Abstract
In recent years there has been a worldwide increased awareness that children are physically abused by their carers. Radiologists play a vital role in the detection of inflicted injuries. This article reviews the skeletal imaging findings seen in child abuse.
Similar content being viewed by others
Introduction
As discussed by Hobbs and Bilo [1], physical abuse of young children is a serious health problem. Diagnostic imaging plays an important role in the early diagnosis of abuse. The radiologist’s task is to detect findings that are suggestive of abuse, to distinguish abuse from other pathologies and normal variants, and to provide reasonable estimates of fracture age and mechanism of injury. Additionally, a radiologist with specialized knowledge in the field of paediatric radiology may provide expert medical opinions to child protection and law enforcement agencies.
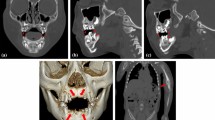
In this article we review the important skeletal imaging findings of abuse. A review paper on neuroimaging in abuse has recently been published, and this topic will not be addressed here [2]. It is, however, worth mentioning that the current controversy in the USA and UK regarding the ‘shaken baby syndrome’ has increased the importance of a detailed evaluation of the skeleton in cases of suspected inflicted neurotrauma (Fig. 1) [2, 3].
Imaging techniques
Fractures are the second most common finding in child abuse after cutaneous findings such as bruises and contusions. The skeletal survey is the cornerstone radiological examination in suspected physical abuse [4]. Although other imaging modalities may be applied, in most cases radiography alone can detect inflicted osseous injuries [5]. The follow-up skeletal survey has been shown to increase the sensitivity of initial radiographic imaging and should be considered in all cases where abuse is strongly suspected (Figs. 2 and 3) [6–9].
A 3-week-old abused girl brought to the emergency room after an apnoeic episode. a, b Initial images of the lower extremity show (a) no abnormality of the right distal femur, and (b) a left distal femur CML (arrow) and no abnormality in the proximal right and left tibiae. c, d Follow-up radiographs 2 weeks later reveal (c) a healing right distal femur CML (arrow) and (d) bilateral proximal tibia CMLs (arrows)
Bone scintigraphy is sometimes used to complement the skeletal survey [10]. Kemp et al. [10] reviewed five studies where bone scintigraphy had greater sensitivity than the skeletal survey [11–15] and two studies where the skeletal survey had a higher sensitivity [16, 17]. Kemp et al. [10] concluded that neither modality alone detected all fractures. Reportedly, bone scintigraphy has a lower sensitivity for the classic metaphyseal lesion (CML) and for skull fractures, but a higher sensitivity for rib fractures [11–16]. The American College of Radiology (ACR) appropriateness criteria state that bone scintigraphy is ‘… indicated when clinical suspicion of abuse remains high and documentation is still necessary’ [18].
CT, US and MRI may be of value in selected cases, but currently cannot replace the radiographic skeletal survey [19–22]. The use of fluorine-18 NaF PET imaging in the detection of occult inflicted fractures has recently been described in a single case; however, its clinical utility in suspected physical abuse requires further research [23].
Imaging protocol
A skeletal survey should be performed in cases of suspected child abuse. The ACR defines the skeletal survey as ‘a systematically performed series of radiographic images that encompasses the entire skeleton’ [24]. The ACR (Table 1) as well as the British Society of Paediatric Radiology (BSPR) (Table 2) [25, 26] have published guidelines for the skeletal survey protocol. The ACR and BSPR guidelines are nearly identical. One difference between the guidelines is the acquisition of oblique radiographs of the ribs. This addition is supported by the findings of Ingram et al. [27] who, in a randomized controlled trial, found that oblique views of the chest increased the sensitivity for the detection of rib fractures by 17% and the specificity by 7%. Hansen et al. [28] compared the conventional two-view chest series to the four-view chest series in 21 abused children. The four-view chest series increased the diagnostic yield, both by including new fractures and by excluding fractures suspected on the two-view series. However, each case had at least one rib fracture visible on the two-view series and there were no cases in which the four-view series excluded all rib fractures seen on the two-view series (Fig. 4).
