Abstract
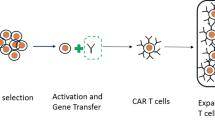
Chimeric antigen receptor T-cell (CAR-T) therapy is a revolutionary cancer treatment modality where a patient’s own T cells are collected and engineered ex vivo to express a chimeric antigen receptor (CAR). These reprogrammed CAR-T cells, when reinfused into the same patient, stimulate a T-cell mediated immune response against the antigen-expressing malignant cells leading to cell death. The initial results from pivotal clinical trials of CAR-T agents have been promising, leading to multiple approvals in various hematologic malignancies in the relapsed setting, including acute lymphoblastic leukemia (ALL), diffuse large B-cell lymphoma (DLBCL), mantle cell lymphoma, follicular lymphoma, and, more recently, multiple myeloma. However, since the initial trials and US Food and Drug Administration approvals, there have been significant barriers to the widespread use of this therapy. The barriers to the use of CAR-T therapy include complex logistics, manufacturing limitations, toxicity concerns, and financial burden. This review discusses potential solutions to overcome these barriers in order to make this life-changing therapy widely accessible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
CAR-T cell therapy has shown promising results in multiple clinical trials, though there are significant barriers to its widespread use. |
Such barriers include complex logistics, concerns over toxicity, and financial burden. |
Despite the barriers and challenges, the positive outcomes seen as a result of CAR-T therapy outweigh the barriers and justify its continued use and development. |
1 Introduction
In 2017, the US Food and Drug Administration (FDA) approved the first chimeric antigen receptor T-cell (CAR-T)-mediated therapies for relapsed/refractory (r/r) diffuse large B-cell lymphoma (DLBCL) and r/r acute lymphoblastic leukemia (ALL) [1, 2]. This novel concept, where a patient’s own T-cells are engineered to attack their cancer, seemed to signal a new frontier in oncology. Since then, CAR-T therapy has been approved for use in additional hematological malignancies, including follicular and mantle cell lymphomas as well as multiple myeloma. Additionally, hundreds of clinical trials are currently being conducted using CAR-T therapies in various other solid tumor malignancies, such as glioma, sarcomas, and pancreatic cancer [3].
Despite the many FDA approvals and promising clinical data being produced, CAR-T therapy is not an option for every patient. Several barriers exist that keep CAR-T from widespread use. These barriers can be grouped into three broad categories: challenges associated with the CAR-T product itself, concerns regarding clinical outcomes, and questions regarding the cost-benefit analysis of this expensive therapy (Table 1). These realities force us to consider the question: is it possible and worthwhile to overcome the many barriers that may prevent the widespread use of this treatment?
2 Product-Related Barriers
2.1 Patient Eligibility
Despite the impressive responses to CAR-T therapy, one of the first barriers to utilization is patient eligibility. It is well documented that clinical trials have strict inclusion criteria and the patient population that is studied is not always representative of real-world patients [4].
Over the last few years, multiple studies in lymphoma and leukemia have examined real-world evidence (RWE) to determine if CAR-T therapy is effective in a broader range of patients. In these studies, the average ages were older compared to the clinical trials, and patients had other diseases (e.g., HIV and hepatitis), which would have excluded them from the original studies [5, 6]. Despite higher co-morbidities, these patients had similar outcomes to those included in the initial clinical trials [5,6,7]. These RWE studies provide an important insight into the feasibility of using CAR-T therapy for a wider array of patients and could help CAR-T therapy centers select patients who might have been excluded in clinical trials.
2.2 Treatment Centers and Current Delivery Model
Another potential barrier to CAR-T therapy is the current paradigm for how this therapy is delivered. Traditionally, CAR-T therapy has been given in an inpatient setting, usually at a large academic medical center [8, 9]. This creates two barriers: one being the issue of a patient’s geographical proximity to treatment, the other being the costs associated with inpatient therapy. If CAR-T therapy is only to be delivered at large, academic medical centers, there is a barrier to referral if patients do not live near one of these institutions [10]. A potential solution to this issue, and one that is receiving growing attention, is the possibility of delivering CAR-T therapy in community-based oncology clinics and hospitals. This would require additional training and resources for these centers to be approved to administer CAR-T therapy but would significantly increase patient access.
