Abstract
Objectives
The WHO recommends artemisinin-based combination therapies for treatment of uncomplicated falciparum malaria. At least 15 African countries have adopted artesunate plus amodiaquine as treatment policy. As no pharmacokinetic data on this combination have been published to date, we investigated its pharmacokinetic interactions and tolerability in healthy volunteers in Africa.
Methods
In a randomized, three-phase, cross-over study, amodiaquine (10 mg/kg) and artesunate (4 mg/kg) were given as single oral doses to 15 healthy volunteers. Artesunate was given to all volunteers on day 0. On day 7 they received either amodiaquine or amodiaquine plus artesunate and the alternative regimen on day 28. The pharmacokinetics of artesunate and amodiaquine and their main active metabolites dihydroartemisinin and desethylamodiaquine were compared following monotherapy and combination therapy using analysis of variance.
Results
Thirteen volunteers completed the study, and pharmacokinetic parameters could be determined for twelve volunteers. When given in combination, the mean AUC was lower for dihydroartemisinin [ratio 67% (95% CI 51–88%); P = 0.008] and desethylamodiaquine [ratio 65% (95% CI 46–90%); P = 0.015] when compared with monotherapy. Adverse events of concern occurred in four volunteers (27%): grade 3 transaminitis (n = 1), neutropaenia (n = 2), and hypersensitivity (n = 1).
Conclusion
The total drug exposure to both drugs was reduced significantly when they were given in combination. The clinical significance of these interactions is unclear and must be studied in malaria patients. The frequency and nature of adverse events among the healthy volunteers were of concern, and suggest laboratory monitoring would be needed in malaria patients treated with artesunate plus amodiaquine.
Similar content being viewed by others
Introduction
Since Plasmodium falciparum has developed resistance to almost all anti-malarial drugs, the use of combinations of effective antimalarials with different mechanisms of action is required to improve cure rates and delay drug resistance. The World Health Organisation (WHO) now recommends treatment of uncomplicated falciparum malaria with one of several artemisinin-based combination therapies (ACTs), including artesunate plus amodiaquine [1]. To date at least 15 African countries have adopted artesunate plus amodiaquine as first-line malaria treatment policy [2].
Although the limited data available suggest that the combination of artesunate and amodiaquine is well tolerated as short-course treatment, there are two safety concerns that have not yet been fully addressed. Neutropaenia and hepatitis curtailed the use of amodiaquine as prophylaxis in the 1980s [3–5]. A recent randomised, controlled trial comparing treatment with amodiaquine alone or in combination with artesunate found marked, asymptomatic neutropaenia on day 28 (NCI grade 3–4, absolute neutrophil counts 306–900 μL−1) in 6% of 153 children with uncomplicated falciparum malaria, all of whom had normal baseline absolute neutrophil counts [6]. We have previously reported a case of hepatitis in this group of volunteers that developed after the second dose of amodiaquine and was considered probably related to amodiaquine [7]. A similar report of delayed-onset asymptomatic hepatitis has been described in healthy American volunteers who had received artesunate plus amodiaquine alone followed by artesunate plus amodiaquine plus efavirenz, resulting in early study discontinuation [8]. In that study, efavirenz was thought to have caused an increase in amodiaquine concentrations by competitive inhibition of the P450 cytochrome enzymes that metabolise amodiaquine. With the widespread use of artesunate plus amodiaquine treatment in Africa, these studies support the need for laboratory monitoring of the treatment’s safety, particularly if antiretrovirals are used concomitantly [1].
Pharmacokinetic data are still sparse for amodiaquine. After oral administration, amodiaquine hydrochloride is rapidly absorbed and undergoes rapid and extensive metabolisation to desethylamodiaquine, the main active metabolite. Amodiaquine has a short elimination half-life (approximately 5 h), while that for desethylamodiaquine is much longer (6–18 days) [9, 10].
There are several pharmacokinetic studies on oral artesunate in healthy volunteers and malaria patients that give broadly consistent results [11, 12]. Artesunate is rapidly absorbed, rapidly converted to its main active metabolite dihydroartemisinin and rapidly cleared (elimination half-life generally <1 h). Dihydroartemisinin has similar pharmacokinetic characteristics but has a slightly longer elimination half-life. There is wide inter-individual variation in artesunate and dihydroartemisinin pharmacokinetic parameters.