A 3-month-old abused boy brought to the emergency room because of a ‘crack’ sound in the chest and irritability. a Initial chest radiograph shows an acute left 7th rib fracture (arrow). b Initial oblique images of the chest better demonstrate the left 7th rib fracture and a possible left 8th rib fracture (arrows). c Follow-up oblique images of the chest obtained 2 weeks later show healing left 7th, 8th and 9th rib fractures
Equivocal fractures at all sites should be evaluated with additional projections. Ideally a radiologist should supervise the skeletal survey, and only once it has been reviewed and approved should the examination be considered complete. Because the skeletal survey may become part of legal proceedings, the radiology technologists are identified on the radiographs – either by their initials, or by preallocated codes.
The ACR and SPR guidelines are available online, but are not widely implemented. Kleinman et al. [5] surveyed radiologists at paediatric health-care facilities in the USA and found that imaging protocols varied from the recommended guidelines. In 2007, Schmit et al. [29] queried members of the Asian & Oceanic Society for Paediatric Radiology, the European Society of Paediatric Radiology, the Latin American Society of Pediatric Radiology, and the Society for Pediatric Radiology about the guidelines. Respondents perceived the recommendations as open to interpretation, improvement and research. Both studies found a wide range of imaging practices in cases of suspected abuse. Offiah and Hall [30] and van Rijn et al. [31] retrospectively examined skeletal surveys and found many differences in the number and quality of radiographs performed. They concluded that the available guidelines are generally not implemented in clinical practice. Efforts to improve the quality of skeletal surveys for suspected abuse should be encouraged and there is evidence that standards, at least in the UK, are improving [32].
What is the impact of digital imaging systems on the evaluation of suspected abuse? Generally, digital imaging (CR and DR) has several practical advantages over conventional film-screen radiography, including economic and ergonomic considerations [33]. Postprocessing functions when used optimally may improve visualization of pathology and bone and soft-tissue detail differentiation. Techniques commonly used are magnification, grey-scale, contrast, brightness, nonlinear grey-scale enhancement, nonlinear unsharp masking (edge enhancement), and single or dual exposure energy subtraction. Digital imaging requires particular attention to technical factors, because observed performance may vary with mAs, kVp and CR system resolution. Radiology departments should optimize their digital imaging techniques accordingly [34]. A study by Offiah et al. [35] suggested that neither postprocessing parameters (magnification and edge enhancement) nor method of digital image display (i.e. whether radiographs were printed or viewed from a monitor) affects the diagnostic accuracy of fracture identification in abuse cases. Regardless of the imaging system used and method of image display, emphasis should be placed on improving performance.
Under- and over-diagnosis of abuse may have detrimental effects on children and their carers. It is critical that the skeletal survey be performed according to a rigorous imaging protocol, with careful attention to technique ensuring high-quality radiographs. The skeletal survey should be reviewed by a radiologist with substantial experience in paediatric imaging to ensure accurate interpretation of the findings.
Radiological findings
Rib fractures
Rib fractures are frequently seen in adolescents and adults after severe trauma. Younger children have higher plasticity of their ribcage; the ribs deform before they fracture. This explains the relative scarcity of rib fractures in this age group. Rib fractures in younger children are usually clinically occult and found incidentally [36]. The presence of rib fractures in infants (less than 1 year of age) is highly specific for abuse (Figs. 2, 4 and 5) [37]. One mechanism of rib fracture is anterior-posterior compression of the chest [38, 39]. Excessive leverage of the ribs over the transverse process leads to fractures of the rib head and neck (Fig. 6). Other forms of chest compression and blunt impact may be responsible for rib fractures at other sites.
Schematic representation of the chest during anterior-posterior compression. Compression can result in fractures at: A costotransverse process articulation, B lateral arc, C costochondral junction, D anterior arc, E posterior arc, and F rib head (adapted with permission from Kleinman [37])
Barsness et al. [40] assessed the positive predictive value (PPV) of rib fractures in relation to abuse. In 62 children, a total of 316 rib fractures were identified. In 51 children (82%) the fractures were due to abuse. In children less than 3 years of age the PPV of rib fractures for abuse was 95%. Fractures of the first rib appear to require even greater force than other rib fractures, and strongly suggest abuse [41].