Somewhat hand in hand with moving CAR-T therapy to the community setting is the idea of providing CAR-T therapy as an outpatient procedure. This could be done in community oncology practices and could reduce costs associated with inpatient stays. Patients still need to reside within 30–60 min of the treatment center for weeks after treatment so that they can be monitored for adverse effects immediately following CAR-T administration. Trial data have shown that a significant fraction of patients treated in the outpatient setting require subsequent hospitalization, often related to life-threatening side effects, including cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS) [8, 9]. Although the feasibility of outpatient delivery has been demonstrated in several trials [1, 11, 12], this may be driven by patient characteristics that need to be considered in deciding the setting for care delivery. Thus, an assessment of the patient’s risk of these side effects, time to onset of CRS and ICANS, and the extent to which the patient has access to trained providers and caregivers are needed to determine whether the outpatient setting is appropriate. To mitigate risks, outpatient centers will need to have detailed safety protocols in place and ample resources to treat patients with CRS and ICANS; that includes not only physical resources (e.g., hospital access and medication), but also proper training of clinical staff [13, 14].
Currently, there is not a robust model or system for delivering CAR-T therapy as an outpatient procedure, but as the field continues to evolve, this may become a reality. Through changes to the therapy itself (e.g., fewer side effects from newer therapies), and better identification of patients suited for outpatient therapy (e.g., discussion of patient cases during tumor-boards), the outpatient model could be implemented in the future.
2.3 Slow Prior Authorization Process
Another barrier to treatment, though not unique to CAR-T therapy, is prior authorization from insurance providers. The process of receiving prior authorization can be very time-consuming, which is a particularly salient issue for patients referred for CAR-T therapy. These patients are often required to have r/r disease and must have previously failed other forms of treatment. In other words, these patients tend to be very sick and need care quickly. Previous studies have shown that, frequently, patients do not receive prior authorization in a timely enough manner and the clinical team will either refer patients to another type of therapy or patients may succumb to the disease while waiting on prior authorization. Various solutions can be considered to speed along prior authorization, such as having a streamlined process that is uniformly adaptable amongst various CAR-T products, creating a pre-approval process that is standardized amongst various insurance companies, and employing the assistance of third-party companies [15].
2.4 Complex Manufacturing
An additional pressing issue is that of lengthy “vein-to-vein” time, referring to the gap of time between leukapheresis and CAR-T administration. This process can take several weeks, and by the time the CAR-T cells are ready, patients may become ineligible due to disease progression or worsening organ function [16]. The process of engineering CAR-T cells for individual patients is laborious. Manufacturing is typically only done at a select number of sites, so cells must be collected and shipped to these manufacturing sites for T-cell engineering. After CAR-T manufacturing, the cells have to undergo rigorous quality and safety checks, making the vein-to-vein time longer. One way to diminish this barrier is the creation of allogeneic, as opposed to autologous, CAR-T cells. Allogeneic therapy is not without its own challenges (e.g., graft vs. host disease), but it could eventually lead to banks of preserved CAR-T cells at individual hospitals that could be given to patients on a much shorter timeline [17].
Another approach to reducing vein-to-vein time, reducing production cost, and increasing scalability of a decentralized CAR-T production model has been explored. This can be achieved by producing CAR-T products in academic hospitals, using GMP grade facilities, or automated CAR-T manufacturing using devices like the Miltenyi Prodigy system or the Lonza Cocoon incubator. In countries like Switzerland with a more permissive regulatory environment, hospitals are manufacturing CAR T cell therapies at US$150,000–US$200,000, approximately half the price of most approved CAR-T cell therapies in the USA. However, in the USA, CAR-T cell therapies irrespective of the site of production (e.g., academic vs. industry) must undergo the same regulatory and pre-market approval as drugs, limiting its widespread application.
3 Clinical Outcomes
The initial data with CAR-T therapy in clinical trials showed striking efficacy in patients with r/r DLBCL or ALL who did not respond to other forms of treatment [1, 2, 18, 19]. The outcome of CAR-T therapy was supposed to be remission for the vast majority of patients. However, these initial data have been somewhat clouded by potentially serious side effects associated with CAR-T therapy, as well as the tendency for the disease to relapse after their initial response to treatment. While some patients will have a complete response and disease will enter remission after CAR-T therapy, others will experience significant adverse events or disease relapse. Do these possibilities, that there may be life-threatening side effects or even just the return of the disease, discredit the successful outcomes seen with CAR-T therapy?