No pharmacokinetic interaction data have yet been published on amodiaquine when used in combination with artesunate. In view of the forthcoming widespread use of this combination in Africa, our study aimed to investigate potential pharmacokinetic interactions between these antimalarials and assess their tolerability in healthy volunteers in Africa.
Methods
Study subjects and study design
Male or female healthy normal volunteers who provided written informed consent and met the following criteria were eligible to participate in the study: aged 18–45 years; no abnormalities on medical history, clinical examination, laboratory safety assessment (full blood count, differential white cell count, routine liver and renal function tests) or electrocardiogram; and a negative pregnancy test (for female volunteers). Volunteers were excluded if they were smokers (>5 cigarettes/day), had taken antimalarials or been in a malarial area in the preceding 8 weeks, had malaria parasites on a thick smear, used recreational drugs, or had ingested any alcohol or any medicines (including over-the-counter preparations) in the week preceding study commencement.
This was a randomised three-phase crossover study. All volunteers took artesunate (4 mg/kg as Arsumax, 50 mg tablets, Sanofi-Aventis), the drug with the shorter elimination half-life, in the first phase, prior to the administration of amodiaquine. In the second phase, 7 days later, the volunteers were randomly allocated to one of two treatment groups: group 1 received a single oral dose of artesunate (4 mg/kg) plus amodiaquine (10 mg base/kg as Camoquin, 200 mg tablets, Parke Davis), and group 2 received a single oral dose of amodiaquine (10 mg/kg) alone. In phase three, 21 days later, the groups received the alternative regimen. All trial drugs were given under direct supervision with 200 ml tap water on an empty stomach after an overnight fast. No caffeinated drinks were allowed during the study period. Standardised meals were offered, commencing with breakfast at 2 h post-dose. Volunteers in phase one had blood samples collected before taking artesunate and at 0.25, 0.50, 0.75, 1.0, 1.5, 2, 3, 4, 6, 8 and 12 h after artesunate administration. In phases two and three (i.e. volunteers receiving artesunate plus amodiaquine or amodiaquine alone) venous blood samples were collected pre-dose and at 0.25, 0.5, 0.75, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, 48 and 72 h, and days 4, 5, 7, 10, 14 and 20 post-dose. At each time two 5-ml venous blood samples were collected in tubes containing sodium heparin anticoagulant, while three 5-ml samples were collected at each time point for the first 12 h from those volunteers receiving both drugs. Each sample was centrifuged within 5 min of collection and the plasma transferred to separate plastic cryotubes and frozen at −70°C until analysed for artesunate, dihydroartemisinin, amodiaquine and desethylamodiaquine. Volunteers remained in the study ward for the first 12 h of each phase; thereafter specimens were collected at outpatient visits.
A clinical examination and laboratory safety tests were performed during screening and 6 days after artesunate administration and 20 days after administration of both amodiaquine and amodiaquine plus artesunate. A 12-lead electrocardiogram (ECG) was recorded for each volunteer during screening and approximately 2 h after each drug dose. The corrected QT interval (QTc) was calculated by dividing the QT interval by the square root of the R-R interval. ECGs were reviewed by C.O. and by a consultant cardiologist. At follow-up visits, the volunteers were asked to report any new symptoms. A targeted physical examination was conducted if indicated. An adverse event together with its relationship to study drugs was defined according to the WHO guidelines [13] and the severity graded using the National Cancer Institute (NCI) Common Toxicity Criteria [14]. All adverse events and concomitant medications taken were recorded. Any significant clinical or laboratory abnormalities or the use of a concomitant medication with a previously described interaction resulted in the volunteer being withdrawn from the study.
Ethical approval
This clinical study was conducted in accordance with the principles laid down by the World Health Assembly of 1975 on Ethics in Human Experimentation and the Helsinki Declaration. The study adhered to the standards established for good clinical practice. The protocol was approved by the University of Cape Town Research Ethics Committee and the WHO Secretariat Committee for Research Involving Human Subjects (SCRIHS). Each volunteer was informed of the objectives, nature and possible risks of the trial. Written informed consent was obtained from every volunteer participating in the study. The volunteers were informed that they were free to withdraw consent at any time.