Although rib factures have a high specificity for abuse, they have been described in other scenarios where similar strong forces may have occurred. Mid-posterior rib arc fractures have been reported after vaginal delivery [42–47]. In most cases the babies were large and the deliveries were difficult or assisted. When data of five studies on birth trauma were combined, yielding a total 115,756 live births, no single case of rib fractures was reported [48–52]. Until recently, cardiopulmonary resuscitation was not considered to cause rib fractures in normal infants. A post-mortem study of 91 infants found no rib fractures after resuscitation efforts [53]. The authors concluded that ‘when rib fractures are encountered in an otherwise normal infant, child abuse must be considered’. A recent development is the introduction of two-handed infant CPR with the hands encircling the chest [54]. This technique resembles the way perpetrators hold their children when they are reportedly shaken. Clouse and Lantz [55] reported four premature neonates (1 day to 3 months) who died after resuscitation. In all cases abuse was excluded and autopsy showed posterior rib fractures. Rib fractures are well described in metabolic bone disease of prematurity [56]. Rib fractures can also be seen with metabolic disorders and skeletal dysplasias. In osteogenesis imperfecta, the fractures most commonly occur in the long bones, although rib fractures can be found (Fig. 7) [57].
Classic metaphyseal lesion
The CML is a highly specific finding for abuse [58, 59]. CMLs are most often found in the distal femur, proximal and distal tibia/fibula and proximal humerus (Figs. 3 and 8) [38]. CMLs are characteristically seen in infants, and above 1 year of age the finding is not specific. Caffey was the first to use the terms “corner fracture” and “bucket handle fracture” to describe the metaphyseal fracture patterns seen in abuse [60]. The radiographic appearance of the CML corner or bucket handle vary depending on the size of the fragment and the position of the extremity relative to the X-ray beam (Fig. 9) [58]. The mechanism of injury for the CML involves a shearing force; the resulting fracture line is nearly parallel to the physis centrally, but veers to undercut the subperiosteal bone collar peripherally [59]. In manual assaults, the extremities may undergo substantial torsional and tractional forces leading to these strong indicators of inflicted injury. Healing of CMLs is variable. Sclerosis may be present at the injury site (Fig. 3). If the CML is associated with significant displacement and periosteal stripping there may be conspicuous sclerosis and subperiosteal new bone formation (Fig. 10). Most CMLs heal without subperiosteal new bone formation. Kleinman et al. [61] described a metaphyseal lucency that grows away from the growth plate invaginating the metaphysis that may be used to determine chronicity.
A 2-month-old girl presenting with convulsions. a The skeletal survey reveals a right distal tibia CML (arrow) and subperiosteal new bone formation (arrowheads). b Axial CT image of the brain demonstrates absence of grey–white matter differentiation (consistent with severe hypoxia) and a small subdural haematoma (arrowhead)
Schematic representation of corner and bucket handle fractures. A tangential view results in a corner fracture pattern (left images). An angled view results in a bucket-handle pattern (right images). Top images show a diffuse bone injury, the bottom images a localized injury (reprinted with permission from Kleinman [58])
A radiographic pattern resembling the CML can be seen in other conditions. As early as 1957, Caffey noted that birth trauma can cause metaphyseal injuries [60]. In a retrospective analysis over a 22-year period, O’Connell and Donoghue [62] reported three neonates with metaphyseal fractures resembling CMLs after lower segment caesarian sections. Iatrogenic metaphyseal injuries have been seen after orthopaedic manipulation for treatment of clubfoot [63].
Metabolic bone diseases and bone dysplasias can have metaphyseal changes similar to the CML. For example, in rickets the characteristic findings of metaphyseal irregularity and physeal widening may be accompanied by osseous fragments resembling the CML [58]. In most cases the diagnosis of rickets will be fairly straightforward and laboratory findings will generally differentiate between abuse and rickets. The Schmid-type metaphyseal chondrodysplasia (OMIM #156500) and the spondylometaphyseal dysplasia, corner fracture type (OMIM %184255) can have marginal metaphyseal fragments. In both dysplasias the lesions lack the typical healing pattern noted with the CML, and the skeletal survey will reveal other abnormalities associated with the given skeletal dysplasia.