3.1 Therapy-Related Toxicities
To answer this question, we first must discuss and understand the most common side effect associated with CAR-T therapy, which is CRS. CRS occurs in almost all patients who receive a CAR-T infusion and can be relatively mild to life-threateningly severe [20,21,22]. Patients will typically develop a fever and can also develop hypotension, tachycardia, and organ failure; the most severe forms of CRS can result in death [21]. However, physicians are becoming more and more familiar with identifying CRS and treating it before it reaches a level where it can be fatal. Additionally, physicians are beginning to identify which patients are most likely to have severe CRS or other side effects [23]. There are several strategies to combat CRS when it does occur, such as the interleukin 6 (IL-6) receptor inhibitor tocilizumab and corticosteroids [24]. Other common CAR-T therapy side effects include ICANS and tumor lysis syndrome (TLS). IL-6 inhibitors, corticosteroids, and anticonvulsant therapy can aid in treating ICANS [24]. TLS is managed with standard supportive care [25]. In addition to these strategies that are currently used to manage CAR-T toxicities, there is also the possibility of modifying the chimeric antigen receptors (CARs) to eliminate these toxicities. This includes tactics such as modifying CARs to contain a safety switch to turn off CAR-T cell activity or using human-derived antibody fragments for CARs (as opposed to mouse) to decrease immune activation [26, 27].
3.2 Patient Survival and Relapse
Along with the issue of severe toxicities associated with CAR-T therapy, disease relapse must also be taken into consideration when assessing the costs and benefits. The initial CAR-T trials showed amazing results, particularly when considering how sick the patients were and the fact that they had failed and relapsed with multiple other treatment modalities (Table 2). However, as CAR-T therapies continue to be used, it is becoming clear that long-term remission is not achieved for every patient. The 5-year progression-free survival rate was recently reported as 31% for patients with DLBCL and 43% for patients with follicular lymphoma who received tisa-cel [28]. Further, the 4-year overall survival rate for patients with DLBCL who received axi-cel was reported as 44% [29]. While these numbers are certainly impressive, it leaves a large portion of patients who experience the return of their disease. A study that examined multiple ALL clinical trials using CAR-T therapy determined that anywhere from 30 to 60% of patients will experience disease relapse after therapy, often within months of the treatment [30]. Similarly, a study conducted on patients receiving CAR-T therapy for DLBCL demonstrated that approximately 50% of patients experienced disease relapse, and relapse occurred on average 30.5 days post-infusion [31].
Relapse in CAR-T-treated patients can either be due to CD19-positive (CD19+) or CD19-negative (CD19-) diesase, referring to the status of the CD19 antigen on the B-cell surface. When patients relapse but are CD19+, this is likely due to a failure of the CAR-T cells to persist in the patient. Initial studies had shown that the costimulatory domain of CARs can contribute to their persistence in the patient, particularly that the 4-1BB costimulatory domain (used in tisa-cel and liso-cel) allows CAR-T cells to persist longer [32]. However the hypothetical benefit of persistence of CAR based on the costimulatory domain was challenged by the excellent long-term survival in patients receiving the axi-cel compound with CD28 as the costimulatory domain. It is also possible for patients to have a CD19- relapse, where the cancerous cells acquire a frameshift mutation or a deletion in the CD19 gene so that the cells can evade detection by CAR-T cells [30]. For the patients experiencing CD19+ relapse, multiple factors are likely at interplay including the health of T cells, murine scFv, type of viral vector on top of CAR-T persistence. Research continues to be conducted to understand which patients are most likely to experience disease relapse, as well as how to engineer CAR-T therapies to avoid relapse and achieve long-term remission in the largest number of patients.
3.3 Post-CAR-T Healthcare Utilization
A final point of consideration regarding patient outcomes is the additional healthcare utilization (HCU) after treatment and therefore the cost of this care. Considering the potential side effects and the fact that not all patients will stay in remission after CAR-T therapy, many patients will need care in addition to the CAR-T treatment itself. A retrospective study examining post-CAR-T HCU in patients with lymphoma found that 28.1% of patients were admitted to the hospital at least once within 3 months of receiving CAR-T therapy, and 15.5% of patients had at least one intensive-care admission within 3 months of receiving therapy [39]. Another study examined HCU pre- and post-CAR-T administration in DLBCL patients and found that there were fewer ambulatory and emergency department visits in the months following CAR-T as compared to the months before; although patients are returning to the hospital, HCU-related costs were significantly lower after treatment [40].
Multiple studies have demonstrated that the most significant costs post-CAR-T are incurred when patients develop severe CRS or neurological events (grade ≥ 3 CRS) [41, 42]. Despite this, an analysis of Medicare claims suggests that the cost of treatment in the 6 months following CAR-T infusion is significantly lower (39%) than in the 6 months preceding treatment [43]. It is somewhat unsurprising that patients require additional HCU after CAR-T therapy, as they likely would with any treatment (e.g., autologous stem cell transplant). While it is difficult to directly compare the post-treatment HCU costs of CAR-T with another therapy, the good news relative to CAR-T is that the cost of treating patients does tend to be much lower after CAR-T therapy. Additionally, if newer generations of CAR-T agents have a more favorable toxicity profile, reducing the cost burden of managing acute adverse events, it may be even more economically advantageous to utilize CAR-T therapy.