Drug assays
Artesunate and dihydroartemisinin concentrations in plasma were analysed using the method of Batty and colleagues [15] with minor modifications. Solid-phase extraction of samples was performed using Bond-Elut phenyl extraction cartridges (Varian, Harbour City, CA, USA). After washing the column with 2 ml of water, samples were eluted from the column with 1.5 ml of acetonitrile, which was then evaporated to dryness under nitrogen. Samples were reconstituted in 100 μl of mobile phase (45% acetonitrile, 0.05 M acetic acid, pH 6.0), and 50 μl was injected onto the column. HPLC was carried out on a Symmetry C 8, 5 μm, 15 cm × 4.6 mm HPLC column (Waters, Milford, MA, USA) using a Waters 600 pump and WISP 712 auto-sampler. The post-column reagent (1.2 M KOH in 90% methanol) was introduced using a Waters reagent delivery module and the mixture passed through a 1-ml reaction coil (Waters) kept at 69°C. Detection was at 290 nm using a Waters 484 Tunable Absorbance Detector, which produced a linear response over the range of the standard curve (20–1,000 ng/ml). Quality control samples of 15, 75 and 150 ng/ml for artesunate and 75, 450 and 750 ng/ml for DHA were included in each run. Within- and between-day coefficients of variation were below 14%. The lower limit of quantification was 24 ng/ml for both artesunate and dihydroartemisinin.
Amodiaquine and desethylamodiaquine were analysed by LC mass spectrometry using an Agilent 1100 Series LC/MS system. Protein was precipitated from plasma samples (200 ul) using three volumes of acetonitrile. Supernatant (5 μl) was injected onto the HPLC. Chromatography was carried out using a 50 × 4.6 mm C18 Xterra column (Waters). The mobile phase comprised 75% acetonitrile, 0.02 M ammonia, pH 10.2. The extracted ion for amodiaquine was m/z 356 and for desethylamodiaquine m/z 328. The calibration curve for amodiaquine was linear in the range 5–100 ng/ml and for desethylamodiaquine in the range 5–400 ng/ml. Quality control samples of 25, 75 and 250 ng/ml were used for desethylamodiaquine and 2.5, 7.5 and 25 ng/ml for amodiaquine. Within- and between-day coefficients of variation were below 12%. The lower limit of quantification was 5 ng/ml for both amodiaquine and desethylamodiaquine.
Statistical analysis
Pharmacokinetic parameters were calculated from the artesunate, dihydroartemisinin, amodiaquine and desethylamodiaquine concentration profiles using WinNonLin, version 3.3 (Pharsight), with concentrations outside the specified limits of quantification regarded as missing values. Clearance (Cl) was calculated as 0.693 × Vd/T1/2 where Vd is the apparent volume of distribution and T1/2 is the elimination half-life. Because there was no intravenous comparator arm in this study, equivalent bioavailability was assumed for comparisons of apparent volume of distribution (Vd/f) and clearance (Cl/f), where f is the oral bioavailability or fraction of the drug absorbed (unknown).
All four compounds were first analysed separately. Because both artesunate and dihydroartemisinin are highly parasiticidal in malaria patients, the pharmacokinetic parameters associated with therapeutic response [area under the plasma concentration time curve (AUC) and maximum clearance (Cmax)] are also reported together as dihydroartemisinin equivalents, defined as the sum of the measured dihydroartemisinin concentrations plus the artesunate concentration converted to dihydroartemisinin equivalents (using molecular weights of 384 and 284 for artesunate and dihydroartemisinin respectively) [16, 17]. As amodiaquine undergoes a rapid and extensive conversion to its active metabolite, desethylamodiaquine was considered the primary analyte [9, 10, 18].
The pharmacokinetic parameters following administration of artesunate and amodiaquine alone and in combination were compared using Stata, version 9.0 [Stata, College Station, TX, USA]. Data were log-transformed and then compared using the analysis of variance (ANOVA) for a cross-over design to take into account the repeated measures by study subject, treatment period and treatment groups and, for amodiaquine and desethylamodiaquine, a sequence effect. The treatment effects generated from the ANOVA were exponentiated in order to express comparisons between monotherapy and combination therapy as a ratio. Any apparent discrepancies between the difference in the group means and these ratios are due to the fact that the ratios are based on the within-patient differences in log-transformed values and not the group arithmetic means. Given the multiple testing, statistical significance of results should be interpreted with caution.