Long-bone fractures
Paediatric long bone diaphyseal (shaft) fractures are a common finding in the emergency department and in general have a low specificity for abuse (Table 3). The older the child, the more likely a long-bone fracture occurred as a result of accidental trauma. Long-bone fractures in nonambulatory infants are concerning for abuse: ‘those who don’t cruise, don’t bruise’ [64] (Fig. 11). The mechanism for the fractures in infants is usually an indirect force. The perpetrator grabs the infant by an extremity and applies a bending or rotational force that results in a transverse, oblique or spiral fracture.
A 7-month-old abused girl in whom a carer admitted to the physical abuse. a Radiograph of the right humerus shows an oblique diaphyseal fracture (arrow). b Radiograph of the forearm reveals transverse fractures of the mid-radius and ulna (arrows). c Radiograph of the left arm shows a transverse fracture of the radius (arrow) and a buckle fracture of the ulna (arrowhead). d Chest radiograph shows multiple healing right anterior rib fractures (see inset)
Carty and Pierce [65] retrospectively studied a cohort of 467 children in whom abuse was suspected (proven in 93%); 77 children had isolated long-bone fractures. The most common sites were the humerus (n=27, 1 metaphyseal) and femur (n=25, two metaphyseal). In a post-mortem study of 31 infants by Kleinman et al. [66], of 165 fractures (skull excluded), 8 were diaphyseal fractures of the long bones.
Other fractures
A linear skull fractures can be seen after a fall from a height of 3–4 feet (about 1 m), and occasionally after a fall from a height less than this [67–69]. The younger the child presenting with a skull fracture the higher the likelihood of abuse, particularly in the absence of a history of trauma [70]. Complex and depressed skull fractures have a higher PPV for abuse than simple linear fractures [70, 71]. A relatively rare complication of skull fractures is the development of a growing fracture (leptomeningeal cyst, traumatic meningocele, cerebrocranial erosion, cephalhydrocele; Fig. 12). When there is clinical concern for leptomeningeal cyst, a CT or MRI scan is indicated.
Pelvic fractures in young children are almost always seen following significant trauma such as motor vehicle accidents. However, there have been case reports of pelvic fractures due to abuse [72–75]. Most of these children were girls who were sexually abused. In infants, care should be taken to exclude normal developmental variants of the superior pubic ramus that may simulate a fracture [76].
A wide variety of other skeletal injuries have been described in abused children [37].
Dating fractures
O’Connor and Cohen outlined radiographic features that may be used to date fractures based on their personal experience (Table 4) [77]. Recently Prosser et al. [78] reported an analysis in which 1,556 publications were systematically reviewed. Three studies, with data on 189 children (only 56 children were younger than 5 years, the age group most vulnerable for abuse) met the authors’ inclusion criteria. The key findings of the review were quite similar to the table of O’Connor and Cohen. Prosser et al. [78] concluded that fracture dating in children is an inexact science, but that radiologists should be able to differentiate recent from old fractures.
Although estimation of fracture age should be approached with caution, experienced paediatric radiologists should be able to make informed judgements as to whether or not fractures (excluding skull, spine fractures and some CMLs) are in a healing phase. Healing can usually be judged as early or mature, and when multiple fractures are present, it is often possible to state if the fractures are of similar or different ages.
Imaging plays an import role in the detection and documentation of abuse, and failure to make a correct diagnosis may have serious consequences. In a retrospective analysis Carty and Pierce [65] showed that out of 435 abuse cases, imaging initially missed 55. Of these 55 children, 6 (12%) died and 10 (20%) survived with a handicap. Careful interpretation of skeletal surveys by radiologists with experience in paediatric imaging is mandatory in cases of suspected abuse. It is the radiologist’s task to distinguish abuse from accidental trauma, normal variants, metabolic bone diseases and skeletal dysplasias. Medical professionals have demonstrated an increasing focus on the problem of child maltreatment. An encouraging sign is the recent establishment of certification of child abuse paediatrics by the American Board of Pediatrics [79]. Paediatric radiologists are a vital resource to these clinicians and must be suitably trained and experienced in the imaging of child abuse and its imitators. An appropriate response to this critical public health concern of child abuse requires a multidisciplinary approach in which paediatric radiologists are active and important members of institutional child protection teams.