4 Cost-Benefit Analysis
When performing financial cost-benefit analyses in healthcare, the cost of therapy and the additional quality-adjusted life years (QALYs) gained are both taken into account. Ideally, these costs and benefits should be compared to counterfactual treatment that the patient would receive in the absence of CAR-T therapy. In the USA, a cost per QALY of US$100,000–US$150,000 has been considered the threshold for whether a therapy is cost-effective [35]. Since the approval of CAR-T therapies, several studies have examined their value based on these metrics. Of the three studies that examined tisa-cel for the treatment of pediatric B-ALL, each determined that the cost per QALY was less than US$100,000; however, the cost per QALY depends on the assumptions for longer-term survival (i.e., > 5 years) [44,45,46]. In a study that focused on adult patients receiving tisa-cel for the treatment of DLBCL, the cost per QALY ranged from US$168,00 to US$337,000, again depending on the longer-term assumptions [47]. The cost per QALY for axi-cel in DLBCL was higher and varied across studies and assumptions, ranging from US$58,146 [48] to US$230,900 [49] per QALY gained. It is also important to note that these studies include not only the cost of therapy itself, but short-term and long-term monitoring of patients and treatment of side effects.
With these initial data in mind, it seems that CAR-T therapy usage could certainly be justified, though there are many caveats to these findings. On one hand, CAR-T therapy has not been in use long enough to fully know the frequency of late relapse, long-term adverse effects leading to additional costs of care later in a patient’s life, and how many patients will experience long-term remission of their disease. On the other hand, these numbers do not consider the contributions that a CAR-T recipient may make to society and the economy if they were to have a long remission as a result of therapy. Another point of consideration is that CAR-T has often been used for patients with relapsed/refractory disease. Patients are typically later in their cancer treatment journey when they receive CAR-T therapy, which could contribute to lower survival rates. If CAR-T therapy were used earlier, survival benefits might potentially increase, simultaneously adjusting the QALY to show even stronger justification for the use of CAR-T. Early data from studies utilizing CAR-T in first relapse show promising efficacy results when compared to standard of care, largely autologous stem cell transplant [50, 51]. Similarly, improved communication between the referring physician and CAR-T centers is critical for successful therapy, as it could lessen the time between referral and treatment delivery. Timing is of the utmost importance when it comes to success in CAR-T therapy, as patients often become too sick or succumb to the disease by the time they can actually receive treatment. Improved and streamlined communication could greatly improve the speed at which patients receive therapy, ultimately leading to better treatment outcomes. By continuing to improve CAR-T therapy manufacturing, access, and timing of therapy, ideally the success rate of therapy will increase, and the costs associated with CAR-T toxicities may also decrease. Both scenarios would help tilt the scales in favor of CAR-T, providing enough benefit to justify its cost.
A final point to consider is the rapidly evolving CAR therapy landscape. First, there is a growing interest in multiple CAR-T cell infusions. While the data are nascent on this topic, providing multiple infusions would certainly drive up the cost of CAR-T therapy, though it could improve survival to a degree that still makes this therapy cost-effective. Additionally, there are countless trials that are currently exploring the use of allogeneic CAR-T therapy, CAR-natural killer (CAR-NK) cell therapy, and CAR-T therapy with various new targets. Though the data are immature on these new therapies at the moment, it stands to reason that the potential for off-the-shelf therapy, or possibly more effective autologous therapy, could both provide improved survival outcomes for patients, which would ultimately impact the cost-benefit analysis as well.
It is also relevant in this conversation to discuss the cost of similarly targeted drugs, such as blinatumomab and tafasitamab. Both of these drugs capitalize on some of the same principles of CAR-T therapy, but differ in a few key ways. Blinatumomab is a bi-specific T-cell engager (BiTE) therapy that does not require personalized treatment for each patient as it recognizes conserved sites on T cells (CD3) and B cells (CD19) and is approved for use in ALL [52]. Tafasitamab is a monoclonal antibody to the CD19 antigen on B cells, approved for use in patients with relapsed DLBCL [53]. When these two agents were initially approved, their price tags seemed incredibly high, in the range of US$100,000 per year [52, 54]. While it is difficult to directly compare these agents, given the different approved indications and variability in patient populations, none of these can exactly be considered conventionally affordable therapies. Blinatumomab and tafasitamab may seem cheaper, but theoretically require more doses than a single CAR-T infusion, making it unclear if they really are any more affordable. With all of this in mind, it is abundantly clear that treating these malignancies does not come cheap, though most studies would suggest that the cost does justify the benefits.
