Abstract
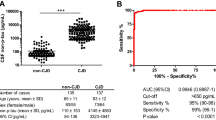
Total tau protein (t-tau) levels in cerebrospinal fluid (CSF) (CSF-tau) are markedly elevated in patients with Creutzfeldt-Jakob disease (CJD). Some CSF-tau may leak into the blood. We evaluated t-tau levels in serum (serum-tau) as a possible marker for the differential diagnosis of CJD from Alzheimer’s disease (AD) and other rapidly progressive dementias (RPD). Serum- and CSF-tau levels were determined in patients with sporadic CJD (n = 12), AD (n = 10) and RPD but no CJD (non-CJD–RPD; n = 9) who showed RPD fulfilling the World Health Organization (WHO) criteria for possible CJD at onset and had a final diagnosis other than CJD. We also analyzed serum-tau levels in healthy volunteers as a control group (n = 10). Serum- as well as CSF-tau levels were significantly elevated in CJD group compared to those in AD, non-CJD–RPD and healthy control groups. Serum-tau would be a simple and useful marker to distinguish CJD from AD and non-CJD–RPD, requiring further large study to confirm this.


Similar content being viewed by others
References
Kapaki E, Kilidireas K, Paraskevas GP et al (2001) Highly increased CSF tau protein and decreased β-amyloid (1–42) in sporadic CJD: a discrimination from Alzheimer’s disease? J Neurol Neurosurg Psychiatry 71:401–403
Reiber H (2001) Dynamics of brain-derived proteins in cerebrospinal fluid. Clin Chim Acta 310:173–186
Van Everbroeck B, Dobbeleir I, De Waele M et al (2004) Differential diagnosis of 201 possible Creutzfeldt-Jakob disease patients. J Neurol 251:298–304
Brown P, Gibbs CJ, Rodgers-Johnson P et al (1994) Human spongiform encephalopathy: the national institutes of health series of 300 cases of experimentally transmitted disease. Ann Neurol 35:513–529
Poser S, Mollenhauer B, Krauß A et al (1999) How to improve the clinical diagnosis of Creutzfeldt-Jakob disease. Brain 122:2345–2351
Will RG, Matthews WB (1984) A retrospective study of Creutzfeldt-Jakob disease in England and Wales 1970–79. I: Clinical features. J Neurol Neurosurg Psychiatry 47:134–140
Tschampa HJ, Neumann M, Zerr I et al (2001) Patients with Alzheimer’s disease and dementia with Lewy bodies mistaken for Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry 71:33–39
Hamaguchi T, Kitamoto T, Sato T et al (2005) Clinical diagnosis of MM2-type sporadic Creutzfeldt-Jakob disease. Neurology 64:643–648
Gelpi E, Heinzi H, Hoftberger R et al (2008) Creutzfeldt-Jakob disease in Austria: an autopsy-controlled study. Neuroepidemiology 30:215–221
WHO (1998) Global surveillance, diagnosis and therapy of human transmissible spongiform encephalopathies. Report of a WHO consultation, Geneva, 9–11 February 1998. http://www.who.int/csr/resources/publications/bse/WHO_EMC_ZDI_98_9/en/. Accessed 27 December 2010
Parchi P, Giese A, Capellari S et al (1999) Classification of sporadic Creutzfeldt-Jakob disease based on molecular and phenotypic analysis of 300 subjects. Ann Neurol 46:224–233
McKhann G, Drachman D, Folstein M et al (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology 34:939–944
Morris JC (1993) The clinical dementia rating (CDR): current version and scoring rules. Neurology 43:2412–2414
Hughes CP, Berg L, Danziger WL et al (1982) A new clinical scale for the staging of dementia. Br J Psychiatry 140:566–572
Folstein M, Folstein S, McHugh P (1975) ‘Mini-mental state’: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Tibbling G (1977) Principles of albumin and IgG analyses in neurological disorder. I. Establishment of reference value. Scand J Clin Lab Invest 37:385–390
Kosik KS, Finch EA (1987) MAP2 and Tau segregate into dendritic and axonal domains after the elaboration of morphologically distinct neuritis: an immunocytochemical study of cultured rat cerebrum. J Neurosci 7:3142–3153
Wunderlich MT, Lins H, Skalej M et al (2006) Neuron-specific enolase and tau protein as neurobiochemical markers of neuronal damage are related to early clinical course and long-term outcome in acute ischemic stroke. Clin Neurol Neurosurg 108:558–563
Sjögren M, Vanderstichele H, Ågren H et al (2001) Tau and Aβ42 in cerebrospinal fluid from healthy adults 21–93 years of age: establishment of reference values. Clin Chem 47:1776–1781
Satoh K, Nakaoke R, Nishiura Y et al (2010) Early detection of sporadic CJD by diffusion-weighted MRI before the onset of symptoms. J Neurol Neurosurg Psychiatry (in press)
Hamaguchi T, Noguchi-Shinohara M, Nozaki I et al (2009) Medical procedures and risk for sporadic Creutzfeldt-Jakob disease, Japan, 1999–2008. Emerg Infect Dis 15:265–271
Nozaki I, Hamaguchi T, Sanjo N et al (2010) Prospective 10-year surveillance of human prion diseases in Japan. Brain 133:3043–3057
Heinemann H, Krasnianski A, Meissner B et al (2007) Creutzfeldt-Jakob disease in Germany: a prospective 12-year surveillance. Brain 130:1350–1359
Acknowledgments
This study was supported in part by the Prion disease and Slow Virus Infection Research Group and Research Committee of Surveillance and Infection Control of Prion Disease, funded by the Ministry of Health, Labour and Welfare, Japan. We thank Ms. Y. Kakuta and Ms. Y. Yamaguchi for excellent technical support, and thank Drs. K. Shima, C. Ishida, A. Morinaga, and A. Sakai for their assistance in data collection.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noguchi-Shinohara, M., Hamaguchi, T., Nozaki, I. et al. Serum tau protein as a marker for the diagnosis of Creutzfeldt-Jakob disease. J Neurol 258, 1464–1468 (2011). https://doi.org/10.1007/s00415-011-5960-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-5960-x