References
Hobbs CJ, Bilo RA (2009) Non-accidental trauma: clinical aspects and epidemiology of child abuse. Pediatr Radiol. doi:10.1007/s00247-008-1136-y
Fernando S, Obaldo RE, Walsh IR et al (2008) Neuroimaging of nonaccidental head trauma: pitfalls and controversies. Pediatr Radiol 38:827–838
Jaspan T (2008) Current controversies in the interpretation of non-accidental head injury. Pediatr Radiol 38(S3):378–387
McMahon P, Grossman W, Gaffney M et al (1995) Soft-tissue injury as an indication of child abuse. J Bone Joint Surg Am 77:1179–1183
Kleinman PL, Kleinman PK, Savageau JA (2004) Suspected infant abuse: radiographic skeletal survey practices in pediatric health care facilities. Radiology 233:477–485
Kellogg ND (2007) Evaluation of suspected child physical abuse. Pediatrics 119:1141–1232
American Academy of Pediatrics Section on Radiology (2000) Diagnostic imaging of child abuse. Pediatrics 105:1345–1348
Kleinman PK, Nimkin K, Spevak MR et al (1996) Follow-up skeletal surveys in suspected child abuse. AJR 167:893–896
Zimmerman S, Makoroff K, Care M et al (2005) Utility of follow-up skeletal surveys in suspected child physical abuse evaluations. Child Abuse Negl 29:1075–1083
Kemp AM, Butler A, Morris S et al (2006) Which radiological investigations should be performed to identify fractures in suspected child abuse? Clin Radiol 61:723–736
Jaudes PK (1984) Comparison of radiography and radionuclide bone scanning in the detection of child abuse. Pediatrics 73:166–168
Conway JJ, Collins M, Tanz RR (1993) The role of bone scintigraphy in detecting child abuse. Semin Nucl Med 23:321–333
Haase GM, Ortiz VN, Sfanakis GN (1980) The value of radionuclide bone scanning in the early recognition of deliberate child abuse. J Trauma 20:873–875
Merten DF, Radlowski MA, Leonidas JC (1983) The abused child: a radiological reappraisal. Radiology 146:377–381
Sty JR, Starshak RJ (1983) The role of bone scintigraphy in the evaluation of suspected child abuse. Radiology 146:369–375
Mandelstam SA, Cook D, Fitzgerald M et al (2003) Complementary use of radiological skeletal survey and bone scintigraphy in detection of bony injuries in suspected child abuse. Arch Dis Child 88:387–390
Pickett WJ, Faleski EJ, Chacko A et al (1983) Comparison of radiographic and radionuclide skeletal surveys in battered children. South Med J 76:207–212
Slovis TL, Smith W, Kushner DC et al (2000) Imaging the child with suspected physical abuse. American College of Radiology. ACR Appropriateness Criteria. Radiology 215(Suppl):805–809
Renton J, Kincaid S, Ehrlich PF (2003) Should helical CT scanning of the thoracic cavity replace the conventional chest x-ray as a primary assessment tool in pediatric trauma? An efficacy and cost analysis. J Pediatr Surg 38:793–797
Traub M, Stevenson M, McEvoy S et al (2007) The use of chest computed tomography versus chest X-ray in patients with major blunt trauma. Injury 38:43–47
Elterman T, Beer M, Girschick HJ (2007) Magnetic resonance imaging in child abuse. J Child Neurol 22:170–175
Stranzinger E, Kellenberger CJ, Braunschweig S et al (2007) Whole-body STIR MR imaging in suspected child abuse: an alternative to skeletal survey radiography? Eur J Radiol Extra 63:43–47
Drubach LA, Sapp MV, Laffin S et al (2008) Fluorine-18 NaF PET imaging of child abuse. Pediatr Radiol 38:776–779
American College of Radiology (2006) ACR practice guideline for skeletal surveys in children. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/guidelines/pediatric/skeletal_surveys.aspx. Accessed 5 Feb 2009
American College of Radiology (1997) ACR standards for skeletal surveys in children. Resolution 22. American College of Radiology, Reston, VA
British Society of Paediatric Radiology. Standard for skeletal surveys in suspected non-accidental injury (NAI) in children. www.bspr.org.uk/nai.htm. Accessed 5 Feb 2009
