Oxford University Press.
Modin, B. (2002). Birth order and mortality: A life-long follow-up of 14,200 boys and girls born in early 20th century Sweden. Social Science and Medicine, 54(7), 1051–1064.
Moore, S. E., Cole, T. J., Poskitt, E. M. E., Sonko, B. J., Whitehead, R. G., McGregor, I. A., & Prentice, A. M. (1997). Season of birth predicts mortality in rural Gambia. Nature, 388, 434.
Moore, S. E., Fulford, A. J. C., Streatfield, P. K., Persson, L. Å., & Prentice, A. M. (2004). Comparative analysis of patterns of survival by season of birth in rural Bangladeshi and Gambian populations. International Journal of Epidemiology, 33, 137–143.
National Public Health Report. (2001). Stockholm: National Board on Health and Welfare.
National Public Health Report. (2005). Stockholm: National Board on Health and Welfare.
Novak, M., Ahlgren, C., & Hammarström, A. (2006). A life-course approach in explaining social inequity in obesity among young adult men and women. International Journal of Obesity, 30(1), 191–200.
Omran, A. R. (1971). The epidemiologic transition. A theory of the epidemiology of population change. The Milbank Memorial Fund Quarterly, 49, 509–538.
Perrenoud, A. (1975). L’inégalité sociale devant la mort à Genève au XVIIIème siècle. Population, 30(Special number), 239.
Preston, S. H., Hill, M. E., & Drevenstedt, G. L. (1998). Childhood conditions that predict survival to advanced ages among African-Americans. Social Science and Medicine, 47, 1231–1246.
Raitakari, O. T., Juonala, M., Kähönen, M., Taittonen, L., Laitinen, T., Mäki-Torkko, N., Järvisalo, M. J., Uhari, M., Jokinen, E., Rönnemaa, T., Åkerblom, H. K., & Viikari, J. S. A. (2003). Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The cardiovascular risk in young Finns Study. Journal of the American Medical Association, 290, 2277–2283.
Riley, J. C. (2001). Rising life expectancy. A global history. Cambridge: Cambridge University Press.
Rosvall, M., Östergren, P. O., Hedblad, B., Isacsson, S. O., Janzon, L., & Berglund, G. (2002). Life-course perspective on socioeconomic differences in carotid atheroschlerosis. Artherioschlerosis, Thrombosis and Vascular Biology, 22(10), 1704–1711.
Rosvall, M., Chaix, B., Lynch, J. W., Lindström, M., & Merlo, J. (2006). Similar support for three different life course socioeconomic models on predicting premature cardiovascular mortality and all-cause mortality. BioMed Central Public Health, 6, 203.
Rotberg, R. I., & Rabb, T. K. (1985). The relationship of nutrition, disease, and social conditions: A graphical presentation. In R. I. Rotberg & T. K. Rabb (Eds.), Hunger and history. The impact of changing food patterns and society. Cambridge/London: Cambridge University Press.
Shaheen, S. (1997). The beginnings of chronic airflow obstruction. In: M. G. Marmot & M. E. J. Wadsworth (Eds.), Fetal and early childhood environment: Long-term health implications. British Medical Bulletin, 53(1), 58–70.
Simondon, K. B., Elguero, E., Marra, A., Diallo, A., Aaby, P., & Simondon, F. (2004). Season of birth is not associated with risk of early adult death in rural Senegal. International Journal of Epidemiology, 33, 130–136.
Sköld, P. (1996a). The two faces of smallpox: A disease and its prevention in eighteenth and nineteenth century Sweden. Thesis, Umeå University, Umeå.
Sköld, P. (1996b). From inoculation to vaccination: Smallpox in Sweden in the eighteenth and nineteenth centuries. Population Studies, 50, 247–262.
Stenberg, S. A., Vågerö, D., Österman, R., Arvidsson, E., von Otter, C., & Janson, C. G. (2007). Stockholm Birth Cohort Study 1953–2003: A new tool for life-course studies. Scandinavian Journal of Public Health, 35(1), 104–110.
Strachan, D. P. (1997). Respiratory and allergic diseases. In D. Kuh & Y. Ben-Shlomo (Eds.), A life course approach to chronic disease Epidemiology. Tracing the origins of ill-health from early to adult life (pp. 101–120). Oxford: Oxford Medical Publications.
Strong, J. P., Malcom, G. T., McMahan, C. A., Tracy, R. E., Newman, W. P., III, Herdrick, E. E., & Cornhill, J. F. (1999). Prevalence and extent of atheroschlerosis in adolescents and young adults: Implications for prevention from the pathobiological determinants of atheroschlerosis in Youth Study. Journal of the American Medical Association, 281, 727–735.
Suomi, S. J. (1997). Early determinants of behaviour: Evidence from primate studies. In M. E. Marmot & M. E. J. Wadsworth (Eds.), Fetal and early childhood environment: Long-term health implications. British Medical Bulletin, 53(1), 170–184.
Timpson, N. J., Lawlor, D. A., Harbord, R. M., Gaunt, T. R., Day, I. N. M., Palmer, L. J., Hattersley, A. T., Ebrahim, S., Lowe, G. D. O., Rumley, A., & Davey Smith, G. (2005). C-reactive protein and its role in metabolic syndrome: Mendelian randomisation study. Lancet, 366, 1954–1959.
United Nations. (1999). World population prospects. The 1998 revision. Volume I: Comprehensive Tables, ST/SER.A/177. New York: United Nations.
von Mutius, E. (2001). Paediatric origins of adult lung disease. Thorax, 56, 153–156.
Wamala, S., Lynch, J. W., & Kaplan, G. A. (2001). Women’s exposure to early and later life socioeconomic disadvantage and coronary heart disease risk: The Stockholm Female Coronary Risk Study. International Journal of Epidemiology, 30(2), 275–284.
Willner, S. (1999). Det svaga könet? Kön och vuxendödlighet i 1800-talets Sverige. Linköping: Linköping University.
Wohl, A. S. (1983). Endangered lives: Public health in Victorian Britain. London: JM Dent.
Wrigley, E. A., & Schofield, R. (1981). The population history of England 1541–1871: A reconstruction. Cambridge: Cambridge University Press.
Wrigley, E. A., Davies, R. S., Oeppen, J. E., & Schofield, R. S. (1997). English population history from family reconstitution 1580–1837. Cambridge: Cambridge University Press.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Lindström, M., Smith, G.D. (2019). A Life Course Perspective to the Modern Secular Mortality Decline and Socioeconomic Differences in Morbidity and Mortality in Sweden. In: Bengtsson, T., Keilman, N. (eds) Old and New Perspectives on Mortality Forecasting . Demographic Research Monographs. Springer, Cham. https://doi.org/10.1007/978-3-030-05075-7_21
Download citation
DOI: https://doi.org/10.1007/978-3-030-05075-7_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-05074-0
Online ISBN: 978-3-030-05075-7
eBook Packages: Social SciencesSocial Sciences (R0)