5 Reimbursement Challenges
Reimbursement challenges have been at the center of discussion since the FDA approval of CAR-T therapy. The Centers for Medicare and Medicaid Services (CMS) reimbursement plan has two main components: (1) Medicare Severity-Diagnosis Related Group (MS-DRG) and (2) New Technology Add-On Payments (NTAP)—class of reimbursement to help pay for new technology that is not included in the MS-DRG payment [55]. A non-specific MS-DRG (MS-DRG 016) was first introduced in October 2017 and included a payment between US$6000 and US$16,000. Since then, MS-DRG has continued to be evaluated with the MS-DRG 016 used between 1 October 2018, and 30 September 2020, to pay US$43,094. On 1 October 2020, MS-DRG 018 was introduced, which provided a base payment rate of US$239,929. It is anticipated that in 2022, the MS-DRG 018 will increase by approximately US$7025, for a total of US$246,958.
Over the last 5 years, we have seen a constant change with slow but steady improvements in the overall reimbursement for CAR-T therapy. However, as suggested by key national organizations like the American Society of Clinical Oncology, these reimbursements still fall short, especially with the minimum estimated cost of CAR-T therapy and related services at US$419,238 [56, 57].
Alternative payment models are being continually explored, with two main strategies. One strategy recommends a bundled payment (or global payment) that includes packaging all costs of care in a one-time payment. The second is a completely opposite strategy, referred to as an outcome-based agreement (OBA) or value-based payment. Novartis was the first to introduce OBA for pediatric induction for Kymriah. In this model, the hospital does not receive an invoice for the CAR-T product if the patient fails to achieve a complete response by the 35th day after infusion. None of the payment models are without issues, and, therefore, both payers and providers will have to continue to be flexible in their utilization of specific models, especially given the evolving nature of cellular therapies [14].
6 Conclusion
In the short time since CAR-T therapies have been FDA approved, we have begun to understand the many barriers and considerations that come along with the wide-scale utility of this game-changing therapy; however, the challenges to using this potentially life-saving therapy are not insurmountable. Clinicians are becoming better at managing CAR-T-related toxicities, with newer CAR-T products appearing to have more favorable safety profiles. Additionally, though CAR-T is expensive, studies show that CAR-T therapy reduces post-treatment HCU and costs and provides an improvement in survival and quality of life, in comparison to the cost of care. Lastly, as with most cancer treatments, there is a possibility of relapse; however, there is a growing understanding of how relapse occurs, and which patients are most susceptible to relapse, which could likely lead to smarter drug design in the long term. Further, we may eventually see the greatest benefit from CAR-T by using it earlier in the course of disease. There is no denying the real concerns associated with CAR-T therapy, but as demonstrated here, there are many reasons to feel optimistic about its future.
References
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378(5):439–48.
Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377(26):2531–44.
Dana H, Chalbatani GM, Jalali SA, Mirzaei HR, Grupp SA, Suarez ER, et al. CAR-T cells: early successes in blood cancer and challenges in solid tumors. Acta Pharm Sin B. 2021;11(5):1129–47.
Gerber DE, Pruitt SL, Halm EA. Should criteria for inclusion in cancer clinical trials be expanded? J Comp Eff Res. 2015;4(4):289–91.
Kevin Tang LJN. Real-world experiences of CAR T-cell therapy for large B-cell lymphoma: how similar are they to the prospective studies? J Immunother Precis Oncol. 2021;4(3):150–9.
Kilgore KM, Mohammadi I, Schroeder A, Teigland C, Purdum A, Shah GL. Medicare patients receiving chimeric antigen receptor T-cell therapy for non-Hodgkin lymphoma: a first real-world look at patient characteristics, healthcare utilization, and costs. Blood. 2019;134(Supplement_1):793.
Jacobson C, Hunter B, Armand P, Kamihara Y, Ritz J, Rodig S, et al. Axicabtagene ciloleucel in the real world: outcomes and predictors of response, resistance and toxicity. Blood. 2018;132(Supplement_1):92.
Lyman GH, Nguyen A, Synder S. Economic evaluation of chimeric antigen receptor T-cell therapy by site of care among patients with relapsed or refractory large B-cell lymphoma. JAMA Netw Open. 2020;3(4): e202072.
Myers GD, Verneris MR, Goy A, Maziarz RT. Perspectives on outpatient administration of CAR-T cell therapy in aggressive B-cell lymphoma and acute lymphoblastic leukemia. J Immunother Cancer. 2021;9(4): e002056.
Dearment A. Outpatient use of CAR-Ts is enticing, but it comes with significant challenges too. 2020 June 3, 2020. https://medcitynews.com/2020/06/outpatient-use-of-car-ts-is-enticing-but-it-comes-with-significant-challenges-too/. Accessed 8 Mar 2022.