For the safety analysis, means and 95% confidence intervals (95% CI) for each haematological parameter (haemoglobin, haematocrit, platelets, white cell count, absolute lymphocyte and neutrophil count) were calculated at baseline and at the end of each treatment phase. Changes in these values from baseline were determined using a mixed effect regression model that took into account repeated measures within-patient and were adjusted for the period and period-treatment interaction effects.
Results
Subject demographics
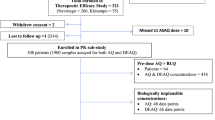
Nineteen volunteers were screened; two were excluded because of neutropaenia and two withdrew consent. Fifteen healthy normal volunteers (10 male, 5 female) entered the study with a mean age, weight and height of 24.4 years, 67.3 kg and 171 cm, respectively. The mean dose of amodiaquine was 10.72 mg/kg and that of artesunate was 4.26 mg/kg. Safety analysis included all 15 volunteers; only data from the 13 volunteers who completed the study were included in the pharmacokinetic analyses. A female volunteer was withdrawn due to a new prescription of fluoxetine for depression, as this drug could potentially interact with artesunate and amodiaquine by inhibiting cytochrome P450 enzymes. One male volunteer was withdrawn due to a possible hypersensitivity reaction on his first exposure to amodiaquine.
Pharmacokinetic parameters
Effect of amodiaquine on artesunate pharmacokinetic parameters
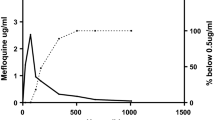
Data were analysed using a non-compartmental model. Figure 1a shows the mean plasma concentration time curves of artesunate and dihydroartemisinin following administration of artesunate alone and artesunate plus amodiaquine. The AUC, Cmax and time to Cmax (Tmax) of artesunate were similar following monotherapy and combination therapy (Table 1). Figure 2a illustrates the impact of adding amodiaquine on the dihydroartemisinin AUC. Following the combination therapy, dihydroartemisinin AUC was lower [ratio 67% (95% CI 51–88%); P = 0.008], Cmax was lower [ratio 51% (95% CI 33–78%); P = 0.005], T1/2 was longer [ratio 157% (95% CI 115–213%); P = 0.008] and Vd was larger [ratio 192% (95% CI 133–275%); P = 0.003], when compared with artesunate monotherapy (Table 1). These ratios have been adjusted for repeated measures by subject and period effects. As a measure of the total exposure to artemisinin derivatives, the Cmax and AUC of the combined DHA-equivalents were also analysed and found to be lower following combination therapy [Cmax ratio 51% (95% CI 32–84%), P = 0.011; AUC ratio 72% (95% CI 54–95%), P = 0.023] when compared with monotherapy. Cl and Tmax of dihydroartemisinin were similar when monotherapy and combination therapy were administered (Table 1).
Effect of artesunate on amodiaquine pharmacokinetic parameters
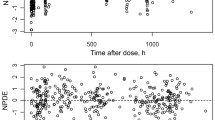
Amodiaquine samples for one volunteer were missing. Figure 1b shows the mean plasma concentrations of desethylamodiaquine over time following administration of amodiaquine alone and in combination. Figure 2b illustrates the impact of artesunate on the desethylamodiaquine AUC. The volunteer (subject A) who had the highest observed AUC for desethylamodiaquine following combination therapy [29,504 ng·h/ml compared with the mean of 8,437 (95% CI 5,744–11,131) ng·h/ml] was excluded from the pharmacokinetic analyses of desethylamodiaquine, as this was an extreme outlier and influential observation (Fig. 2b; Fig. 3).