Ingram JD, Connell J, Hay TC (2007) Oblique radiographs of the chest in nonaccidental trauma. Emerg Radiol 7:42–46
Hansen KK, Prince JS, Nixon GW (2008) Oblique chest views as a routine part of skeletal surveys performed for possible physical abuse – is this practice worthwhile? Child Abuse Negl 2008 32:155–159
Schmit P, Abdolell M, Bellemare S et al (2007) Inflicted injury in children: variability of imaging practice among pediatric radiologists. Pediatr Radiol 37(Suppl 1):S49
Offiah AC, Hall CM (2003) Observational study of skeletal surveys in suspected non-accidental injury. Clin Radiol 58:702–705
van Rijn RR, Kieviet N, Hoekstra R et al (2008) Radiology in suspected non accidental injury: theory and practice in the Netherlands. Eur J Radiol. doi:10.1016/j.ejrad.2008.02.014
Swinson S, Tapp M, Brindley R et al (2008) An audit of skeletal surveys for suspected non-accidental injury following publication of the British Society of Paediatric Radiology guidelines. Clin Radiol 63:651–656
Schaefer-Prokop CM, Prokop M (1997) Storage phosphor radiography. Eur Radiol 7(Suppl 3):S58–S65
Kleinman PL, Zurakowski D, Strauss KJ et al (2008) Detection of simulated inflicted metaphyseal fractures in a fetal pig model: image optimization and dose reduction with computed radiography. Radiology 247:381–390
Offiah AC, Moon L, Hall CM et al (2006) Diagnostic accuracy of fracture detection in suspected non-accidental injury: the effect of edge enhancement and digital display on observer performance. Clin Radiol 61:163–173
Stover B (2007) Diagnostic imaging in child abuse. Radiologe 47:1037–1048
Kleinman PK (1998) Diagnostic imaging of child abuse, 2nd edn. Mosby, St. Louis
Kleinman PK, Marks SC Jr, Nimkin K et al (1996) Rib fractures in 31 abused infants: postmortem radiologic-histopathologic study. Radiology 200:807–810
Worn MJ, Jones MD (2007) Rib fractures in infancy: establishing the mechanisms of cause from the injuries – a literature review. Med Sci Law 47:200–212
Barsness KA, Cha ES, Bensard DD et al (2003) The positive predictive value of rib fractures as an indicator of nonaccidental trauma in children. J Trauma 54:1107–1110
Strouse PJ, Owings CL (1995) Fractures of the first rib in child abuse. Radiology 197:763–765
Barry PW, Hocking MD (1993) Infant rib fracture – birth trauma or non-accidental injury. Arch Dis Child 68:250
Bulloch B, Schubert CJ, Brophy PD et al (2000) Cause and clinical characteristics of rib fractures in infants. Pediatrics 105:E48
Durani Y, DePiero AD (2006) Images in emergency medicine. Fracture of left clavicle and left posterior rib due to birth trauma. Ann Emerg Med 47:210, 215
Hartmann RW Jr (1997) Radiological case of the month. Rib fractures produced by birth trauma. Arch Pediatr Adolesc Med 151:947–948
Rizzolo PJ, Coleman PR (1989) Neonatal rib fracture: birth trauma or child abuse? J Fam Pract 29:561–563
Thomas PS (1977) Rib fractures in infancy. Ann Radiol (Paris) 20:115–122
Alexander JM, Leveno KJ, Hauth J et al (2006) Fetal injury associated with cesarean delivery. Obstet Gynecol 108:885–890
Gudmundsson S, Henningsson AC, Lindqvist P (2005) Correlation of birth injury with maternal height and birthweight. BJOG 112:764–767
Rubin A (1964) Birth injuries: incidence, mechanisms and end results. Obstet Gynecol 23:218–221
Levine MG, Holroyde J, Woods JR Jr et al (1984) Birth trauma: incidence and predisposing factors. Obstet Gynecol 63:792–795
Bhat BV, Kumar A, Oumachigui A (1994) Bone injuries during delivery. Indian J Pediatr 61:401–405
Spevak MR, Kleinman PK, Belanger PL et al (1994) Cardiopulmonary resuscitation and rib fractures in infants. A postmortem radiologic-pathologic study. JAMA 272:617–618
International Liaison Committee on Resuscitation (2006) The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: pediatric basic and advanced life support. Pediatrics 117:e955–e977
