Abstract
Over the last two decades, small interfering RNA (siRNA)-mediated gene silencing has quickly become one of the most powerful techniques used to study gene function in vitro and a promising area for new therapeutics. Delivery remains a significant impediment to realizing the therapeutic potential of siRNA, a problem that is also tied to immunogenicity and toxicity. Numerous delivery vehicles have been developed, including some that can be categorized as pseudovirions: these are vectors that are directly derived from viruses but whose viral coding sequences have been eliminated, preventing their classification as viral vectors. Characteristics of the pseudovirions discussed in this review, namely phagemids, HSV amplicons, SV40 in vitro-packaged vectors, influenza virosomes, and HVJ-Envelope vectors, make them attractive for the delivery of siRNA-based therapeutics. Pseudovirions were shown to deliver siRNA effector molecules and bring about RNA interference (RNAi) in various cell types in vitro, and in vivo using immune-deficient and immune-competent mouse models. Levels of silencing were not always determined directly, but the duration of siRNA-induced knockdown lasted at least 3 days. We present examples of the use of pseudovirions for the delivery of synthetic siRNA as well as the delivery and expression of DNA-directed siRNA.
Similar content being viewed by others
INTRODUCTION
Principles of RNA Interference
RNA interference (RNAi) is a process in which the presence of double-stranded RNA (dsRNA) induces the selective and catalytic degradation of the homologous mRNA by endogenous cell machinery. Since being identified in Caenorhabditis elegans by Fire and coworkers in 1998 (1), RNAi has since been extensively studied and is now known to exist in plants, animals, and insects. Numerous reviews detail the mechanisms of action of RNAi (2–4) and the ways in which RNAi has been developed and exploited to achieve efficient knockdown of genes both in vitro and in vivo (5–11). Briefly, long dsRNA or hairpin RNA is processed by the endonuclease Dicer into smaller RNA fragments. These small RNA fragments, termed small interfering RNA (siRNA), are separated into single strands and then loaded into the multi-component RNA-Induced Silencing Complex (RISC). The siRNA within the RISC complex serves as a template to guide the selective cleavage of the complementary mRNA. The cleaved mRNA, which has two unprotected ends, is highly susceptible to degradation by nucleases. A similar process takes place with microRNA (miRNA) that, like siRNA, is the product of dsRNA that has been cleaved by Dicer. A key difference is that microRNAs are typically endogenously produced and regulate the translation of mRNAs to which they have partial complementarity; by contrast, siRNAs, either directly introduced into the cell or generated from long dsRNA as products of Dicer, are fully complementary to the target mRNA and bring about complete mRNA degradation.
Considerations for siRNA Effector Molecules
siRNA is the effector molecule of RNAi that has received the most attention by far, and the use of siRNA in investigations to knockdown gene expression is now fairly common. Nevertheless, there are still many factors that must be considered when designing and using siRNA, such as target sequence, sequence length, overhangs, and secondary structure. siRNA effector molecules exist in several forms; siRNA can be delivered as single-stranded oligomers, doublestranded duplexes, RNA hairpins or other forms (reviewed by Amarzguioui et al. (12)). There are also a number of concerns related to the inherent immunogenicity of RNA in vivo that must be considered. Long dsRNA molecules are well-known to activate an innate anti-viral response, primarily through interferon (IFN) induction and the secretion of inflammatory cytokines. Short siRNAs, however, have also been shown to induce IFN responses through both sequence-dependent and sequence-independent mechanisms (reviewed by Judge and Maclachlan (13), Behlke (14), and references therein). Sequence-dependent mechanisms include activation of toll-like receptors (TLR) 7 and 8, which are present in endosomes. Many siRNA delivery systems, including some discussed here, rely on endocytotic uptake, so the siRNA they carry passes through endosomes where these RNA-sensing receptors are localized. TLR7 and 8 recognize specific sequences of both ssRNA and dsRNA, which ultimately leads to the secretion of a number of cytokines and IFN subtypes. However, not all cell types are activated to the same extent. Sequence-independent mechanisms include recognition of dsRNA and subsequent generation of IFN responses by TLR3, dsRNA binding protein kinase (PKR), 2′,5′-oligoadenylate synthetase 1 (OAS1), and retinoic acid-inducible gene-1 (RIG-1).
Because RNA is highly susceptible to degradation, the effects of siRNA are transient. One strategy to address this has been to introduce chemical modifications to the siRNA structure to confer heightened stability to the siRNA, thereby lengthening the time it is able to exert its effect. By replacing phosphodiester linkages with phosphorothioates or boranophosphates, or by modifying the 2′ position of the ribose ring, greater resistance to degradation by nucleases has been achieved, resulting in an increased serum half-life and greater potency (Behlke (14) and references therein). There is evidence that chemical modifications can also modulate the immunostimulatory properties of siRNA without affecting efficacy (13). Another common strategy to achieve longer-term silencing is to deliver DNA plasmid vectors that generate short hairpin RNA (shRNA), which is processed by Dicer in the cell to yield siRNA (DNA-directed siRNA) (15). As with the direct application of RNA molecules, thought must be given to the possible sequence-specific effects of any shRNA, and subsequent siRNA, generated from the expression of the plasmid in the cell.
PSEUDOVIRIONS AS A CLASS OF DELIVERY VEHICLES
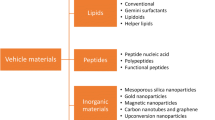
One of the obstacles to the therapeutic use of siRNA is that of delivery. Some aspects of delivery include targeted delivery into various cell types, transducing dividing and quiescent cells, and crossing the blood-brain barrier. Numerous approaches to siRNA delivery have been developed to date, and broad categories include physical methods, viral vectors, and non-viral vectors. One interesting subset of delivery vehicles includes those that are directly derived from viruses but whose characteristics prevent them from being classified as viral and whose origins make them distinctly different from other types of non-viral vectors such as liposomes or polymer-based complexes. These pseudoviral particles, or pseudovirions, are vectors in which key structural elements of viruses are used or repurposed to deliver a cargo other than the original viral genetic material.
A successful delivery vehicle must be able to both efficiently deliver as well as protect the cargo. Pseudovirions are useful delivery vehicles because they combine the most appealing features of viral and non-viral systems. Viral vectors are attractive because viruses have evolved to deliver their genetic material very efficiently to cells, and the vectors are capable of achieving long-term expression. However, there are a number of safety concerns linked with virus-based therapies, such as the immunogenic nature of viruses and the potential for recombination and non-specific integration into the host genome. Viral vectors also often have a limited capacity and are difficult to retarget. By contrast, non-viral vectors, such as liposomes, are usually non-immunogenic and are easy to prepare and modify quickly. However, they often suffer from poor transfection efficiency. Pseudovirions have the advantage of being virally derived and so often have efficient delivery with defined uptake mechanisms. Like non-viral vectors, pseudovirions are generally easy to modify and produce.
Pseudoviral Delivery: Trans-packaging and Viral Envelope Systems
We present below several examples of pseudoviral vectors that have been developed and used in RNAi applications. These selected examples can serve as an overview of pseudovirions as delivery vehicles. Two general types of pseudoviral systems are described. First are trans-packaging systems in which viral machinery and proteins have been repurposed to package genetic material other than the original viral genome. These include phagemid particles, Herpes Simplex Virus-1 amplicons, and SV40 in vitro-packaged vectors. These vectors are distinguished from recombinant viral vectors in that they contain no coding viral sequences and at most carry the non-coding sequences necessary for packaging. Second are the viral envelope systems, in which native enveloped virus particles are inactivated and used to package other cargos. For each pseudovirion, a short introduction to the originating viral entity is given, followed by details of pseudovirion preparation and examples from the literature. Finally, advantages, disadvantages, and concerns are highlighted for each pseudoviral system.
Phagemid Particles for the Delivery of DNA-Directed siRNA in Mammalian Cells
Bacteriophage and Phagemid Particles
Bacteriophages (phages) are viruses that infect bacteria. Over the last two decades, phage derivatives and technologies have been developed for a wide variety of applications. One example is phagemids. The properties of phagemids were first explored in the 1980s (16,17), and they were used as cloning and sequencing vectors (18). Phage-display is a closely related technology in which phages are engineered to present recombinant protein libraries on their surface, and this method has been used to develop and select highly specific peptides and antibody fragments against a variety of targets (for a review, see Kehoe and Kay (19)). The M13 filamentous phage has been extremely well-characterized (20) and is one of the phages most commonly used as a base for these technologies. This phage is rod-like in shape and has five coat proteins that assemble around the circular, single-stranded DNA (ssDNA) phage genome. The length of the phage is proportional to the size of the genome, and for a wild-type phage whose genome is between 5–8 kb, the mature phage is 6 nm wide and 800–2000 nm long. Genomes as large as 12 kb can also be packaged (20). One of the minor coat proteins, pIII, makes up part of the cap on the end of the M13 virion and is the protein that has been most successfully modified to present recombinant proteins in phage-display applications. Uptake of phage in mammalian cells is achieved via receptor-mediated endocytosis through the use of targeted ligands displayed on the phage surface (21).
Phagemid Components and Preparation
Phagemids are plasmid vectors that can be transformed and propagated in bacteria. Unlike conventional plasmid vectors, phagemids contain elements that cause them to be packaged into phage capsids as ssDNA when the phagemid-transformed bacteria are superinfected by helper phage, resulting in phagemid particles (19). These essential elements typically include an antibiotic resistance marker, bacterial replication of origin, and a phage origin of replication, which is also important for packaging. Helper phage are bacteriophages whose genomes have been modified such that they provide all the proteins necessary to generate new phage, but are themselves very inefficiently packaged in the presence of phagemid vectors that carry optimal packaging signals (phage origin of replication). An alternative method for phagemid particle preparation is to transform the phagemid vector into bacteria that have been previously transformed with a helper phage genome (22,23). A schematic of these two preparation methods is shown in Fig. 1.
Methods of phagemid particle preparation. Phagemids are plasmid vectors containing an shRNA cassette, an antibiotic resistance marker (e.g., Ampr), a phage origin of replication (e.g., f1 ori), and a bacterial origin of replication (e.g., ColE1 ori). Phagemid vectors are transformed into bacteria and then amplified. Transformed bacteria are superinfected with a helper phage that provides the proteins required for packaging, including an EGF-modified version of the pIII minor coat protein. The helper phage carries a defective phage origin of replication and so is inefficiently packaged in the presence of phagemid vectors that carry an optimal packaging signal. Phagemid vectors are packaged as circular single-stranded DNA into phagemid particles. Alternatively, bacteria are transformed with a helper phage genome to generate bacteria that express the phage proteins necessary for packaging (bacterial packaging cells, LMP). LMP cells are transformed with phagemid vector, and then the phagemid vector is amplified and packaged into phagemid particles.
In Vitro Delivery of Phagemids Expressing shRNA
The field of phagemid-mediated transgene and siRNA delivery is currently in its infancy. However, we present two examples demonstrating the ability of phagemid particles to deliver plasmids which generate shRNA in mammalian cells.
Recently, Jiang et al. (24) were able to knock down the expression of enhanced green fluorescent protein (EGFP) and the oncogene AKT1, coding for a serine-threonine protein kinase, in NCI-H1299 (large-cell lung carcinoma) cells in vitro using epidermal growth factor (EGF)-displaying phagemid particles and RNAi, in the presence of the topoisomerase I inhibitor hydroxycamptothecin (HCPT). Using pSilencer plasmids designed to generate shRNA against either EGFP or AKT1, they created phagemids that were effectively packaged into phagemid particles in E. coli transformed with the EGF-pIII-encoding helper phage genome, M13KO7EGFCT. The gene encoding pIII in this helper phage genome has been modified such that the minor coat protein expressed is a pIII-EGF fusion protein (22). Because these phagemid particles expressed EGF on their surface, they could be taken up via receptor-mediated endocytosis by mammalian cells to which they otherwise have no natural tropism.