Bachier CR, Palomba ML, Abramson JS, Andreadis C, Sehgal AR, Godwin J, et al. Outpatient treatment with lisocabtagene maraleucel (liso-cel) in three ongoing clinical studies in relapsed/refractory (r/r) B cell non-Hodgkin lymphoma (NHL), including second-line transplant ineligible patients: transcend NHL 001, Outreach, and PILOT. Blood. 2019;134(Supplement_1):2868.
Schuster SJ, Bishop MR, Tam C, Borchmann P, Jaeger U, Waller EK, et al. Sustained disease control for adult patients with relapsed or refractory diffuse large B-cell lymphoma: an updated analysis of Juliet, a global pivotal phase 2 trial of tisagenlecleucel. Blood. 2018;132(Supplement 1):1684.
Jain T, Bar M, Kansagra AJ, Chong EA, Hashmi SK, Neelapu SS, et al. Use of chimeric antigen receptor T cell therapy in clinical practice for relapsed/refractory aggressive B cell non-hodgkin lymphoma: an expert panel opinion from the American society for transplantation and cellular therapy. Biol Blood Marrow Transplant. 2019;25(12):2305–21.
Kansagra AJ, Frey NV, Bar M, Laetsch TW, Carpenter PA, Savani BN, et al. Clinical utilization of chimeric antigen receptor T cells in B cell acute lymphoblastic leukemia: an expert opinion from the European society for blood and marrow transplantation and the American society for blood and marrow transplantation. Biol Blood Marrow Transplant. 2019;25(3):e76–85.
Caffrey M. Delays With Payers Mean Some Patients Miss Window for CAR T-Cell Therapy, Findings Show. 2021 April 26, 2021. https://www.ajmc.com/view/delays-with-payers-mean-some-patients-miss-window-for-car-t-cell-therapy-findings-show. Accessed 8 Mar 2022.
Nam S, Smith J, Yang G. Driving the Next Wave of Innovation in CAR T-cell Therapies. 2019 Dec. 13, 2019. https://www.mckinsey.com/industries/life-sciences/our-insights/driving-the-next-wave-of-innovation-in-car-t-cell-therapies. Accessed 8 Mar 2022.
Depil S, Duchateau P, Grupp SA, Mufti G, Poirot L. “Off-the-shelf” allogeneic CAR T cells: development and challenges. Nat Rev Drug Discov. 2020;19(3):185–99.
Munshi NC, Anderson LD Jr, Shah N, Madduri D, Berdeja J, Lonial S, et al. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N Engl J Med. 2021;384(8):705–16.
Berdeja JG, Madduri D, Usmani SZ, Jakubowiak A, Agha M, Cohen AD, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398(10297):314–24.
Sterner RC, Sterner RM. CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J. 2021;11(4):69.
Brudno JN, Kochenderfer JN. Toxicities of chimeric antigen receptor T cells: recognition and management. Blood. 2016;127(26):3321–30.
Brudno JN, Kochenderfer JN. Recent advances in CAR T-cell toxicity: mechanisms, manifestations and management. Blood Rev. 2019;34:45–55.
Faramand R, Jain M, Staedtke V, Kotani H, Bai R, Reid K, et al. Tumor microenvironment composition and severe cytokine release syndrome (CRS) influence toxicity in patients with large B-cell lymphoma treated with axicabtagene ciloleucel. Clin Cancer Res. 2020;26(18):4823–31.
Murthy H, Iqbal M, Chavez JC, Kharfan-Dabaja MA. Cytokine release syndrome: current perspectives. Immunotargets Ther. 2019;8:43–52.
Namuduri M, Brentjens RJ. Medical management of side effects related to CAR T cell therapy in hematologic malignancies. Expert Rev Hematol. 2016;9(6):511–3.
Rafiq S, Hackett CS, Brentjens RJ. Engineering strategies to overcome the current roadblocks in CAR T cell therapy. Nat Rev Clin Oncol. 2020;17(3):147–67.
Giordano-Attianese G, Gainza P, Gray-Gaillard E, Cribioli E, Shui S, Kim S, et al. A computationally designed chimeric antigen receptor provides a small-molecule safety switch for T-cell therapy. Nat Biotechnol. 2020;38(4):426–32.
Chong EA, Ruella M, Schuster SJ. Five-year outcomes for refractory B-cell lymphomas with CAR T-cell therapy. N Engl J Med. 2021;384(7):673–4.
Jacobson C, Locke FL, Ghobadi A, Miklos DB, Lekakis LJ, Oluwole OO, et al. Long-term survival and gradual recovery of B cells in patients with refractory large B cell lymphoma treated with axicabtagene ciloleucel (Axi-Cel). Blood. 2020;136(Supplement_1):40–2.