The impact of adding artesunate to amodiaquine on the pharmacokinetic parameters of amodiaquine and desethylamodiaquine is reported for the remaining 11 volunteers. The pharmacokinetic parameters of amodiaquine were similar when administered as monotherapy or in combination with artesunate (Table 2). The desethylamodiaquine AUC is lower [ratio 65% (95% CI 46–90%); P = 0.015], Tmax shorter [ratio 60% (95% CI 45–80%); P = 0.003] and clearance more rapid [ratio 164% (95% CI 112–243%); P = 0.016] when amodiaquine was administered in combination with artesunate rather than as monotherapy (Table 2). There was a trend towards a lower day 7 concentration of desethylamodiaquine [ratio 56% (95% CI 30–104%); P = 0.064] when amodiaquine was administered in combination (Fig. 3). These ratios have been adjusted for repeated measures by subject, period and sequence effects. The Vd and Cmax were not significantly different when monotherapy and combination therapy were administered.
Safety
Twenty-nine adverse events were reported over the course of the study by 10 (67%) of the 15 volunteers. The frequency of adverse events was similar across all three treatment arms (P > 0.10): 4/15 (27%) following artesunate alone, 8/15 (53%) following amodiaquine alone, and 5/15 (33%) following the combination. All adverse events were consistent with the product information available, resolved spontaneously and, except for the transaminitis (see below) were mild or moderate in intensity.
A case of asymptomatic, prolonged, severe transaminitis (NCI grade 3, AST 5–20× upper limit of normal) that developed after phase 3 of the study has been previously published [7]. This was considered to be probably related to amodiaquine, rather than artesunate, before the pharmacokinetic results were available. The subsequent finding that this volunteer had the highest measured desethylamodiaquine AUC following the administration of artesunate plus amodiaquine [29,504 ng·h/ml compared with the combination therapy mean of 8,437 (95% CI 5,744–11,131) ng·h/ml] strengthened this assessment. There were no liver function abnormalities detected in any other volunteers. No renal or electrolyte abnormalities were detected in any volunteers.
Significant haematological changes were confined to the white cell counts. During phase 2 of the study, two volunteers (one following amodiaquine alone, one following the combination) developed asymptomatic, NCI grade 1 leucopaenia (3 to <4 × 109/L) and either a grade 1 (1.5 to <2 ×109/L) or grade 2 (1 to <1.5 × 109/L) neutropaenia. None of the other observed changes in haematological parameters were outside the normal range.
There were no significant changes following treatment seen on the ECGs; the mean (95% CI) QTc interval was 398 (390–406) ms at screening, 401 (393–409) ms following artesunate alone, 400 (385–414) ms following amodiaquine alone and 412 (400–424) ms following the combination. In two patients, the prolongation following treatment with amodiaquine or artesunate plus amodiaquine was considered of borderline clinical significance.
Discussion
The pharmacokinetic analyses in this randomised, cross-over study showed statistically significant pharmacokinetic interactions resulting in reductions in the AUC of both dihydroartemisinin and desethylamodiaquine when artesunate and amodiaquine were given in combination to healthy volunteers. Of further concern is that one healthy volunteer failed to reach quantifiable concentration of both artesunate and dihydroartemisinin throughout the initial 12 h. There is insufficient evidence currently available to explain the basis of these interactions.
The clinical significance of our findings is unclear because we studied healthy volunteers. In one study comparing pharmacokinetic parameters of dihydroartemisinin in patients and volunteers, patients had a significantly higher Cmax (1,948 vs. 1,192 nmol/l) and AUC0–12 (4,024 vs. 1,763 nmol·h/l), while their Vd and Cl were both lower. The Tmax and terminal elimination half-life of the patients were similar to those of the volunteers [19]. Desethylamodiaquine pharmacokinetic parameters in malaria-infected adults in Africa [20] and children with acute malaria in Papua New Guinea [21] were similar to those of normal volunteers.
In artemisinin-based combination therapy, the artemisinin is given to kill most of the parasites quickly, while the longer-acting partner drug (e.g. amodiaquine) is given to kill the residual parasites. For an antimalarial with a long elimination half-life like desethylamodiaquine, the key pharmacokinetic parameter for parasite killing is the AUC, which is a useful predictor of therapeutic response as it captures both the drug concentration and the duration of exposure [22, 23]. For such drugs the antimalarial concentration on day 7 is strongly correlated with AUC, and thus treatment response [23]. An association of desethylamodiaquine concentration on day 7 and amodiaquine treatment response has been found in children with uncomplicated falciparum malaria [18]. In our study, the AUC (and probably the day 7 desethylamodiaquine concentration) was reduced following the artemisinin-based combination; this may result in reduced parasite killing, particularly in areas where there is reduced amodiaquine sensitivity. Although there is a linear relationship between amodiaquine dose and the desethylamodiaquine AUC [24], the wide inter-individual variability in desethylamodiaquine levels (five-fold in our study), and the consequent potential for drug-induced toxicity, could preclude increasing the amodiaquine dose to compensate for the lower desethylamodiaquine AUC observed following co-administration with artesunate.