Jiang et al. used their phagemid encoding siRNA against EGFP to estimate the transduction efficiency of their system. Cells were transfected with EGFP and then 12 h later transduced with 1011 plaque-forming units per ml of phagemid particles. At 24 h after transduction, HCPT was added to a final concentration of 2.5 µM. When assayed 48 h after transduction, the percentage of EGFP-positive cells in H1299 cells treated with siEGFP phagemid particles and 2.5 µM HCPT was reduced to approximately 50% of the control cells that had been treated with phagemid particles carrying an empty pSilencer vector.
Jiang and coworkers also achieved a 50–60% knockdown in the expression of AKT1 72 h after transduction, as determined by Western blotting, using siAKT phagemids. Untransduced cells and a mock control phagemid that differed from the siAKT sequence by only one nucleotide were used for comparison. Knockdown of AKT1 protein expression was dependent on the phagemid particle dose and required the presence of HCPT. The level of knockdown observed using the highest dose of siAKT phagemid particles was comparable to that observed when the corresponding non-phagemid siAKT vector (i.e., the same siRNA expression vector without the F1 origin sequence that is essential for phagemid packaging by helper phage) was transfected into H1299 cells using Lipofectamine™ 2000 (Invitrogen), a common nucleic acid transfection reagent. Despite the significant reduction in AKT1 protein expression, Jiang et al. did not observe significant inhibition of cell growth, which they posit may be a result of the stimulatory nature of the EGF ligands present on the phagemid particles.
In related work by Cai et al. (25), the same methodology was used to construct a phagemid-encoding shRNA against focal adhesion kinase, which was subsequently packaged into EGF-displaying phagemid particles using E. coli transformed with M13KO7EGFCT. Focal adhesion kinase (FAK) is a non-receptor tyrosine kinase that has been shown to be a key component in the regulation of cell survival, proliferation, and migration, and appears to play an important role in tumorigenesis and metastasis, making it an attractive target for cancer therapy (26). siFAK-encoding phagemid particles in conjunction with HCPT treatment significantly reduced the expression of FAK in H1299 cells, inhibited cell invasiveness in a transwell invasion assay by approximately 50%, and reduced colony formation by 54% compared to control groups. While MTT cell growth assays showed after 72 h that HCPT and HCPT + mock siRNA phagemid particles reduced cell growth by 12–19%, the growth of cells treated with siFAK phagemid particles and HCPT was reduced by 52–61% compared to untreated cells (25).
Concerns and Outlook for Phagemid Particles
In both of these examples of siRNA-encoding phagemid particles, significant knockdown was only seen in the presence of HCPT, a topoisomerase I inhibitor that is also used as an anti-cancer treatment. While it has been shown that genotoxic treatments can increase gene delivery, the mechanism is not completely understood (27,28). This seeming requirement for co-treatment with HCPT to achieve significant knockdown may pose an obstacle for the further development of these vectors.
Additionally, the authors of both studies make only qualitative statements about the degree of contaminating helper phage in their phagemid particle stocks, saying that “almost all of the DNA packaged” was phagemid DNA (24,25). In both studies, E. coli were transformed with a helper phage genome as reported by Li et al. (22) and used to generate phagemid particles, yet contaminating helper phage was still present. By contrast, Chasteen and co-workers reported that helper-free phagemid preparations were achieved using a conceptually similar system, i.e., one using cells transformed with an engineered helper phage genome (23). Given these conflicting reports, and because of the prevalence of similar problems in other helper virus systems, it is unclear whether helper-free phagemid preparations are an impossibility or if they can be achieved through careful design and engineering of the phagemid and helper phage genome.
Pharmacokinetics is another important consideration for the use of phage-derived technologies in vivo. Bacteriophage are known to be rapidly cleared from the circulatory system of mammals. However, circulation time is dependent on the type of phage used and the peptides displayed on its surface; work by several groups has shown that modification of the phage coat proteins can dramatically improve the serum half-life of phages (29–33).
Phagemid particles are an attractive delivery vehicle because, unlike animal viruses, bacteriophages exhibit no natural tropism toward mammalian cells and, by virtue of their ligand display properties, have the potential to be developed as highly specific, targeted vectors. The ability to generate targeted ligands quickly through phage-display technology and directed evolution is well-known, and while not always dramatic, results showing that phage-derived vectors can be targeted toward mammalian cells are promising (19,27,28,34–38).
Herpes Simplex Virus Type-1 Amplicon Vectors for Delivery of shRNA In Vitro and In Vivo
Properties of Herpes Simplex Virus-1
Herpes Simplex Virus-1 (HSV-1) has been used to develop another pseudoviral system, the HSV amplicon. HSV-1 is a member of the Alphaherpesvirinae subfamily of Herpesviruses. Wild-type HSV-1 is an enveloped virus whose attachment is mediated first by the interactions of envelope glycoproteins gB and gC with heparin sulfate on the cell surface. This is followed by binding of envelope glycoprotein gD with heparin sulfate, herpes virus entry mediator (HVEM), or nectins, which leads to fusion of the viral envelope with the cell membrane (39). Because these receptors are widely expressed, HSV-1 has wide tropism for neuronal, as well as epithelial, cells.
The size of the native HSV-1 genome is 150 kb; it encodes numerous immediate-early, early, and late gene products. Several of its immediate-early gene products, including ICP0, ICP27, ICP4, and ICP22 are involved in the regulation of viral gene expression (39). More than 40% of adults possess antibodies against HSV-1 (40) and potentially harbor latent infections. In its latent state, the HSV-1 genome is maintained episomally in neurons.
Essential Elements of Herpes Simplex Virus-1 Amplicons
Herpes Simplex Virus-1 amplicons (HSV amplicons) were initially developed as amplifying and cloning vectors (41) and, like phagemid particles, are an example of a trans-packaging system. Amplicon plasmids contain two key elements, namely the viral origin of replication (ori) and the DNA cleavage/packaging signal (pac), and comprise the base of the system. HSV amplicons are helper-dependent vectors. When helper functions are supplied in trans by one of the various helper systems (described below), the amplicon plasmid is replicated and amplified as ~150 kb head-to-tail concatamers of linear DNA and is packaged into particles. The particles are structurally identical to wild-type HSV-1 viral particles, i.e., DNA associated with core proteins, surrounded by an icosohedral nucleocapsid, tegument, and viral envelope. The resulting amplicon vector contains only the linear concatameric form of the plasmid and does not contain any HSV coding sequences (42). Amplicon vectors make use of the inherent, large 150 kb capacity of HSV-1 virions. For example, an HSV amplicon resulting from a 5 kb amplicon plasmid will carry a linear DNA with 30 tandem repeats of the plasmid sequence and transgene, whereas a 150 kb amplicon plasmid will result in an HSV amplicon vector that carries only one repeat (43). The ability of amplicon plasmids to carry such long segments of DNA allows for entire regulatory sequences of the exogenous gene to be accommodated.
Because the only viral sequences HSV amplicons carry are the ori and pac, several systems have been designed to provide the viral genes essential for replication and packaging. At their inception, HSV amplicon systems relied on a replication-deficient helper virus to provide these functions (41,43). Similar to the phagemid system, eukaryotic cells were transfected first with the amplicon plasmid and then superinfected with HSV helper viruses. These preparations invariably had high levels of contaminating helper virus that were cytotoxic. Later, the work of Geller and Breakefield (44) demonstrated that by using a replication-defective and temperature-sensitive mutant of HSV as the helper virus to prepare the amplicon stocks, transgene expression could be achieved in rat neurons while generating only low levels of replication-competent helper virus in the transduced cells (less than 10 plaque-forming units per ml).
The next advance towards developing a helper-free packaging system was a set of five overlapping cosmids that together cover the entire HSV genome, but with the packaging signals removed, which supply all of the HSV genes needed for replication and packaging (45,46). This system required that cells be transfected with the entire set of cosmids in addition to the amplicon plasmid. The major drawback was that even though the packaging signals had been removed from the cosmids, low levels of helper virus (generated through recombination) were still present in the amplicon stocks.
Most recently, Saeki et al. (47) developed a packaging system capable of producing virtually helper-virus-free amplicon stocks containing less than 1 helper virus per 108 amplicon transducing units (T.U.). In this system, an artificial bacterial chromosome (BAC) containing the entire HSV genome, with the packaging signals and ICP27 coding sequences removed, as well as an additional “stuffer” DNA sequence, was engineered. ICP27 must be supplied in trans either by transfection or by a complementing cell line (Fig. 2). The stuffer DNA sequence increases the size of the BAC to 178 kb. This decreases, though does not eliminate, the likelihood that the BAC will be packaged into a viral particle in the event that it acquires a packaging signal through recombination with the amplicon vector. Additionally, the majority of reconstituted helper viruses generated in this way are likely to be attenuated or replication-defective because they lack ICP27 and have likely lost viral genes through deletions to achieve a size small enough to be packaged. Furthermore, the potential to generate a packaging- and replication-competent helper virus exists; however, this requires that the BAC acquire ICP27 through another recombination event with the ICP27 plasmid, or from the complementing cell line. Because this combination of events is rare, the HSV amplicon stocks produced are essentially helper-free.
Preparation of Herpes Simplex Virus-1 amplicons. The HSV amplicon plasmid contains a shRNA cassette, a viral origin of replication (ori), and a packaging signal (pac). Three helper systems are available for the preparation of HSV amplicons; each provides all of the viral genes necessary for packaging. A. Helper virus: Permissive cells are transfected with the amplicon plasmid and then superinfected with HSV helper virus. B. Cosmids: The amplicon plasmid is co-transfected into permissive cells along with a set of five cosmids covering the entire HSV-1 genome (with the packaging signals deleted). C. BAC: The amplicon plasmid is co-transfected into permissive cells along with a plasmid carrying the ICP27 gene and a Bacterial Artificial Chromosome (BAC) containing the entire HSV-1 genome, minus the packaging signal and ICP27. In all systems, the amplicon plasmid is replicated in permissive cells via a rolling-circle mechanism, and the resulting linear concatameric DNA is cut into 150 kb segments that are then packaged into amplicons. Amplicon stocks produced using the helper virus system (A) contain low levels of contaminating helper virus. Amplicon preparations produced using the cosmid system (B) contain low levels of contaminating recombinant virus. In the last system, the large size of the BAC precludes the generation and packaging of the majority of recombinant HSV, resulting in virtually pure amplicon preparations (C). Figure adapted from Marconi P, Argnani R, Berto E, Epstein AL, Manservigi R. HSV as a vector in vaccine development and gene therapy. Hum Vaccin. 2008;4:91–105, by permission of the author.
Alternatively, improvements continue to be made in the development of helper virus-based helper systems to produce amplicon stocks free of contaminating helper virus. For example, in the work of Zaupa and colleagues (48), a series of two ICP4-completmenting cell lines, the second of which also expresses Cre recombinase, and an ICP4-deficient helper virus with a floxed packaging signal were developed. The amplicon plasmid is transfected into the first cell line and then super-infected with helper virus to produce amplicon vectors containing helper virus. These stocks are then used on the second, Cre-expressing cell line; because this line expresses Cre recombinase, the floxed packaging signal in the helper virus is removed, preventing packaging of the helper genome. The final amplicon vector stocks produced with this procedure have high titer, up to 5 × 108 T.U. per ml after concentration, with one contaminating helper virus per 224 amplicons.
HSV Amplicons for RNAi In Vitro and In Vivo
Because HSV amplicons are only capable of carrying DNA, it is not possible to directly deliver siRNA oligomers. However, there have been several reports of RNAi achieved with helper virus-free HSV amplicons carrying DNA sequences that generate shRNA.
Sabbioni et al. (49) used shRNA-generating amplicon vectors to silence the expression of the large T antigen (T-Ag) in BK polyomavirus-transformed cells, thus neutralizing their tumorigenic properties and transformed phenotype. In addition to two GFP cassettes used to monitor transduction efficiency, the amplicon plasmid contained an oligonucleotide sequence under an H1 RNA polymerase III promoter that when expressed generates an shRNA designed to suppress T-ag (pA-shBKVT). Reduced staining with a fluorescently tagged antibody against T-ag in successfully transduced (i.e., GFP-positive) cells was observed, indicating that T-ag expression was being suppressed by siRNA. This was confirmed by Western blot, as they saw a marked reduction in T-ag levels in pA-shBKVT-transduced cells as compared to those transduced with a scrambled shRNA control (multiplicity of transduction (MOT) = 5 was used). Cell counting assays showed a dose-dependent reduction in the growth rate of pA-shBKVT-transduced cells in vitro, and pA-shBKVT transduced cells (2 × 105 cells per mouse) did not establish tumors even after 31 days in BALB/c mice, unlike empty vector and scrambled controls.