Xu X, Qihang S, Liang X, Chen Z, Zhang X, Zhou X, et al. Mechanisms of relapse after CD19 CAR T-cell therapy for acute lymphoblastic leukemia and its prevention and treatment strategies. Front Immunol. 2019;10:2664.
Vercellino L, Di Blasi R, Kanoun S, Tessoulin B, Rossi C, D’Aveni-Piney M, et al. Predictive factors of early progression after CAR T-cell therapy in relapsed/refractory diffuse large B-cell lymphoma. Blood Adv. 2020;4(22):5607–15.
Nie Y, Weiqing L, Chen D, Tu H, Guo Z, Zhou X, et al. Mechanisms underlying CD19-positive ALL relapse after anti-CD19 CAR T cell therapy and associated strategies. Biomark Res. 2020;8:18.
Jacobson C, Locke F, Ghobadi A, et al. Long-term (4- and 5-year) overall survival in ZUMA-1, the pivotal study of axicabtagene ciloleucel (Axi-Cel) in patients with refractory large B-cell lymphoma (LBCL). Blood. 2021;138(Supplement_1):1764.
Nie Y, Weiqing L, Chen D, et al. Mechanisms underlying CD19-positive ALL relapse after anti-CD19 CAR T cell therapy and associated strategies. Biomark Res. 2020;8:18.
Abramson JS, Palomba ML, Gordon LI, Lunning MA, Wang M, Arnason J, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839–52.
Wang M, Munoz J, Goy A, Locke FL, Jacobson CA, Hill BT, et al. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2020;382(14):1331–42.
Shah BD, Ghobadi A, Oluwole OO, Logan AC, Boissel N, Cassaday RD, et al. KTE-X19 for relapsed or refractory adult B-cell acute lymphoblastic leukaemia: phase 2 results of the single-arm, open-label, multicentre ZUMA-3 study. Lancet. 2021;398(10299):491–502.
Shah BD, Bishop MR, Oluwole OO, Logan AC, Baer MR, Donnellan WB, et al. KTE-X19 anti-CD19 CAR T-cell therapy in adult relapsed/refractory acute lymphoblastic leukemia: ZUMA-3 phase 1 results. Blood. 2021;138(1):11–22.
Johnson PC, Jacobson C, Yi A, Saucier A, Dhawale TM, Nelson A, et al. Healthcare utilization and end-of-life outcomes in patients receiving CAR T-cell therapy. J Natl Compr Canc Netw. 2021;19:1–7.
Purdum A, Johnson J, Bonagura A, Nyamutswa L, Elliot C, Lal LS. The first retrospective commercial claims-based analysis of CAR T treated patients with relapsed or refractory large B-cell lymphoma (R/R LBCL). Blood. 2020;136(Supplement_1):31.
Keating S, Gu T, Jun MP, Pelletier C, McBride A. Health care resource utilization (HCRU) and total costs of care (TCOC) among patients (pts) with diffuse large B-cell lymphoma (DLBCL) treated with chimeric antigen receptor (CAR) T-cell therapies in the United States: an analysis of four claims databases. J Clin Oncol. 2020;38:76.
Hari P, Nguyen A, Pelletier C, McGarvey N, Gitlin M, Parikh K. Healthcare resource utilization and cost of cytokine release syndrome and neurotoxicity in patients with relapsed and refractory multiple myeloma receiving the BCMA-directed chimeric antigen receptor T cell therapy idecabtagene vicleucel (ide-cel, bb2121) in the KarMMa trial. J Clin Oncol. 2020;38(29_suppl):61.
Starr, P. Real-World Healthcare Utilization and Costs Support Broader Use of CAR T-Cell Therapy. 2020 Feb. https://www.ahdbonline.com/issues/2020/february-2020-vol-13-special-issue/2921-real-world-healthcare-utilization-and-costs-support-broader-use-of-car-t-cell-therapy. Accessed 10 Mar 2022.
Sarkar RR, Gloude NJ, Schiff D, Murphy JD. Cost-effectiveness of chimeric antigen receptor T-cell therapy in pediatric relapsed/refractory B-cell acute lymphoblastic leukemia. J Natl Cancer Inst. 2019;111(7):719–26.
Lin JK, Lerman BJ, Barnes JI, Boursiquot BC, Tan YJ, Robinson AQ, et al. Cost effectiveness of chimeric antigen receptor T-cell therapy in relapsed or refractory pediatric B-cell acute lymphoblastic leukemia. J Clin Oncol. 2018;36(32):3192–202.