Clouse JR, Lantz PE (2008) Posterior rib fractures in infants associated with cardiopulmonary resuscitation. American Academy of Forensic Sciences, 60th annual meeting, Washington
Smurthwaite D, Wright N, Russell S et al (2008) How common are rib fractures in extremely low birth weight preterm infants? Arch Dis Child Fetal Neonatal Ed. doi:10.1136/adc.2007.136853
Feldman KW, Brewer DK (1984) Child abuse, cardiopulmonary resuscitation, and rib fractures. Pediatrics 73:339–342
Kleinman PK (2008) Problems in the diagnosis of metaphyseal fractures. Pediatr Radiol 38(Suppl 3):S388–S394
Kleinman PK, Marks SC Jr (1995) Relationship of the subperiosteal bone collar to metaphyseal lesions in abused infants. J Bone Joint Surg Am 77A:1471–1476
Caffey J (1957) Some traumatic lesions in growing bones other than fractures and dislocations: clinical and radiological features: The Mackenzie Davidson Memorial Lecture. Br J Radiol 30:225–238
Kleinman PK, Marks SC Jr, Spevak MR et al (1991) Extension of growth-plate cartilage into the metaphysis: a sign of healing fracture in abused infants. AJR 156:775–779
O’Connell AM, Donoghue VB (2008) Classic metaphyseal lesions follow uncomplicated caesarean section NOT brittle bone disease. Pediatr Radiol 38:600
Grayev AM, Boal DK, Wallach DM et al (2001) Metaphyseal fractures mimicking abuse during treatment for clubfoot. Pediatr Radiol 31:559–563
Sugar NF, Taylor JA, Feldman KW (1999) Bruises in infants and toddlers: those who don’t cruise rarely bruise. Puget Sound Pediatric Research Network. Arch Pediatr Adolesc Med 153:399–403
Carty H, Pierce A (2002) Non-accidental injury: a retrospective analysis of a large cohort. Eur Radiol 12:2919–2925
Kleinman PK, Marks SC Jr, Richmond JM et al (1995) Inflicted skeletal injury: a postmortem radiologic-histopathologic study in 31 infants. AJR 165:647–650
Warrington SA, Wright CM (2001) Accidents and resulting injuries in premobile infants: data from the ALSPAC study. Arch Dis Child 85:104–107
Nimityongskul P, Anderson LD (1987) The likelihood of injuries when children fall out of bed. J Pediatr Orthop 7:184–186
Lyons TJ, Oates RK (1993) Falling out of bed: a relatively benign occurrence. Pediatrics 92:125–127
Hobbs CJ (1984) Skull fracture and the diagnosis of abuse. Arch Dis Child 59:246–252
Lee AC, Ou Y, Fong D (2003) Depressed skull fractures: a pattern of abusive head injury in three older children. Child Abuse Negl 27:1323–1329
Johnson K, Chapman S, Hall CM (2004) Skeletal injuries associated with sexual abuse. Pediatr Radiol 34:620–623
Starling SP, Heller RM, Jenny C (2002) Pelvic fractures in infants as a sign of physical abuse. Child Abuse Negl 26:475–480
Prendergast NC, deRoux SJ, Adsay NV (1998) Non-accidental pediatric pelvic fracture: a case report. Pediatr Radiol 28:344–346
Ablin DS, Greenspan A, Reinhart MA (1992) Pelvic injuries in child abuse. Pediatr Radiol 22:454–457
Perez-Rossello JM, Connolly SA, Newton AW et al (2008) Pubic ramus radiolucencies in infants: the good, the bad, and the indeterminate. AJR 190:1481–1486
O’Connor JF, Cohen J (1998) Dating fractures. In: Kleinman PK (ed) Diagnostic imaging of child abuse, 2nd edn. Mosby, St. Louis, pp 168–177
Prosser I, Maguire S, Harrison SK et al (2005) How old is this fracture? Radiologic dating of fractures in children: a systematic review. AJR 184:1282–1286
Block RW, Palusci VJ (2006) Child abuse pediatrics: a new pediatric subspecialty. J Pediatr 148:711–712
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License, which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Offiah, A., van Rijn, R.R., Perez-Rossello, J.M. et al. Skeletal imaging of child abuse (non-accidental injury). Pediatr Radiol 39, 461–470 (2009). https://doi.org/10.1007/s00247-009-1157-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-009-1157-1