Saydam et al. (50) had previously used a similar system, in which amplicon vectors contained an EGFP expression cassette and a shRNA sequence, to suppress the growth of human glioma cells in vitro and in vivo by targeting epidermal growth factor receptor (EGFR). In vitro, EGFP expression allowed Saydam and colleagues to determine that approximately 30% of cells were transduced by the amplicon vectors. Western blotting showed a marked decrease in EGFR in cells 4 days after transduction with amplicons expressing shRNA against EGFR (pHSVsiEGFR). Saydam et al. also observed a 40–50% decrease in colony forming ability as well as an increase in apoptosis over the control (MOT = 5). In athymic nude mice, glioma cells transduced with amplicons carrying only EGFP and shRNA against EGFP were able to establish tumors, whereas those transduced with pHSVsiEGFR prior to implantation were not. For pre-established xenograft tumors, those treated intratumorally with 1 × 106 T.U. of pHSVsiEGFR three times per week were significantly smaller in volume and expressed less EGFR compared to those that were mock- or EGFP-treated.
Finally, Saydam et al. (51) were able to show in a separate study that glioma cells in vitro and xenograft tumors treated with amplicons carrying shRNA against Rad51, an essential component for homologous recombination in double-stranded DNA break repair, were more sensitive to the effects of ionizing radiation than those treated with control amplicons coding for shRNA against EGFP.
Concerns and Outlook for HSV Amplicons
There are several disadvantages to the HSV amplicon system, including the difficulty in producing high-titer, helper-virus-free amplicon stocks. Although the BAC system can generate essentially helper-free amplicon stocks, the titer is on the order of 107 T.U. per ml (47). This issue may be addressed with additional improvements to the helper-free systems, or potentially with the further development of helper systems, such as the one described above by the Epstein group (48), which achieve high titers albeit with higher levels of contamination. The level of helper virus in their system is relatively low (0.5%), and 36% transduction efficiency was maintained with only a minute increase (0.23%) in cell death.
HSV amplicons carry no viral coding sequences and are therefore not toxic to the transduced cell. However, the possible impact of pre-existing immunity to HSV on the efficacy of HSV amplicons and the potential for recombination in a patient with a latent HSV infection is still somewhat debated (39,52–54). The HSV amplicon is also a transient expression system. Therefore, long-term, stable expression of the transgene sequence is not possible without the creation of an integrative amplicon hybrid, such as the EBV-, retrovirus-, or AAV-amplicon hybrids (55).
HSV amplicons are attractive vectors because of their similarity to HSV-1, while not containing any viral genes. HSV amplicons make use of the natural tropism of wild-type HSV for neural and epithelial cells, but have also been shown to be capable of transducing a number of cell and tissue types (43,56). In addition, work on the engineering and targeting of HSV to specific receptors and cell types can also be directly applied to amplicons (57–59). Perhaps the most attractive feature of HSV amplicons is their extremely large transgene capacity. The native virus’s 150 kb capacity allows for the conveyance of extremely large fragments of foreign DNA, meaning that multiple transgenes and expression cassettes can be included on the same vector, such as EGFP to monitor transduction efficiency, as well as entire regulatory mechanisms (60). Other possibilities include expression cassettes for multiple shRNAs against different sequences of the targeted mRNA, several variants of the targeted mRNA (i.e., spliced forms), or different mRNAs. Because of the concatameric nature of the amplicon, there can be multiple copies of the transgenic sequence, thus increasing the likelihood that these sequences will be expressed at high levels within the cell.
SV40 In Vitro–Packaged Vectors: An Efficient Method to Deliver siRNA and Express DNA-Directed siRNA
Simian Virus 40
Simian virus 40 (SV40) is a non-enveloped polyomavirus with a 5.2 kb double-stranded circular DNA genome. The wild-type SV40 genome encodes two early genes: the large T antigen (T-ag), which is essential for viral genome replication and expression of the late genes, and the small t antigen (t-ag). The expression of T-ag and t-ag are driven by the SV40 early promoter. The late promoter, located on the opposite strand from the early promoter, is responsible for the transcription of the three capsid genes: VP1, VP2 and VP3 (61–65).
SV40 is able to infect both dividing and non-dividing cells and is capable of integrating into the host genome in various locations. Moreover, the circular DNA genome may open at various sites when it integrates (66,67). SV40 infection and integration can occur in all mammalian species; however, replication of the virus is limited to monkeys who are therefore considered “permissive.” Human cells support viral replication in a non-efficient manner, and therefore are categorized as “semi-permissive,” and other species, such as mice, are “non-permissive.” Maintenance of the wild-type virus within the host genome can occur either by integration, as described above, or by the formation of a self-replicating mini-chromosome, a process that requires the expression of T-ag.
Entry of the wild-type virus into cells differs from most other viral infection pathways in that it largely avoids a cytoplasmic phase and differs from enveloped viruses because of its inability to fuse with the cell membrane. Viral entry begins with the virus binding to its primary receptor, the major histocompatibility complex class I (MHC class I) (68). The virus then binds to GM1 gangliosides and travels with them to the endoplasmic reticulum (ER). The transport to the ER is mediated by caveolae and facilitated by ER chaperones. Following disassembly in the ER, nuclear pore complexes assist in delivery of the viral DNA to the nucleus for replication.
Preparation of SV40 In Vitro-Packaged Vectors
SV40 in vitro-packaged vectors represent a third example of a trans-packaging system. These vectors are derived from SV40 and exploit the ability of the viral capsid proteins to self-assemble into virus-like structures around nucleic acids (65,69). While in vitro-packaged vectors have been prepared using all three capsid proteins (70,71), these virus-like particles are routinely assembled using only VP1, greatly simplifying their preparation (72).
The first step in the in vitro preparation of the SV40 particles is the production of VP1. Production of this major capsid protein is accomplished in Sf9 insect cells using a baculovirus expression system. Sf9 nuclear extract containing VP1 is mixed in a tube with the nucleic acid cargo (either plasmid DNA or siRNA) around which VP1 assembles into pseudoviral particles in the presence of ATP and MgCl2. After assembly, the pseudoviral particles are stabilized by the addition of CaCl2. No encapsulation sequences are required, so the process does not incorporate any of the wild-type SV40 genetic material. Mukherjee and colleagues (73) developed a slightly different methodology for encapsulation using the same VP1-containing nuclear extracts from Sf9 cells treated with a reducing agent (dithiolthreitol, DTT) and RNase. During the assembly step, their method calls for KCl, NH4Cl, glycerol, and a pH of 7.9 in addition to ATP and MgCl2. The stabilization step is buffered to a pH of 5.2. Fig. 3 compares these two methods. The lack of viral genetic material means that synthetic siRNA oligomers or large DNA plasmids, up to ~ 17 kb, can be efficiently packaged. These particles can be stored at −20°C or −80°C and used to directly transduce a variety of cells in vitro (dividing as well as resting cells), or injected in vivo. While the inherent immunogenicity of SV40 in vitro-packaged vectors has not been conclusively determined, based on studies of other SV40-derived vectors, it is thought that these pseudovirions are unlikely to elicit immune responses in vivo (74,75).
Methods of SV40 in vitro packaging. Nuclear extracts from Sf9 cells are harvested 3 days after infection with a baculovirus that carries the gene for the major capsid protein of SV40, VP1. In the conventional method of packaging (left-hand side), 100 µg of nuclear extract is mixed with the cargo (e.g., siRNA), ATP, doubly distilled water, and MgCl2 and incubated in a 37°C water bath for 6 h (Assembly). This represents one packaging reaction. To stabilize the pseudovirions, CaCl2 is then added and the packaging reaction is placed on ice for 1 h before being stored at −20°C. In a second method, developed by Mukherjee et al. (73???) (right-hand side), nuclear extracts are treated with a reducing agent (DTT) and RNase for 20 min in a 37°C water bath to fully dissociate partially formed capsids and to remove Sf9 RNA. In the assembly step, a mix containing plasmid DNA, ATP, Hepes-KOH pH 7.9, MgCl2, KCl, NH4Cl, glycerol, NP-40, and doubly distilled water is combined with the treated nuclear extracts in a 1:5 (wt/wt) ratio of DNA to VP1 and incubated at 37°C for 1 h. Next, the stabilization buffer, containing CaCl2, sodium acetate buffer pH 5.2, KCl, NH4Cl, and distilled water, is added to packaging reaction and kept on ice overnight. Lastly, the finished packaging reaction is incubated with DNase I on ice for 10 min to digest unincorporated DNA. The DNA disgestion is stopped by performing a chloroform extraction, and completed particles are collected in the aqueous phase and stored at −80°C.
Comparison to Recombinant SV40 Virus (rSV40)
There are certain fundamental differences between in vitro-packaged vectors and the related, recombinant SV40 viral vectors (rSV40) described in the works of Strayer and Cordelier, among others (76). In 2003, Cordelier and colleagues (77) designed a recombinant SV40 vector that lacked T-ag sequences but retained the SV40 capsid genes, as well as the origin of replication (ori) and packaging signal (ses), which overlap with the SV40 early promoter region. This recombinant virus carried a shRNA sequence shown to target the CCR5 chemokine receptor in phagocytes and was packaged into infectious virions with the help of a COS7 packaging cell line that stably expresses an origin-defective SV40 mutant. They demonstrated a reduction in the number of cell membrane CCR5 receptors, which was shown to protect cells from infection with R5-tropic HIV. These rSV40 vectors differ from in vitro-packaged vectors, which carry no viral sequences and have also been used in RNAi applications (described below), because they still carry viral coding sequences and so cannot be categorized as pseudovirions. rSV40 vectors whose structural genes have been removed, leaving only ori, ses, and the SV40 early-promoter (which is overlapped by ori and ses), are also possible (76).
Delivery and Expression of siRNA Using SV40 In Vitro-Packaged Vectors
In a 2005 report (78), we demonstrated the use of in vitro-packaged SV40 pseudovirions to deliver plasmids expressing shRNAs and synthetic, single-stranded siRNA oligomers. A panel of experiments was performed in two different types of cells (non-adherent .45 human lymphoblastoid cells and adherent HeLa cells) to determine the conditions needed for packaging siRNA, the quantities of siRNA or shRNA plasmid vector needed to silence the reporter gene EGFP, and the requirements for co-transducing an EGFP reporter gene with siRNA or shRNA plasmid vector.
Using confocal microscopy, we demonstrated the delivery of fluorescently-tagged siRNAs (siRNA-3′FL) via SV40 in vitro-packaged pseudovirions into .45 lymphoblastoid cells. Three days post-transduction, the fluorescence signal observed using confocal microscopy as well as flow cytometry indicated that in vitro-packaged vectors successfully delivered siRNA to all cells. Human lymphoblastoid cells were also transduced with pseudovirions carrying a plasmid that expresses EGFP as well as two sets of pseudovirions containing siRNAs to silence EGFP (IVP-siGFP). The cells were monitored daily via flow cytometry. Expression of EGFP was virtually shut down on day 3 and recovered completely by day 6. This is a significant result because transduction of cells in suspension with siRNA is more challenging than with adherent cells.
siRNA was also effectively delivered into HeLa cells that stably express EGFP using SV40 in vitro-packaged vectors; cells analyzed by flow cytometry three days post-transduction with IVP-siGFP showed that a 300-fold reduction in fluorescence was achieved in these cells. Moreover, various amounts of siRNA were used in the packaging reaction— from 1 to 100 μg, equivalent to approximately 140 pmol to 14 nmol— and in all cases EGFP fluorescence was dramatically reduced after 3 days with only very slight dose-response differences, indicating that sub-microgram quantities of in vitro-packaged siGFP may be sufficient to silence gene expression. On day 4, EGFP expression slowly began to increase and completely recovered six days post-transduction.