Whittington MD, McQueen RB, Ollendorf DA, Kuman VM, Chapman RH, Tice JA, et al. Long-term survival and value of chimeric antigen receptor T-cell therapy for pediatric patients with relapsed or refractory leukemia. JAMA Pediatr. 2018;172(12):1161–8.
Lin JK, Muffly LS, Spinner MA, Barnes JI, Owens DK, Goldhaber-Fiebert A. Cost effectiveness of chimeric antigen receptor T-cell therapy in multiply relapsed or refractory adult large B-cell lymphoma. J Clin Oncol. 2019;37(24):2105–19.
Roth JA, Sullivan SD, Lin VW, Bansal A, Purdum AG, Navale L, et al. Cost-effectiveness of axicabtagene ciloleucel for adult patients with relapsed or refractory large B-cell lymphoma in the United States. J Med Econ. 2018;21(12):1238–45.
Whittington MD, McQueen RB, Ollendorf DA, Kuman VM, Chapman RH, Tice JA, et al. Long-term survival and cost-effectiveness associated with axicabtagene ciloleucel vs chemotherapy for treatment of B-cell lymphoma. JAMA Netw Open. 2019;2(2): e190035.
Locke F, Miklos DB, Jacobson C, Perales MA, Kersten MJ, Oluwole OO, et al. Axicabtagene ciloleucel as second-line therapy for large B-cell lymphoma. N Engl J Med. 2022;386(7):640–54.
Kamdar M, Solomon SR, Arnason JE, Johnston PB, Glass B, Bachanova V, et al. Lisocabtagene maraleucel (liso-cel), a CD19-directed chimeric antigen receptor (CAR) T cell therapy, versus standard of care (SOC) with salvage chemotherapy (CT) followed by autologous stem cell transplantation (ASCT) as second-line (2L) treatment in patients (Pts) with relapsed or refractory (R/R) large B-cell lymphoma (LBCL): results from the randomized phase 3 transform study. Blood. 2021;138(Supplement_1):91.
Subklewe M. BiTEs better than CAR T cells. Blood Adv. 2021;5(2):607–12.
Salles G, Dlugosz-Danecka M, Ghesquieres H, Jurczak W. Tafasitamab for the treatment of relapsed or refractory diffuse large B-cell lymphoma. Expert Opin Biol Ther. 2021;21(4):455–63.
Staines R. Incyte/Morphosys take on CAR-Ts with $198,000 per year antibody. 2020. https://pharmaphorum.com/news/incyte-morphosys-take-on-car-ts-as-lymphoma-antibody-monjuvi-approved-in-us/. Accessed 10 Mar 2022.
Kansagra A, Farnia S, Majhail N. Expanding access to chimeric antigen receptor T-cell therapies: challenges and opportunities. Am Soc Clin Oncol Educ Book. 2020;40:1–8.
ASCO. CAR-T Therapy Policy Brief Update, in ASCO Position Statement—On Addressing the Affordability of Cancer Drugs. 2017. https://www.asco.org/sites/new-www.asco.org/files/content-files/advocacy-and-policy/documents/2017-ASCO-Position-Statement-Affordability-Cancer-Drugs-footer.pdf. Accessed 10 Mar 2022.
Geethakumari PR, Ramasamy DP, Dholaria B, Berdeja J, Kansagra A. Balancing quality, cost, and access during delivery of newer cellular and immunotherapy treatments. Curr Hematol Malig Rep. 2021;16(4):345–56.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access publication was funded by Cardinal Health. No external funding was used in the preparation of this article.
Conflicts of interest
Ajeet Gajra is a Cardinal Health employee, owns Cardinal Health stock, and is an employee of ICON Clinical Research. Abigail Zalenski is a Cardinal Health employee. Yolaine Jeune-Smith is a Cardinal Health employee and owns Cardinal Health stock. Ankit Kansagra is on the advisory board for AbbVie, Alynylam® Pharmaceuticals, Bristol Myers Squibb, Cota Healthcare, GlaxoSmithKline, Janssen Pharmaceuticals, Oncopeptides, and Takeda. Aishwarya Sannareddy and Kandice Kapinos declare that they have no conflicts of interest that might be relevant to the contents of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Code availability
Not applicable.
Author contributions
All of the authors (AG, AAZ, AS, YJS, KK, and AK) participated in writing and review of the manuscript. AG and AK were responsible for conceptualization of the manuscript. All authors have read and approved the final version.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gajra, A., Zalenski, A., Sannareddy, A. et al. Barriers to Chimeric Antigen Receptor T-Cell (CAR-T) Therapies in Clinical Practice. Pharm Med 36, 163–171 (2022). https://doi.org/10.1007/s40290-022-00428-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-022-00428-w