Extensive clinical trial data show that artesunate plus amodiaquine is more effective (at clearing parasitaemia and preventing recrudescence) than amodiaquine alone [1, 6]. Therefore, if reductions in the Cmax and AUC of desethylamodiaquine and dihydroartemisinin occur in patients, the negative effect on parasite killing may become clinically insignificant due to the additive (or possibly synergistic) parasiticidal effects of the combination. However, this may only apply to areas where the level of amodiaquine resistance is low. Although clinically significant resistance to the artemisinins has not yet been documented, amodiaquine resistance is well documented and this is probably the principal explanation for low artesunate plus amodiaquine cure rates observed in a number of African countries [1, 6].
Despite our small sample size, we detected the well-known amodiaquine-related adverse drug reactions. Clinically important adverse events were reported by a quarter of these volunteers, even though all were healthy and only two doses were administered 3 weeks apart (rather than the daily administration for 3 days recommended for malaria treatment). When the artesunate plus amodiaquine combination becomes widely used, monitoring of liver function tests and haematological parameters are warranted to define these risks in malaria patients, particularly in patients at special risk such as those at the extremes of age, with HIV co-infection or malnutrition [1]. However, the feasibility of this recommendation outside of the research setting is of concern.
To conclude, the total exposure to the main active metabolites of both artesunate and amodiaquine was significantly reduced when administered in combination to healthy African volunteers; this might be important clinically. However, because cure rates with this combination are generally higher than with amodiaquine monotherapy, artesunate and amodiaquine could remain in the armamentarium of drugs used to combat falciparum malaria, provided efficacy continues to be monitored and adequate safety precautions can be taken. Further pharmacokinetic research on artesunate plus amodiaquine, when administered concurrently or as a fixed dose combination, is urgently required in patients with malaria to establish the extent and clinical significance of these pharmacokinetic interactions.
References
World Health Organisation (2006) WHO guidelines for the treatment of malaria. http://www.who.int/malaria/docs/TreatmentGuidelines2006.pdf
World Health Organisation (2006) Facts on ACTs (artemisinin-based combinations). http://www.rollbackmalaria.org/cmc_upload/0/000/015/364/RBMInfosheet_9.pdf
Hatton CS, Peto TE, Bunch C, Pasvol G, Russell SJ, Singer CR et al (1986) Frequency of severe neutropenia associated with amodiaquine prophylaxis against malaria. Lancet 1(8478):411–414
Larrey D, Castot A, Pessayre D, Merigot P, Machayekhy JP, Feldmann G et al (1986) Amodiaquine-induced hepatitis. A report of seven cases. Ann Intern Med 104(6):801–803
Neftel KA, Woodtly W, Schmid M, Frick PG, Fehr J (1986) Amodiaquine induced agranulocytosis and liver damage. Br Med J (Clin Res Ed) 292(6522):721–723
Adjuik M, Agnamey P, Babiker A, Borrmann S, Brasseur P, Cisse M et al (2002) Amodiaquine-artesunate versus amodiaquine for uncomplicated Plasmodium falciparum malaria in African children: a randomised, multicentre trial. Lancet 359(9315):1365–1372
Orrell C, Taylor WR, Olliaro P (2001) Acute asymptomatic hepatitis in a healthy normal volunteer exposed to 2 oral doses of amodiaquine and artesunate. Trans R Soc Trop Med Hyg 95(5):517–518
German P, Greenhouse B, Coates C, Dorsey G, Rosenthal P, Charlebois E et al (2007) Hepatotoxicity due to a drug interaction between amodiaquine plus artesunate and efavirenz. Clin Inf Dis 44:889–891