These findings suggest that SV40 pseudovirions can be used to package and introduce siRNA sequences into both adherent and non-adherent cells, achieving some degree of silencing for up to 6 days in vitro.
Concerns and Outlook for In Vitro-Packaged SV40 Vectors
In conclusion, SV40-based pseudovirions have a promising potential for use in RNAi applications. SV40 in vitro-packaged vectors have a number of important advantages and a few disadvantages. They are able to transduce cells from a variety of mammalian species and to transduce quiescent as well as actively dividing cells. In vitro, cells in suspension are transduced with a similar efficacy and efficiency as adherent cells, a highly desirable and distinguishing characteristic of these vectors. The greatest advantage of the SV40 system is the ease with which the vectors are prepared and the flexibility that the system affords with regard to cargo. As described above, SV40 in vitro-packaged vectors do not require any viral packaging sequences, neither in cis nor in trans, and thus are able to package shRNA-encoding plasmids as well as synthetic siRNA oligomers. In addition, synthetically modified oligomers, such as those that have been fluorescently tagged, can also be packaged, which sets SV40 apart from the two pseudovirion systems discussed above.
In our 2005 work (78), the lower limit of siRNA needed to achieve silencing was undetermined, and so the quantity of siRNA needed may be much less than 1 µg. While there has been some study of cellular uptake (79), the mechanism of vector entry has not been fully elucidated. It is possible that wild-type SV40 virions, which are trafficked to the ER and subsequently disassembled, travel a different pathway than in vitro-packaged vectors carrying siRNA oligomers, whose cargo must ultimately go to the cytoplasm.
Because the VP1 capsid protein is produced in Sf9 cells, large quantities of vector can be easily prepared in vitro; this, however, is also one of the greatest drawbacks to the SV40 system. The mechanism of packaging and pseudovirion self-assembly is not yet fully understood, and components in the crude nuclear extracts of Sf9 cells that may aid in this process are as yet uncharacterized. This lack of characterization presents an additional obstacle to the development of these vectors for therapeutic use in humans.
Application of Influenza Virosomes to the Delivery of siRNA
The Influenza Virus
Influenza is an enveloped RNA virus that infects mammals and birds. The virus bears an 80–120 nanometer envelope coat which encapsulates a core of negative-sense genomic RNA intertwined in nucleoprotein. Owing to its segmented genome and lack of proofreading RNA polymerase, influenza evolves rapidly, allowing it to evade host protective immunity (80). Many serotypes exist, based on antibody response to distinct influenza envelope proteins, which gives rise to the common nomenclature for this virus (e.g., H5N1, H1N1). Of the three genera of influenza, type A boasts the greatest serotypic variety and presents the most serious risk of virulence to humans. Advances in virology have allowed researchers to harness the infectious qualities of this virus in the form of reconstituted influenza virosomes, which represent a promising delivery vehicle of therapeutic agents such as siRNA.
The influenza virus has ensured its continued survival by evolving elegant mechanisms to faithfully deliver its genetic material and efficiently escape host cell defenses. It relies on two viral coat proteins to accomplish this task: hemagglutinin (HA) and neuraminidase (NA). HA is a homotrimeric integral membrane glycoprotein which binds to terminal sialic acids located on surface glycoproteins and glycolipids of target cells. Once tethered to the cell surface, viral particles are endocytosed via clathrin-dependent and clathrin-independent pathways (81). The virus is then sequestered in endosomes and is subjected to acidification during endosome maturation. A drop in pH below 6 initiates a conformational change in HA such that a hydrophobic fusion peptide is able to insert into the endosomal membrane. The fusion of the viral and endosomal membranes liberates the encapsulated genomic RNA which escapes into the cytosol (82,83).
Neuraminidase, the other chief virulence coat protein, cleaves terminal sialic acid from the cell surface. While HA is integral to viral entry, its binding also hinders the budding of a mature virus particle. NA thus ensures a timely release by eliminating binding sites for HA (84). Sialic acids located on neighboring viral envelopes are also cleaved by NA, which prevents viral aggregation.
Virosomes and Their Uses
The HA coat protein is sufficient to mediate both cell surface binding and membrane fusion (85). HA, along with the other viral envelope constituents, can be isolated and reconstituted into virus-like particles dubbed virosomes (86). Virosomes mimic native influenza in terms of morphology, receptor binding characteristics, and membrane fusion capability. They have proven their utility in the delivery of a variety of therapeutics that can be linked to the virosomal surface or encapsulated within the lumen.
Aside from their power to encapsulate and deliver siRNA, virosomes have proven useful in a number of other applications. Since the first documented production of virosomes in 1975, the span of virosome-mediated applications has broadened markedly. Initial investigations into reconstituted virosomes indicated that they are strong stimulants of the immune system (86). Accordingly, virosomal vaccine strategies have been at the forefront of much research regarding reconstituted influenza virosomes. Unlike inactivated native influenza, virosomes retain their endosomal fusogenic properties. They can present antigens to the cytosol, enabling them to access MHC class I antigen presentation and thus provoke CD8+ T lymphocyte activity. Virosomes, therefore, stimulate the cellular arm of the immune system by spurring cytotoxic T lymphocyte activity, in addition to eliciting a potent humoral response. The existence of virosome-based influenza and non-influenza vaccines (87,88) and reported anti-cancer immune stimulating properties (89) demonstrate the versatility and immunostimulatory characteristics inherent to virosomes. In addition to their immunological applications, cytotoxic drugs and other toxins have been incorporated and delivered using virosomes (90,91).
For over a decade, virosomes have been recognized for their ability to deliver plasmid DNA (pDNA) attached to their surface (92). Conventionally, a cationic lipid is incorporated into the virosomal membrane, which allows pDNA to associate externally. However, DNA complexed to the virosome surface is sensitive to nucleases and is degraded in vivo (93). This susceptibility spurred the development of a new method for preparing virosomes that offers protection to the nucleic acid cargo. The virosome assembly method discussed below accomplishes this task.
Virosome Preparation
The production of virosomes primed for the delivery of encapsulated siRNA is detailed by de Jonge et al. (94) and in Fig. 4. Native type A influenza virus, H3N2 in this instance, is first subjected to β-propiolactone, a common anti-viral agent that inactivates the viral RNA. The viral envelope is then solubilized by the addition of 1,2-dihexanoyl-sn-glycero-3-phosphatidylcholine (DCPC), a short-chain phosphatidylcholine with detergent-like properties. Subsequent ultracentrifugation of the solubilized virus serves to both isolate the major envelope proteins, namely HA and NA, in a clear supernatant and remove pelleted nucleoprotein containing the influenza genomic RNA that remains intact, thus removing any replicative ability.
Preparation of siRNA-loaded influenza virosomes. Native influenza virus is first inactivated by the addition of β-propiolactone. The virus is sedimented from the preparation and solubilized upon the addition of DCPC, a short-chain phosphatidylcholine with detergent-like properties. Ultracentrifugation pellets the viral capsids and nucleoprotein. Solubilized viral coat components remain in the supernatant and are combined with siRNA that has been previously complexed with the cationic lipid DODAC. DCPC is removed through dialysis allowing for viral membrane reconstitution and siRNA encapsulation. Lastly, reconstituted virosomes are purified through discontinuous sucrose gradient ultracentrifugation. (Influenza virus image adapted from the “Molecular Expressions” website of the National High Magnetic Field Laboratory, Florida State University, by permission.)
Because the encapsulation of naked siRNA is inefficient (95), duplex siRNA is first complexed to the cationic lipid N,N-dioleoyl-N,N-dimethylammonium chloride (DODAC); this increases the incorporation efficiency of siRNA to 35%. The addition of complexed siRNA to the solubilized viral lipids and membrane proteins is followed by the removal of the DCPC detergent by dialysis. Extraction of DCPC permits the virosomes to reconstitute and, in the process, encapsulate siRNA. Finally, any free, unencapsulated material is removed from the preparation by discontinuous sucrose gradient ultracentrifugation. The resulting virosome particles have a mean diameter of 60 nm and are prepared to deliver their packaged siRNA.
Analysis of reconstituted virosomes by continuous sucrose gradient centrifugation reveals that virosome protein, phospholipids and siRNA are enriched at a single sucrose density. Virosomes are also capable of protecting encapsulated siRNA from extravirosomal proteins, as exposure to benzonase, a potent endonuclease, fails to substantially degrade packaged siRNA (<20%). Thus, siRNA is tightly packaged within mature virosomes (94).
In Vitro and In Vivo Delivery of siRNA Via Virosomes
Jonge et al. (94) conclusively established the in vitro delivery of duplex siRNA packaged within virosomes and provided preliminary insight into the in vivo utility of this delivery system. Using Cy5-labelled siRNA, the fusogenic capability of packaged virosomes was first verified: virosomes exhibited rapid fusion with erythrocyte ghost target membranes at pH 5.5 but not when incubated at a pH of 7.7. Therefore, reconstituted virosomes retain the pH-dependent conformational switch mechanism intrinsic to native influenza HA. Importantly, virosomes do not exhibit the significant levels of cellular toxicity detected in baby hamster kidney (BHK21) cells, unlike native influenza.
A direct assessment of delivery capacity alongside Lipofectamine™ 2000 resulted in similar levels of siRNA delivery, with virosomes having slightly higher efficiency at low siRNA concentrations. A functional in vitro analysis showed that siRNA packaged into virosomes was able to inhibit the expression of both transiently and constitutively expressed EGFP in a dose-dependent manner: BHK21 cells analyzed by confocal microscopy 24 h after treatment with virosomes containing siRNA showed little change with 1 and 2.5 pmol of siRNA, but significant fluorescence reduction with 5 and 10 pmol. The effects were specific, as control cells treated with virosomes containing siRNA directed against HA exhibited no reduction in fluorescence. In addition, the effect was shown to rely on the fusogenic capability of the packaged virosomes, as virosomes whose HA had been inactivated with low pH treatment were ineffective.
In A2780 cells constitutively expressing GFP, a dose-dependent silencing effect was seen using flow cytometry at 24 h after treatment, with a maximum reduction (77%) in expression observed at 72 h. Importantly, transfection efficiency seemed to approach 100% as the entire cell population was shifted to lower fluorescence. Transfection efficiency with Lipofectamine™ 2000 was slightly more effective but also more toxic to cells, limiting the maximum deliverable amount of siRNA to 3 pmol. By contrast, siRNA-loaded virosomes were well-tolerated.
Lastly, C57BL/6 mice injected intraperitoneally with 200 pmol of fluorescently labeled siRNA encapsulated within virosomes showed significant levels of siRNA within cells of different sizes, probably representing granulocytes, macrophages and lymphocytes. While not comprehensive, these results indicate virosomes may represent an efficacious vehicle for the in vivo delivery of siRNA into various cell types.
Modifying Influenza Virosomes: Targeting Through Hydrophilic Polymers
In an effort to improve stability and target specific cell types, innovative modifications to virosome composition have been proposed. While they are just beginning to be explored, these types of alterations have been extensively investigated in liposomal applications, and could ultimately prove beneficial in advancing virosomal delivery techniques.
The addition of hydrophilic polymers such polyethylene glycol (PEG), polyacryloylmorpholine, polyvinylpyrrolidone, or poly(2-oxazoline) can stabilize liposomal vesicles (96,97) and increase circulation time in vivo (98). However, finding evidence that these polymers confer heightened stability once incorporated into the virosome membrane has proved difficult. In fact, initial examination of PEG-modified virosomes showed substantial inhibition of fusogenic capacity and sialic acid receptor binding (99). Also, PEG-incorporated liposomes typically have PEG moieties on both sides of the bilayer membrane. When located on the inner face of a liposome, its large molecular weight renders a PEG molecule a steric inhibitor of nucleic acid encapsulation (100). An alternative preparative methodology has been established that results in PEG moieties being preferentially inserted into the outer membrane of liposomes, which results in little loss of encapsulated material (101).
While hydrophilic polymers have presented obstacles in conferring virosomal stability, their role in targeting virosomes to specific cell types has yielded promising results. Due to the ubiquitous nature of the cell surface receptors targeted by HA, directing virosomes to a specific cell type is challenging because they must be redirected and targeted concurrently. By coupling Fab’ fragments of an anti-epithelial glycoprotein antibody to the distal end of PEG, reconstituted virosomes have been shown to selectively target ovarian carcinoma cells (102). In this instance, the conjoined antibody ensures target cell specificity. The PEG layer simultaneously prevents HA from binding to cell surface sialic acids, while also preserving the function of the HA fusion peptide within acidified endosomes. Similarly, conjugating Fab’ fragments of an anti-Neu (an oncogenic transmembrane growth factor receptor) antibody to PEG-coated virosomes resulted in selective cell infection (90). Doxorubicin was selectively delivered to Neu-over-expressing breast tumor cells using these targeted virosomes. When tested in vivo, administration of doxorubicin-loaded virosomes arrested tumor formation. While these two antibody-conjugated PEG virosomes were originally developed as vehicles for cytotoxic drugs, their application to virosomal siRNA delivery should be straightforward.
Concerns and Outlook for Influenza Virosomes
Their ease of production and modification makes virosomes an attractive choice for the delivery of siRNA. Additionally, all components of the virosome have been approved for use in humans. Like other pseudovirions, virosomes are stripped of their functioning genetic material and therefore do not raise the concerns that surround conventional viral use.
Virosomes are often compared to liposomal cationic lipids, a closely related delivery vehicle that is extensively used in the in vitro delivery of siRNA (103–106). Both virosomes and cationic lipids are able to deliver large lipid:DNA complexes into cells. Because cationic lipid complexation and liposome encapsulation have proven to be effective at nuclease protection and endocytosis initiation, their employment in the in vivo delivery of siRNA has been widely explored. But the mechanisms by which internalized siRNA escapes endosomes packaged within liposomes are not fully understood, and lipid compositions must be carefully selected in order to ensure efficient membrane disruption and cytosolic liberation.
Drawbacks to influenza virosome-mediated siRNA delivery arise primarily from the strong immune response elicited upon virosome administration. This delivery system’s stark immunogenicity is problematic, especially when considering that many individuals bear pre-existing HA- or NA-specific antibodies stemming from prior influenza exposure, including vaccination. Some studies have shown that uptake of influenza virus by cells expressing high levels of Fc receptors is enhanced by non-neutralizing, anti-HA and anti-NA antibodies (107,108). While opsonization of virosomes does result in antibody-dependent enhancement of infection, it proves beneficial only when using virosomes as a delivery vehicle for immunizing proteins and peptides destined for antigen-presenting cells (109). This phenomenon offers little, if any, benefit to siRNA delivery, since the vast majority of mammalian cells do not have significant levels of Fc receptors on their surface (110). Neutralizing antibodies can severely impede the cellular uptake of virosomes, which is likely to render readministration of virosome-encapsulated siRNA problematic. Thus, the delivery of siRNA encapsulated in virosomes is inherently immunogenic. Immuno-privileged sites within the body may tolerate the introduction of virosomes well, but the direct injection of virosomes into organs and tissues such as the brain, eyes and testicles presents technical challenges.
Measures to circumvent obstacles presented by the immune system have been proposed. If prior exposure to a particular serotype of influenza is known, virosomes can be manufactured using novel influenza serotypes to avoid a strong, immediate immune response. The use of pH sensitive bonds between PEG and virosome lipids has been conjectured to circumvent immunological detection while dependably preserving the fusogenic capability of the virosome (102). This strategy, although unproven, may prove to be practical and effective at surmounting the challenges presented by virosome immunogenicity.
Finally, influenza virosomes are relatively unproven in their ability to deliver siRNA both in vitro and in vivo. To date, only one report has shown their competency to deliver siRNA (94). Even so, virosomes have proven their worth in a number of other in vivo applications, including immunization and drug delivery. This newly engineered delivery system will likely receive added attention in forthcoming siRNA applications, but much work lies ahead.
Hemagglutinating Virus of Japan Envelope Vector
Hemagglutinating Virus of Japan (HVJ)
Hemagglutinating Virus of Japan (HVJ), also known as Sendai virus, is a murine parainfluenza virus of the Paramyoxviridae family that was first identified in Japan in the early 1950s (111). HVJ is a negative-strand RNA virus. The nucleocapsid core of the virus, which contains the RNA genome, is surrounded by a lipid-bilayer viral envelope, and its overall size is 150-600 nm (112). The surface of the viral envelope contains two characteristic and integral glycoproteins, both of which are essential for infectivity. The first glycoprotein, HN, has both hemagglutinating and neuraminidase activities. HN binds to, and ultimately degrades, acetylated sialic acid receptors on the surface of cells.
After HN has bound HVJ to the cell surface, the fusion protein, F, is able to interact with lipids in the cell’s plasma membrane, such as cholesterol. The F glycoprotein induces the fusion of the viral envelope with the cell membrane, at which point the contents of the viral envelope are delivered directly into the cytoplasm. This process can occur at neutral pH, an important contrast to influenza. The influenza virus enters the cell via endocytosis, and the viral contents escape only after acidification of the endosome, by which point the contents could be degraded. By contrast, HVJ, and other viruses, such as herpes virus and human immunodeficiency virus (HIV), fuse directly with the cell membrane (112).
Development of the HVJ-Envelope Vector: Derivative of the Hemagglutinating Virus of Japan
Although the viral fusion properties of HVJ make it attractive as a vector, the viral proteins produced in infected cells are cytotoxic and highly immunogenic (113). Thus, a pseudoviral vector was developed that makes use of the desirable qualities of HVJ while circumventing those that are problematic. It should be noted that several groups have used virosomes that incorporate the reconstituted envelope proteins of HVJ (114–116). However, they are not discussed further here because of their similarity to influenza virosomes.
A chimeric HVJ-liposome system was first reported by Kaneda et al. in 1989 and subsequently developed (117,118). In this system, loaded DNA liposomes were fused with UV-inactivated HVJ to form fusogenic liposome hybrids that had higher levels of trapped DNA than reconstituted virosomes, and whose major advantage was their ability to transmit their cargo directly to the cytoplasm, bypassing endocytotic uptake (119,120). The HVJ-liposome system, however, suffered from a complicated procedure used to generate and fuse liposomes with inactivated HVJ, and reduced fusogenic ability (approximately 2% relative to native HVJ) due to dilution of HVJ glycoproteins (121). To address these issues, a new vehicle, termed the HVJ-Envelope (HVJ-E) vector, was developed (121) in which cargo, such as DNA, is incorporated directly into intact, though inactivated, HVJ (reviewed by Kaneda et al. (113,122)).
To generate HVJ-E vectors, wild-type HVJ (VR-105 parainfluenza1 Sendai/52, Z strain) (113) is first inactivated by treatment with either β-propiolactone (0.0075–0.001%) or by UV irradiation (99–198 mJoule/cm2), and then purified by ion-exchange chromatography and gel-filtration. The resulting inactivated HVJ particles have a mean diameter of 220 nm, and maintain the native ratio of F and HN fusion proteins, ~ 2–2.3:1, which is extremely important for the efficient fusion of the viral envelope with the cell membrane (112,123). Because this ratio is preserved, the fusogenic ability of the inactivated HVJ is similar to that of native HVJ. Inactivated HVJ is then treated with a mild detergent (e.g., 0.24–2% Triton X-100) in the presence of the intended cargo (e.g., plasmid DNA, siRNA, ODNs, peptides, drugs, or combinations thereof) and centrifuged at 18,500 × g for 15 min to move the cargo into the inactivated HVJ, resulting in HVJ-E vectors (Fig. 5). Fragments of the inactivated HVJ genome and nucleocapsid are present inside of the HVJ-E vector. The supernatant containing unincorporated cargo is removed, and the pelleted HVJ-E is resuspended in PBS. The incorporation efficiency for plasmid DNA is approximately 15–20%; incorporation efficiency drops to 3% without centrifugation, and no DNA is incorporated without detergent treatment. The efficiency of DNA incorporation was measured by treating the completed vectors with DNase I and then solubilizing the vectors and measuring the amount of DNA that was protected within the envelope (121). The incorporation efficiency for siRNA is reported to be similar to that for plasmid DNA. However, determining incorporation efficiency in this manner may not account for nucleic acids adsorbed to the surface of the vector or anchored in the bilayer.
Preparation of hemagglutinating virus of Japan envelope (HVJ-E) vectors for the delivery of siRNA. Native HVJ virus is inactivated with UV irradiation and then purified using ion-exchange and gel-filtration chromatographies. Fragments of the inactivated viral genome and nucleocapsid are retained within the inactivated HVJ particle. Inactivated HVJ particles are then treated with a mild detergent and combined with siRNA and centrifuged at 18,500 × g for 15 min. The siRNA is incorporated into the HVJ particles, resulting in HVJ-E. After centrifugation, the supernatant containing unincorporated siRNA is removed and the pelleted HVJ-E vectors are resuspended in PBS.
The most significant difference between HVJ-E and other non-viral envelope-based vectors is that the native structure of the HVJ is never lost. That is, HVJ is never completely disassembled by solubilization with detergent. HVJ-E has been widely used to deliver a number of different molecules to a variety of adherent and non-adherent cells in vitro (121), and to a number of different target organs and tissues in vivo (113,124,125). The vector kit (GenomONE, Ishihara Sangyo Kaisha, Ltd.) has been commercially available since 2002.
There has also been some work done to target HVJ-E to specific tissues. The first approach was to conjugate HVJ-E with cationized gelatin (CG), a biocompatible polymer. CG-conjugated HVJ-E were shown to deliver a luciferase vector primarily to tumor deposits in a mouse model (126,127). A second approach was to create an HVJ virus that expressed a chimeric form of the F protein in which the extracellular portion of the F protein was replaced with a single chain antibody fragment against mouse desmoglein 3, a cadherin in the basal keratinocytes in skin (128). These chimeric HVJ viruses were used to generate HVJ-E that more efficiently transferred a collagen-VII expression plasmid into basal keratinocytes in mouse skin relative to wild-type HVJ.
In Vitro and In Vivo Delivery of siRNA via HVJ-E
While there are numerous examples of HVJ-E-mediated delivery of siRNA, two examples are presented here. In 2005, Ito et al. (129) used HVJ-E to deliver single-stranded siRNA against Rad51 (important for homologous recombination in dsDNA break repair) and saw an increase in sensitivity to cisplatin in vitro and in vivo. Northern blots of HeLa cells transfected with empty HVJ-E, scrambled siRNA HVJ-E, or siRad51 HVJ-E (siRad51 HVJ-E) showed 0%, 10%, and 90% reduction in Rad51 mRNA levels, respectively. Rad51 protein expression was undetectable for 4 days after transfection with siRNA against Rad51 (~80 pmol siRNA per 1 × 105 cells) compared to the HVJ-E scrambled siRNA control. Additionally, Ito and co-workers showed that siRad51 HVJ-E treatment with cisplatin greatly reduces the colony-forming ability of HeLa cells. The number of colonies formed after 7 days by HeLa cells treated with siRad51 HVJ-E and then treated 3 h later with 0.02 µg/ml cisplatin was only 10% of that formed by cells treated with the HVJ-E scrambled siRNA control and the same amount of cisplatin. The increased sensitivity to cisplatin was true not only of HeLa cells but also of five other commonly used cancer cell lines: PNAC-1 and AsPC-1 (pancreatic), A549 (lung), DU145 (prostate), and MCF-7 (mammary). Cells were treated with HVJ-E siRNA and then treated with 0.1 µg/ml cisplatin 3 days later. Cell counts on day 5 were reduced by at least 30% for all cell lines tested relative to the scrambled control.