Winstanley PA, Edwards G, Orme M, Breckinridge AM (1987) The disposition of amodiaquine in man after oral administration. Br J Clin Pharmacol 23:1–7
Krishna S, White NJ (1996) Pharmacokinetics of quinine, chloroquine and amodiaquine. Clinical implications. Clin Pharmacokinetics 30(4):263–299
Benakis A, Paris M, Loutan L, Plessas CT, Plessas ST (1997) Pharmacokinetics of artemisinin and artesunate after oral administration in healthy volunteers. Am J Trop Med Hyg 56:17–23
Newton P, Suputtamongkol Y, Teja-Isavadharm P, Pukrittayakamee S, Navaratnam V, Bates I, White N (2000) Antimalarial bioavailability and disposition of artesunate in acute falciparum malaria. Antimicrob Agents Chemother 44(4):972–977
Edwards IR, Biriell C (1994) Harmonization in pharmacovigilance. Drug Safety 10(2):93–102
NIH (1999) Common toxicity criteria, version 2.0. http://ctep.cancer.gov/forms/CTCv20_4-30-992.pdf
Batty KT, Davis TME, Thus LTA, Binh TQ, Anh TK, Ilett KF (1996) Selective high-performance liquid chromatographic determination of artesunate and alpha and beta-dihydroartemisinin in patients with falciparum malaria. J Chromatogr 677:345–350
Karbwang J, Na-Bangchang K, Thanavibul A, Molunto P (1998) Plasma concentrations of artemether and its major plasma metabolite, dihydroartemsinin, following a 5-day regimen of oral artemether, in patients with uncomplicated falciparum malaria. Ann Trop Med Parasitol 92(1):31–36
Silamut K, Newton PN, Teja-Isavadharm P, Suputtamongkol Y, Siriyanonda D, Rasameesoraj M, Pukrittayakamee S, White NJ (2003) Artemether bioavailability after oral or intramuscular administration in uncomplicated falciparum malaria. Antimicrob Agents Chemother 47(12):3795–3798
Hietala SF, Bhattarai A, Msellem M, Roshammar D, Ali AS, Stromberg J, Hombhanje FW, Kaneko A, Bjorkman A, Ashton M (2007) Population pharmacokinetics of amodiaquine and desethylamodiaquine in pediatric patients with uncomplicated falciparum malaria. J Pharmacokinet Pharmacodyn 34(5):669–686
Teja-Isavadharm P, Watt G, Eamsila C, Jongsakul K, Li Q, Keeratithakul G et al (2001) Comparative pharmacokinetics and effect kinetics of orally administered artesunate in healthy volunteers and patients with uncomplicated falciparum malaria. Am J Trop Med Hyg 65(6):717–721
Winstanley PA, Simooya O, Kofi-Ekue JM, Walker O, Salako LA, Edwards G et al (1990) The disposition of amodiaquine in Zambians and Nigerians with malaria. Br J Clin Pharmacol 29(6):695–701
Hombhanje FW, Hwaihwanje I, Tsukahara T, Saruwatari J, Nakagawa M, Osawa H et al (2005) The disposition of oral amodiaquine in Papua New Guinean children with falciparum malaria. Br J Clin Pharmacol 59(3):298–301
White NJ (2002) The assessment of antimalarial drug efficacy. Trends Parasitol 18(10):458–464
Barnes KI, Watkins WM, White NJ (2008) Antimalarial dosing regimens and drug resistance. Trends Parasitol 24(3):127–134
Winstanley PA, Edwards G, Orme ML, Breckenridge AM (1987) Effect of dose size on amodiaquine pharmacokinetics after oral administration. Eur J Clin Pharmacol 33(3):331–333
Acknowledgements
The authors gratefully acknowledge the contributions of Jennifer Norman, Gary Gabriels and Quinton Fivelman for assisting in data collection, and of Alicia Evans for performing the drug assays. This study was funded by the UNICEF/UNDP/WB/WHO Special Programme for Research and Training in Tropical Diseases (TDR).
Disclaimer
The authors declare no conflict of interest. Piero Olliaro is a staff member of the World Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy or views of the World Health Organization.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Orrell, C., Little, F., Smith, P. et al. Pharmacokinetics and tolerability of artesunate and amodiaquine alone and in combination in healthy volunteers. Eur J Clin Pharmacol 64, 683–690 (2008). https://doi.org/10.1007/s00228-007-0452-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0452-8