For their in vivo studies (129), intradermal HeLa xenografts were established by Ito and colleagues in SCID mice and treated intratumorally with either siRad51 HVJ-E (~2.5 nmol of siRNA) or scrambled siRNA HVJ-E every two days for a total of three injections. Cisplatin (200 µg) was injected intraperitoneally on the day of the second siRNA injection. Tumor volumes were measured every two days, and at the end of the 20-day experiment, the average volumes of tumors treated with siRad51 HVJ-E and cisplatin were approximately 400 mm3, compared to 1000 mm3 for the scrambled siRNA HVJ-E with cisplatin, 1300 mm3 for cisplatin alone, and 2100 mm3 for PBS alone, PBS with scrambled siRNA, and siRad51 HVJ-E. Transfection efficiency of HVJ-E into tumor tissue was estimated at ~ 50% using HVJ-E carrying FITC-ODN.
It is difficult to make many qualitative comparisons between the work of Ito et al. and Saydam et al. (described above (51)), both of which targeted Rad51, due to inherent differences between the systems (HVJ-E and HSV amplicons, respectively). For example, Saydam et al. used ionizing radiation to induce DNA damage, whereas Ito et al. used chemotherapeutic cisplatin. Comparisons are also difficult because the assays and experiments in each study were highly dissimilar; there are, however, a few points worth highlighting. Both studies were targeting the same sequence on the Rad51 mRNA, and both were able to reduce the growth of tumor xenografts when used in combination with drug or radiation therapy. In vitro, the HVJ-E system eliminated Rad51 protein expression 4 days after transfection, whereas with HSV amplicons, expression was reduced by 60–70%. Saydam et al. note that their reduction in Rad51 was achieved using 2000-fold fewer T.U. than in the HVJ-E work by Ito et al. (5 vs. 104 T.U. per cell). However, this comparison is imperfect; in the HSV amplicon system, DNA encoding shRNA was delivered, whereas in the HVJ-E system, siRNA oligomers were delivered directly. Viewed in a different way, Ito et al. used 4.8 × 108 ssRNA oligomers per cell, whereas Saydam et al. used 110 copies of the shRNA cassette per cell.
Another example of HVJ-E-mediated siRNA delivery comes from the work of Watanabe and colleagues (130). In their in vitro studies, they targeted Phsopholamban (PLB), a negative regulator protein of sarcoplasmic reticulum Ca2+ ATPase 2 (SERCA2), responsible for Ca2+ uptake into the sarcoplasmic reticulum. Improper Ca2+ uptake and compartmentalization is a known feature of cardiac failure, and knockdown of PLB has been shown to restore cardiac performance (131). Using duplex siRNA targeted against PLB (siPLB) delivered via HVJ-E (with a scrambled siRNA duplex as a control, 30 nM siRNA), Watanabe and co-workers were able to show successful, dose-dependent knockdown of PLB and a corresponding increase in Ca2+ uptake in rat cardiac myocytes. Transfection of scrambled siRNA showed no effect on PLB mRNA levels compared to HVJ-E alone, whereas PLB mRNA levels were reduced to 24% of the scrambled control 48 h after treatment in cells treated with siPLB HVJ-E. Likewise, PLB protein levels in siPLB HVJ-E-treated cells, measured by Western blot 48 h after treatment, were 12% of those in scrambled siRNA HVJ-E. In a time-course experiment, mRNA levels in siPLB HVJ-E-treated cells were seen to decrease after 1 h, reaching a minimum after 12 h, and recovering only after 4 days. PLB protein levels reached a minimum after 48 h and recovered after 7 days. Levels of PLB in the scrambled control were not significantly changed. Neither were levels of SERCA2 or calsequestrin. Encouragingly, empty HVJ-E vectors did not exhibit cellular toxic effects: subcellular localization of PLB was unchanged, as were mRNA levels for PLB, SERCA2, and calsequestrin. Transfection efficiency, measured using FITC-conjugated siRNA against luciferase that was co-delivered with either scrambled or siPLB, was lower using HVJ-E compared to cationic liposomes. However, the inhibitory effect on PLB expression was higher, presumably because of the protection afforded by HVJ-E against endosomal and lysosomal degradation.
Concerns and Outlook for HVJ-E Vectors
HVJ-E vectors have many strengths. Chief among them is their ability to deliver their cargo directly to the cytoplasm, bypassing endosomal uptake and potential degradation. This is a result of their fusogenic viral origin, and one of the key features that distinguishes them from influenza virosomes. This direct delivery of siRNA to the cytoplasm is also advantageous because it potentially circumvents recognition by TLR7 and 8 in the endosome, similar to electroporation (132). Like virosomes, various cargos, such as peptides, plasmid DNA, siRNA, and small molecule drugs, can, particularly since the development of the vector kit for research use, be delivered using HVJ-E in vitro and in vivo to a number of cell and tissue types. With regard to the delivery of siRNA, the two examples discussed here demonstrate that the effects of siRNA delivered via HVJ-E vectors can be seen in some systems for multiple days in vivo and in vitro.
One potential concern that remains is that of immunogenicity. Although the viral genomic material is completely destroyed during the inactivation process, HVJ-derived vectors are still known to be slightly immunogenic (113). Indeed, one of the applications of HVJ-E makes use of this fact. It was observed that empty HVJ-E vectors have anti-tumorigenic effects through at least two different mechanisms. First, HVJ-E has been shown to activate adaptive immunity and elicit an anti-tumor response via dendritic cell maturation and IL-6 secretion, which in turn mitigates the immune-suppression response of regulatory T cells. In a study by Kurooka and colleagues (133), HVJ-E alone was used as an anti-cancer treatment. In tumor xenograft mouse studies, tumors were established on the left and right flanks of BALB/C mice. Intratumoral injections of HVJ-E to one side eradicated tumors in the opposite flank. This effect was shown to be due to an induced anti-tumor response because similar phenomena were not observed in SCID mice. Second, HVJ-E was shown to activate innate (i.e., non-T cell) immunity. A study by Fujihara et al. (134) showed that HVJ-E caused the secretion of CXCL10 (a chemokine) by dendritic cells in the tumor tissue, recruiting natural killer (NK) cells, as well as activating NK cells systemically.
While anti-tumor effects due to immune system stimulation may be desirable in the treatment of cancer, these phenomena may adversely affect outcomes in other applications of HVJ-E, including siRNA delivery.
CONCLUSION AND FUTURE OUTLOOK
The number of reports of pseudoviral-mediated siRNA delivery remains relatively small, due primarily to the fact that the majority of pseudovirion systems to date have been used for exogenous gene transfer applications. However, as the systems and studies discussed here demonstrate, pseudoviral systems have been used to successfully deliver a number of different siRNA effector molecules, including single-stranded and duplex siRNA and/or siRNA-encoding DNA. They have achieved gene-specific knockdown in a variety of cell types in vitro and in vivo (see Table I). For the majority of systems, direct evidence of the ability to deliver siRNA or a shRNA-encoding vector was shown. More importantly, specific and efficient silencing was achieved over the course of several days in many different model systems.
The basic requirement for any delivery vector is that it delivers its cargo and that the cargo, once delivered, can exert its intended effect. Ideally, a delivery vehicle should also be efficient, targeted, easy to prepare and modify, and non-immunogenic. The unique combination of characteristics possessed by pseudoviral systems makes them extremely attractive as delivery vehicles. For example, pseudovirions are very flexible. Envelope-type vectors are able to deliver multiple cargos, such as combinations of siRNA and small molecule drugs. Also, SV40 in vitro-packaged vectors can encapsulate any number of expression plasmids without modification, greatly simplifying the generation of vectors for new target genes.
There are inherent problems associated with any given pseudoviral vector. For example, systems such as HSV amplicons and phagemid particles are only able to deliver DNA, which is inherently more risky than siRNA oligomers, due to the possibility of integration into the host genome and insertional mutagenesis. One of the most important concerns when using pseudovirions is immunogenicity. For several of the pseudoviral systems presented here, such as the influenza virosome, HVJ-E, and SV40 in vitro-packaged pseudovirions, the extent to which the vectors are inherently immunogenic is still in question, and ways to mitigate cellular and host immune responses are under investigation. Additionally, systems in which the RNAi is derived from DNA (i.e., phagemid particles and HSV amplicons) are unable to package siRNA effector molecules that have been chemically modified to reduce susceptibility to degradation by nucleases and avoid eliciting an innate immune response.
The other most pressing technical problem is that of cell- or tissue-specific targeting, an issue which is not unique to pseudoviral vectors. Fortunately, techniques for addressing this, such as the development of high-affinity ligands through the phage-display system in the case of phagemid particles or functionalized biopolymers in the case of virosomes, already exist. Furthermore, ongoing work to create targeted versions of the parent viral systems is likely to be directly applicable to the virally-derived systems (i.e., pseudovirions), such as the work to create chimeric F-peptides in the HVJ system.
In conclusion, pseudoviral vectors may prove useful in broadening the current scope of siRNA therapeutic strategies and in vitro delivery techniques.
DISCLAIMER
The findings and conclusions in this article have not been formally disseminated by the Food and Drug Administration and should not be construed to represent any Agency determination or policy.
References
Fire A, Xu SQ, Montgomery MK, Kostas SA, Driver SE, Mello CC. Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature. 1998;391:806–11.
Rana TM. Illuminating the silence: understanding the structure and function of small RNAs. Nat Rev Mol Cell Biol. 2007;8:23–36.
Sontheimer EJ. Assembly and function of RNA silencing complexes. Nat Rev Mol Cell Biol. 2005;6:127–38.
Aigner A. Cellular delivery in vivo of siRNA-based therapeutics. Curr Pharm Des. 2008;14:3603–19.
Aigner A. Gene silencing through RNA interference (RNAi) in vivo: strategies based on the direct application of siRNAs. J Biotechnol. 2006;124:12–25.
Aigner A. Delivery systems for the direct application of siRNAs to induce RNA interference (RNAi) in vivo. J Biomed Biotechnol. 2006;4:71659.
Martin SE, Caplen NJ. Applications of RNA interference in mammalian systems. Annu Rev Genomics Hum Genet. 2007;8:81–108.
Nguyen T, Menocal EM, Harborth J, Fruehauf JH. RNAi therapeutics: an update on delivery. Curr Opin Mol Ther. 2008;10:158–67.
Sandy P, Ventura A, Jacks T. Mammalian RNAi: a practical guide. Biotechniques. 2005;39:215–24.
Sanguino A, Lopez-Berestein G, Sood AK. Strategies for in vivo siRNA delivery in cancer. Mini-Rev Med Chem. 2008;8:248–55.
de Fougerolles A. Delivery vehicles for small interfering RNA in vivo. Hum Gene Ther. 2008;19:125–32.
Amarzguioui M, Rossi JJ, Kim D. Approaches for chemically synthesized siRNA and vector-mediated RNAi. FEBS Lett. 2005;579:5974–81.
Judge A, Maclachlan I. Overcoming the innate immune response to small interfering RNA. Hum Gene Ther. 2008;19:111–24.
Behlke MA. Progress towards in vivo use of siRNAs. Mol Ther. 2006;13:644–70.
Siolas D, Lerner C, Burchard J, Ge W, Linsley PS, Paddison PJ, et al. Synthetic shRNAs as potent RNAi triggers. Nat Biotechnol. 2005;23:227–31.
Dotto GP, Enea V, Zinder ND. Functional analysis of bacteriophage f1 intergenic region. Virology. 1981;114:463–73.
Dente L, Cortese R. pEMBL: a new family of single-stranded plasmids for sequencing DNA. Methods Enzymol. 1987;155:111–9.
Mead DA, Kemper B. Chimeric single-stranded DNA phage-plasmid cloning vectors. Biotechnology. 1988;10:85–102.
Kehoe JW, Kay BK. Filamentous phage display in the new millennium. Chem Rev. 2005;105:4056–72.
Marvin DA. Filamentous phage structure, infection and assembly. Curr Opin Struct Biol. 1998;8:150–8.
Monaci P, Urbanelli L, Fontana L. Phage as gene delivery vectors. Curr Opin Mol Ther. 2001;3:159–69.
Li ZH, Jiang H, Zhang J, Gu JR. Cell-targeted phagemid particles preparation using Escherichia coli bearing ligand-pIII encoding helper phage genome. Biotechniques. 2006;41:706–7.
Chasteen L, Ayriss J, Pavlik P, Bradbury ARM. Eliminating helper phage from phage display. Nucleic Acids Res. 2006;34:11.
Jiang H, Cai XM, Shi BZ, Zhang J, Li ZH, Gu JR. Development of efficient RNA interference system using EGF-displaying phagemid particles. Acta Pharmacol Sin. 2008;29:437–42.
Cai XM, Xie HL, Liu MZ, Zha XL. Inhibition of cell growth and invasion by epidermal growth factor-targeted phagemid particles carrying siRNA against focal adhesion kinase in the presence of hydroxycamptothecin. BMC Biotechnol. 2008;8:7.
van Nimwegen MJ, van de Water B. Focal adhesion kinase: A potential target in cancer therapy. Biochem Pharmacol. 2007;73:597–609.
Burg MA, Jensen-Pergakes K, Gonzalez AM, Ravey P, Baird A, Larocca D. Enhanced phagemid particle gene transfer in camptothecin-treated carcinoma cells. Cancer Res. 2002;62:977–81.
Liang Y, Shi BZ, Zhang J, Jiang H, Xu YH, Li ZH, et al. Better gene expression by (-)gene than by (+)gene in phage gene delivery systems. Biotechnol Prog. 2006;22:626–30.
Merril CR, Biswas B, Carlton R, Jensen NC, Creed GJ, Zullo S, et al. Long-circulating bacteriophage as antibacterial agents. Proc Natl Acad Sci USA. 1996;93:3188–92.
Molenaar TJM, Michon I, de Haas SAM, van Berkel TJC, Kuiper J, Biessen EAL. Uptake and processing of modified bacteriophage M13 in mice: Implications for phage display. Virology. 2002;293:182–91.
Vitiello CL, Merril CR, Adhya S. An amino acid substitution in a capsid protein enhances phage survival in mouse circulatory system more than a 1000-fold. Virus Res. 2005;114:101–3.
Yip YL, Hawkins NJ, Smith G, Ward RL. Biodistribution of filamentous phage-Fab in nude mice. J Immunol Methods. 1999;225:171–8.
Zou J, Dickerson MT, Owen NK, Landon LA, Deutscher SL. Biodistribution of filamentous phage peptide libraries in mice. Mol Biol Rep. 2004;31:121–9.
Kassner PD, Burg MA, Baird A, Larocca D. Genetic selection of phage engineered for receptor-mediated gene transfer to mammalian cells. Biochem Biophys Res Commun. 1999;264:921–8.
Larocca D, Baird A. Receptor-mediated gene transfer by phage-display vectors: applications in functional genomics and gene therapy. Drug Discov Today. 2001;6:793–801.
Larocca D, Burg MA, Jensen-Pergakes K, Ravey EP, Gonzalez AM, Baird A. Evolving phage vectors for cell targeted gene delivery. Curr Pharm Biotechnol. 2002;3:45–57.
Legendre D, Fastrez J. Construction and exploitation in model experiments of functional selection of a landscape library expressed from a phagemid. Gene. 2002;290:203–15.
Uppala A, Koivunen E. Targeting of phage display vectors to mammalian cells. Comb Chem High Throughput Screen. 2000;3:373–92.
Lachmann RH. Herpes simplex virus-based vectors. Int J Exp Pathol. 2004;85:177–90.
Smith JS, Robinson NJ. Age-specific prevalence of infection with herpes simplex virus types 2 and 1: a global review, Univ Chicago Press, 2002; S3–S28.
Spaete RR, Frenkel N. The herpes simplex virus amplicon: a new eukaryotic defective-virus cloning-amplifying vector. Cell. 1982;30:295–304.
Marconi P, Argnani R, Berto E, Epstein AL, Manservigi R. HSV as a vector in vaccine development and gene therapy. Hum Vaccin. 2008;4:91–105.
Cuchet D, Potel C, Thomas J, Epstein AL. HSV-1 amplicon vectors: a promising and versatile tool for gene delivery. Expert Opin Biol Ther. 2007;7:975–95.
Geller AI, Breakefield XO. A defective HSV-1 vector expresses Escherichia coli beta-galactosidase in cultured peripheral neurons. Science. 1988;241:1667–9.
Cunningham C, Davison AJ. A cosmid-based system for constructing mutants of herpes simplex virus type-1. Virology. 1993;197:116–24.
Fraefel C, Song S, Lim F, Lang P, Yu L, Wang YM, et al. Helper virus-free transfer of herpes simplex virus type 1 plasmid vectors into neural cells. J Virol. 1996;70:7190–7.
Saeki Y, Fraefel C, Ichikawa T, Breakefield XO, Chiocca EA. Improved helper virus-free packaging system for HSV amplicon vectors using an ICP27-deleted, oversized HSV-1 DNA in a bacterial artificial chromosome. Mol Ther. 2001;3:591–601.
Zaupa C, Revol-Guyot V, Epstein AL. Improved packaging system for generation of high-level noncytotoxic HSV-1 amplicon vectors using Cre-loxP site-specific recombination to delete the packaging signals of defective helper genomes. Hum Gene Ther. 2003;14:1049–63.
Sabbioni S, Callegari E, Manservigi M, Argnani R, Corallini A, Negrini M, et al. Use of herpes simplex virus type 1-based amplicon vector for delivery of small interfering RNA. Gene Ther. 2007;14:459–64.
Saydam O, Glauser DL, Heid I, Turkeri G, Hilbe M, Jacobs AH, et al. Herpes simplex virus 1 amplicon vector-mediated siRNA targeting epidermal growth factor receptor inhibits growth of human glioma cells in vivo. Mol Ther. 2005;12:803–12.
Saydam O, Saydam N, Glauser DL, Pruschy M, Dinh-Van V, Hilbe M, et al. HSV-1 amplicon-mediated post-transcriptional inhibition of Rad51 sensitizes human glioma cells to ionizing radiation. Gene Ther. 2007;14:1143–51.
Brockman MA, Knipe DM. Herpes simplex virus vectors elicit durable immune responses in the presence of preexisting host immunity. J Virol. 2002;76:3678–87.
Hocknell PK, Wiley RD, Wang XQ, Evans TG, Bowers WJ, Hanke T, et al. Expression of human immunodeficiency virus type 1 gp120 from herpes simplex virus type 1-derived amplicons results in potent, specific, and durable cellular and humoral immune responses. J Virol. 2002;76:5565–80.
Lauterbach H, Ried C, Epstein AL, Marconi P, Brocker T. Reduced immune responses after vaccination with a recombinant herpes simplex virus type 1 vector in the presence of antiviral immunity. J Gen Virol. 2005;86:2401–10.
Oehmig A, Fraefel C, Breakefield XO, Ackermann M. Herpes simplex virus type 1 amplicons and their hybrid virus partners, EBV, AAV, and retrovirus. Curr Gene Ther. 2004;4:385–408.
Kwong AD, Frenkel N. The herpes simplex virus amplicon. IV. Efficient expression of a chimeric chicken ovalbumin gene amplified within defective virus genomes. Virology. 1985;142:421–5.
Zhou G, Roizman B. Characterization of a recombinant herpes simplex virus 1 designed to enter cells via the IL13Ralpha2 receptor of malignant glioma cells. J Virol. 2005;79:5272–7.
Zhou G, Roizman B. Construction and properties of a herpes simplex virus 1 designed to enter cells solely via the IL-13alpha2 receptor. Proc Natl Acad Sci USA. 2006;103:5508–13.
Zhou G, Ye GJ, Debinski W, Roizman B. Engineered herpes simplex virus 1 is dependent on IL13Ralpha 2 receptor for cell entry and independent of glycoprotein D receptor interaction. Proc Natl Acad Sci USA. 2002;99:15124–9.
Wade-Martins R, Smith ER, Tyminski E, Chiocca EA, Saeki Y. An infectious transfer and expression system for genomic DNA loci in human and mouse cells. Nat Biotechnol. 2001;19:1067–70.
Liddington RC, Yan Y, Moulai J, Sahli R, Benjamin TL, Harrison SC. Structure of Simian Virus-40 at 3.8-Å resolution. Nature. 1991;354:278–84.
Nakanishi A, Nakamura A, Liddington R, Kasamatsu H. Identification of amino acid residues within simian virus 40 capsid proteins Vp1, Vp2, and Vp3 that are required for their interaction and for viral infection. J Virol. 2006;80:8891–8.
Li PP, Naknanishi A, Tran MA, Ishizu KI, Kawano M, Phillips M, et al. Importance of Vp1 calcium-binding residues in assembly, cell entry, and nuclear entry of simian virus 40. J Virol. 2003;77:7527–38.
Kawano M, Inoue T, Tsukamoto H, Takaya T, Enomoto T, Takahashi R, et al. The VP2/VP3 minor capsid protein of simian virus 40 promotes the in vitro assembly of the major capsid protein VP1 into particles. J Biol Chem. 2006;281:10164–73.
Colomar MC, Degoumoissahli C, Beard P. Opening and refolding of simian virus 40 and in vitro packaging of foreign DNA. J Virol. 1993;67:2779–86.
Botchan M, Topp W, Sambrook J. Arrangement of simian virus 40 sequences in DNA of transformed cells. Cell. 1976;9:269–87.
Botchan M, Stringer J, Mitchison T, Sambrook J. Integration and excision of SV40 DNA from the chromosome of a transformed cell. Cell. 1980;20:143–52.
Pelkmans L, Kartenbeck J, Helenius A. Caveolar endocytosis of simian virus 40 reveals a new two-step vesicular-transport pathway to the ER. Nat Cell Biol. 2001;3:473–83.
Salunke DM, Caspar DLD, Garcea RL. Self-assembly of purified polyomavirus capsid protein VP1. Cell. 1986;46:895–904.
Sandalon Z, Dalyot-Herman N, Oppenheim AB, Oppenheim A. In vitro assembly of SV40 virions and pseudovirions: vector development for gene therapy. Hum Gene Ther. 1997;8:843–9.
Sandalon Z, Oppenheim A. Self-assembly and protein-protein interactions between the SV40 capsid proteins produced in insect cells. Virology. 1997;237:414–21.
Kimchi-Sarfaty C, Arora M, Sandalon Z, Oppenheim A, Gottesman MM. High cloning capacity of in vitro packaged SV40 vectors with no SV40 virus sequences. Hum Gene Ther. 2003;14:167–77.
Mukherjee S, Abd-El-Latif M, Bronstein M, Ben-nun-Shaul O, Kler S, Oppenheim A. High cooperativity of the SV40 major capsid protein VP1 in virus assembly. PLoS ONE. 2007;2:e765.
Arad U, Zeira E. Abd El-Latif M, Mukherjee S, Mitchell L, Pappo O, et al. Liver-targeted gene therapy by SV40-based vectors using the hydrodynamic injection method. Hum. Gene Ther. 2005;16:361–71.
Kondo R, Feitelson MA, Strayer DS. Use of SV40 to immunize against hepatitis B surface antigen: implications for the use of SV40 for gene transduction and its use as an immunizing agent. Gene Ther. 1998;5:575–82.
Strayer DS, Agrawal L, Cordelier P, Liu B, Louboutin JP, Marusich E, et al. Long-term gene expression in dividing and nondividing cells using SV40-derived vectors. Mol Biotechnol. 2006;34:257–70.
Cordelier P, Morse B, Strayer DS. Targeting CCR5 with siRNAs: using recombinant SV40-derived vectors to protect macrophages and microglia from R5-tropic HIV. Oligonucleotides. 2003;13:281–94.
Kimchi-Sarfaty C, Brittain S, Garfield S, Caplen NJ, Tang QQ, Gottesman MM. Efficient delivery of RNA interference effectors via in vitro-packaged SV40 pseudovirions. Hum Gene Ther. 2005;16:1110–5.
Kimchi-Sarfaty C, Garfield S, Alexander NS, Ali S, Cruz C, Chinnasamy D, et al. The pathway of uptake of SV40 pseudovirions packaged in vitro: from MHC class I receptors to the nucleus. Gene Ther Mol Biol. 2004;8:439–50.
Steinhauer DA, Skehel JJ. Genetics of influenza viruses. Annu Rev Genet. 2002;36:305–32.
Ohuchi M, Asaoka N, Sakai T, Ohuchi R. Roles of neuraminidase in the initial stage of influenza virus infection. Microbes Infect. 2006;8:1287–93.
Wiley DC, Skehel JJ. The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu Rev Biochem. 1987;56:365–94.
Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu Rev Biochem. 2000;69:531–69.
Wagner R, Matrosovich M, Klenk HD. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev Med Virol. 2002;12:159–66.
White JM, Hoffman LR, Arevalo JH, Wilson IA. Attachment and entry of influenza virus into host cells. In: Chiu W, Burnett RM, Garcea RL, editors. Structural biology of viruses. New York: Oxford University Press; 1997. p. 80–104.
Almeida JD, Edwards DC, Brand CM, Heath TD. Formation of virosomes from influenza subunits and liposomes. Lancet. 1975;2:899–901.
de Bruijn IA, Nauta J, Gerez L, Palache AM. Virosomal influenza vaccine: a safe and effective influenza vaccine with high efficacy in elderly and subjects with low pre-vaccination antibody titers. Virus Res. 2004;103:139–45.
Huckriede A, Bungener L, Stegmann T, Daemen T, Medema J, Palache AM, et al. The virosome concept for influenza vaccines. Vaccine. 2005;23(Suppl 1):S26–38.
Schwaninger R, Waelti E, Zajac P, Wetterwald A, Mueller D, Gimmi CD. Virosomes as new carrier system for cancer vaccines. Cancer Immunol Immunother. 2004;53:1005–17.
Waelti E, Wegmann N, Schwaninger R, Wetterwald A, Wingenfeld C, Rothen-Rutishauser B, et al. Targeting her-2/neu with antirat Neu virosomes for cancer therapy. Cancer Res. 2002;62:437–44.
Bron R, Ortiz A, Wilschut J. Cellular cytoplasmic delivery of a polypeptide toxin by reconstituted influenza virus envelopes (virosomes). Biochemistry. 1994;33:9110–7.
Schoen P, Chonn A, Cullis PR, Wilschut J, Scherrer P. Gene transfer mediated by fusion protein hemagglutinin reconstituted in cationic lipid vesicles. Gene Ther. 1999;6:823–32.
de Jonge J, Leenhouts JM, Holtrop M, Schoen P, Scherrer P, Cullis PR, et al. Cellular gene transfer mediated by influenza virosomes with encapsulated plasmid DNA. Biochem J. 2007;405:41–9.
de Jonge J, Holtrop M, Wilschut J, Huckriede A. Reconstituted influenza virus envelopes as an efficient carrier system for cellular delivery of small-interfering RNAs. Gene Ther. 2006;13:400–11.
Judge AD, Bola G, Lee AC, MacLachlan I. Design of noninflammatory synthetic siRNA mediating potent gene silencing in vivo. Mol Ther. 2006;13:494–505.
Zalipsky S, Hansen CB, Oaks JM, Allen TM. Evaluation of blood clearance rates and biodistribution of poly(2-oxazoline)-grafted liposomes. J Pharm Sci. 1996;85:133–7.
Weissig V, Whiteman KR, Torchilin VP. Accumulation of protein-loaded long-circulating micelles and liposomes in subcutaneous Lewis lung carcinoma in mice. Pharm Res. 1998;15:1552–6.
Moghimi SM, Szebeni J. Stealth liposomes and long circulating nanoparticles: critical issues in pharmacokinetics, opsonization and protein-binding properties. Prog Lipid Res. 2003;42:463–78.
Chams V, Bonnafous P, Stegmann T. Influenza hemagglutinin mediated fusion of membranes containing poly(ethylene-glycol) grafted lipids: new insights into the fusion mechanism. FEBS Lett. 1999;448:28–32.
Liang W, Levchenko TS, Torchilin VP. Encapsulation of ATP into liposomes by different methods: optimization of the procedure. J Microencapsul. 2004;21:251–61.
Steenpass T, Lung A, Schubert R. Tresylated PEG-sterols for coupling of proteins to preformed plain or PEGylated liposomes. Biochim Biophys Acta. 2006;1758:20–8.
Mastrobattista E, Schoen P, Wilschut J, Crommelin DJ, Storm G. Targeting influenza virosomes to ovarian carcinoma cells. FEBS Lett. 2001;509:71–6.
Khoury M, Louis-Plence P, Escriou V, Noel D, Largeau C, Cantos C, et al. Efficient new cationic liposome formulation for systemic delivery of small interfering RNA silencing tumor necrosis factor alpha in experimental arthritis. Arthritis Rheum. 2006;54:1867–77.
Kumar VV, Singh RS, Chaudhuri A. Cationic transfection lipids in gene therapy: successes, set-backs, challenges and promises. Curr Med Chem. 2003;10:1297–306.
Ewert K, Slack NL, Ahmad A, Evans HM, Lin AJ, Samuel CE, et al. Cationic lipid-DNA complexes for gene therapy: understanding the relationship between complex structure and gene delivery pathways at the molecular level. Curr Med Chem. 2004;11:133–49.
Karmali PP, Chaudhuri A. Cationic liposomes as non-viral carriers of gene medicines: resolved issues, open questions, and future promises. Med Res Rev. 2007;27:696–722.
Ochiai H, Kurokawa M, Matsui S, Yamamoto T, Kuroki Y, Kishimoto C, et al. Infection enhancement of influenza A NWS virus in primary murine macrophages by anti-hemagglutinin monoclonal antibody. J Med Virol. 1992;36:217–21.
Tamura M, Webster RG, Ennis FA. Subtype cross-reactive, infection-enhancing antibody responses to influenza A viruses. J Virol. 1994;68:3499–504.
Cusi MG, Terrosi C, Savellini GG, Di Genova G, Zurbriggen R, Correale P. Efficient delivery of DNA to dendritic cells mediated by influenza virosomes. Vaccine. 2004;22:735–9.
Zhu X, Meng G, Dickinson BL, Li X, Mizoguchi E, Miao L, et al. MHC class I-related neonatal Fc receptor for IgG is functionally expressed in monocytes, intestinal macrophages, and dendritic cells. J Immunol. 2001;166:3266–76.
Kuroya M, Ishida N. Newborn virus pneumonitis (type Sendai). II. The isolation of a new virus possessing hemagglutinin activity. Yokohama Med Bull. 1953;4:217–33.
Okada Y. Sendai virus-induced cell-fusion. Methods Enzymol. 1993;221:18–41.
Kaneda Y. Applications of hemagglutinating virus of Japan in therapeutic delivery systems. Expert Opin Drug Deliv. 2008;5:221–33.
Bagai S, Puri A, Blumenthal R, Sarkar DP. Hemagglutinin-neuraminidase enhances F protein-mediated membrane fusion of reconstituted Sendai virus envelopes with cells. J Virol. 1993;67:3312–8.
Bagai S, Sarkar DP. Targeted delivery of hygromycin B using reconstituted Sendai viral envelopes lacking hemagglutinin-neuraminidase. FEBS Lett. 1993;326:183–8.
Ramani K, Bora RS, Kumar M, Tyagi SK, Sarkar DP. Novel gene delivery to liver cells using engineered virosomes. FEBS Lett. 1997;404:164–8.
Kaneda Y, Iwai K, Uchida T. Increased expression of DNA cointroduced with nuclear protein in adult rat liver. Science. 1989;243:375–8.
Kato K, Nakanishi M, Kaneda Y, Uchida T. Okada Y. Expression of hepatitis B virus surface antigen in adult rat liver. Co-introduction of DNA and nuclear protein by a simplified liposome method. J Biol Chem. 1991;266:3361–4.
Dzau VJ, Mann MJ, Morishita R, Kaneda Y. Fusigenic viral liposome for gene therapy in cardiovascular diseases. Proc Natl Acad Sci USA. 1996;93:11421–5.
Nakamura N, Hart DA, Frank CB, Marchuk LL, Shrive NG, Ota N, et al. Efficient transfer of intact oligonucleotides into the nucleus of ligament scar fibroblasts by HVJ-cationic liposomes is correlated with effective antisense gene inhibition. J Biochem (Tokyo). 2001;129:755–9.
Kaneda Y, Nakajima T, Nishikawa T, Yamamoto S, Ikegami H, Suzuki N, et al. Hemagglutinating virus of Japan (HVJ) envelope vector as a versatile gene delivery system. Mol Ther. 2002;6:219–26.
Kaneda Y, Yamamoto S, Nakajima T. Development of HVJ envelope vector and its application to gene therapy. Adv Genet. 2005;53:307–32.
Nakanishi M, Uchida T, Kim J, Okada Y. Glycoproteins of Sendai virus (HVJ) have a critical ratio for fusion between virus envelopes and cell membranes. Exp Cell Res. 1982;142:95–101.
Zhang QX, Li Y, Shi YH, Zhang YL. HVJ envelope vector, a versatile delivery system: Its development, application, and perspectives. Biochem Biophys Res Commun. 2008;373:345–9.
GenomONE-Neo HVJ Envelope Transfection Kit : Cosmo Bio Co., Ltd. http://www.cosmobio.co.jp/export_e/products/cells/products_ISK_20070531.asp (accessed 7/19/09).
Mima H, Tomoshige R, Kanamori T, Tabata Y, Yamamoto S, Ito S, et al. Biocompatible polymer enhances the in vitro and in vivo transfection efficiency of HVJ envelope vector. J Gene Med. 2005;7:888–97.
Mima H, Yamamoto S, Ito M, Tomoshige R, Tabata Y, Tamai K, et al. Targeted chemotherapy against intraperitoneally disseminated colon carcinoma using a cationized gelatin-conjugated HVJ envelope vector. Mol Cancer Ther. 2006;5:1021–8.
Kawachi M, Tamai K, Saga K, Yamazaki T, Fujita H, Shimbo T, et al. Development of tissue-targeting hemagglutinating virus of Japan envelope vector for successful delivery of therapeutic gene to mouse skin. Hum Gene Ther. 2007;18:881–94.
Ito M, Yamamoto S, Nimura K, Hiraoka K, Tamai K, Kaneda Y. Rad51 siRNA delivered by HVJ envelope vector enhances the anti-cancer effect of cisplatin. J Gene Med. 2005;7:1044–52.
Watanabe A, Arai M, Yamazaki M, Koitabashi N, Wuytack F, Kurabayashi M. Phospholamban ablation by RNA interference increases Ca2+ uptake into rat cardiac myocyte sarcoplasmic reticulum. J Mol Cell Cardiol. 2004;37:691–8.
Minamisawa S, Hoshijima M, Chu GX, Ward CA, Frank K, Gu YS, et al. Chronic phospholamban-sarcoplasmic reticulum calcium ATPase interaction is the critical calcium cycling defect in dilated cardiomyopathy. Cell. 1999;99:313–22.
Sioud M. Induction of inflammatory cytokines and interferon responses by double-stranded and single-stranded siRNAs is sequence-dependent and requires endosomal localization. J Mol Biol. 2005;348:1079–90.
Kurooka M, Kaneda Y. Inactivated Sendai virus particles eradicate tumors by inducing immune responses through blocking regulatory T cells. Cancer Res. 2007;67:227–36.
Fujihara A, Kurooka M, Miki T, Kaneda Y. Intratumoral injection of inactivated Sendai virus particles elicits strong antitumor activity by enhancing local CXCL10 expression and systemic NK cell activation. Cancer Immunol Immunother. 2008;57:73–84.
ACKNOWLEDGEMENTS
The authors thank George Leiman for his editorial assistance with this manuscript as well as his insightful aide in the preparation of the figures. This work was supported in part by the Intramural Research Program of the National Institutes of Health, National Cancer Institute and by the Research Participation program at the Center for Biologics Evaluation and Research administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy and the U.S. Food and Drug Administration.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lund, P.E., Hunt, R.C., Gottesman, M.M. et al. Pseudovirions as Vehicles for the Delivery of siRNA. Pharm Res 27, 400–420 (2010). https://doi.org/10.1007/s11095-009-0012-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-009-0012-2