Abstract
Purpose
This study is a meta-analysis evaluating the efficacy of central neuraxial blockade (CNB) (epidural or spinal) to facilitate fetal version.
Methods
A search with no language restriction for all available randomized controlled trials (RCT) was conducted in PUBMED on July 2, 2009, EMBASE 1980 to 2009 Week 27, Ovid MEDLINE(R) 1950 to Week 4 in June 2009, EBM Reviews - Cochrane Central Register of Controlled Trials 2nd Quarter 2009, and CINAHL on July 4, 2009. Reference lists of all studies were also checked. Two investigators extracted data independently. The optimal information size (OIS) was calculated on a 50% failure rate of fetal version for a relative reduction of 25% (α = 0.05 two-tailed, β = 0.2).
Results
The OIS was 494. Seven RCTs were found, including 681 pregnant women with a Jadad score from 1 to 3. Central neuraxial blockade increases the success rate of fetal version (risk ratio [RR] = 1.44; 95% confidence interval [CI] = 1.16-1.79; P = 0.001) (random effects model; I2 = 30.25%; P value for heterogeneity = 0.20). Three studies used a CNB at anesthetic dose of local anesthetic (RR = 1.95; 95% CI = 1.46-2.60; P < 0.001; I2 = 0.00%; P value for heterogeneity = 0.86; number needed to treat = 4; 95% CI = 3-6). Four studies used an analgesic dose (RR = 1.18; 95% CI = 0.94-1.49; P = 0.15; I2 = 0.00%; P value for heterogeneity = 0.77). These two subgroups were significantly different one from the other with a P value of 0.007.
Conclusion
Anesthetic dose neuraxial blockade increases the success rate of external fetal version.
Résumé
Objectif
Il s’agit d’une méta-analyse évaluant l’efficacité des blocs périmédullaires (péridurale ou rachianesthésie) (BPM) pour accroître le taux de succès des versions fœtales.
Méthode
Une recherche dans PUBMED le 2 juillet 2009, EMBASE de 1980 à 2009 semaine 27, Ovid MEDLINE(R) de 1950 à juin semaine 4 2009, EBM Reviews - Cochrane Central Register of Controlled Trials 2e trimestre 2009 et CINAHL le 4 juillet 2009 sans restriction de langue pour toute étude randomisée contrôlée (ERC) disponible a été effectuée. La liste de références des articles a aussi été vérifiée. Les données ont été extraites indépendamment par deux chercheurs. Le nombre de patients à inclure (OIS) a été calculé pour une diminution relative du taux d’échec de 25 % à partir d’un taux de base de 50 % (α = 0,05 bilatéral; β = 0,2).
Résultats
L’OIS était égal à 494. Sept ERC incluant 681 parturientes et ayant un score de Jadad entre 1 et 3 ont été extraits. Les BPMs accroissent le taux de succès des versions fœtales [risque relatif (RR) = 1,44 (intervalle de confiance (IC) 95 % = 1,16-1,79); P = 0,001] (modèle aléatoire); I2 = 30,25 %; valeur de P pour l’hétérogénéité = 0,20. Trois études ont utilisé un BPM avec anesthésique local à dose anesthésique RR = 1,95 (IC 95 % = 1,46-2,60); P < 0,001; I2 = 0,00 %; P pour l’hétérogénéité = 0,86; nombre de sujets à traiter = 4 (IC 95 % = 3-6). Quatre ont utilisé une dose analgésique RR = 1,18 (IC 95 % = 0,94-1,49); P = 0,15; I2 = 0,00 %; P pour l’hétérogénéité = 0,77. Ces deux sous-groupes sont significativement différents l’un de l’autre avec une valeur de P de 0,007.
Conclusion
À dose anesthésique, les blocs périmédullaires accroissent le taux de succès des versions fœtales.
Similar content being viewed by others
The incidence of breech presentation is approximately 3% of term pregnancies. Delivery of a breech is associated with significant fetal morbidity and mortality. Fetal version is commonly practiced in order to avoid a Cesarean delivery, which is associated with significant morbidity for the mother and increases health care costs. Pain relief is said to be a significant factor associated with a successful fetal version.1 Therefore, central neuraxial blocks (CNB), which offer excellent pain control, have been proposed to increase the success rate of fetal versions. However, the results of studies on the efficacy of CNBs to increase the success rate of fetal versions have been contradictory; some have reported a clear benefit while others have not.
The purpose of this meta-analysis was to evaluate the efficacy of CNBs to increase the success rate of fetal versions.
Methods
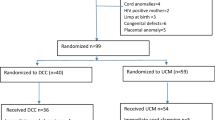
A search with no language restriction for all available randomized controlled trials (RCT) was conducted in PUBMED on July 2, 2009 using “Fetal Version AND Anesthesia limit to human”, “Fetal Version AND spinal limit to human”, “Fetal Version AND epidural limit to human”, “Fetal Version AND regional”, and “Fetal Version AND central neuraxial block”; in EMBASE 1980 to 2009 Week 27 using “Fetal.mp. AND version.mp. AND anesthesia OR caudal anesthesia OR continuous epidural anesthesia OR epidural anesthesia OR local anesthesia OR obstetric anesthesia OR regional anesthesia OR spinal anesthesia OR lumbar epidural OR thorax epidural anesthesia”; in Ovid MEDLINE(R) 1950 to Week 4 in June 2009 using “Version, Fetal AND Anesthesia OR Regional anesthesia OR Epidural OR Spinal”; in EBM Reviews - Cochrane Central Register of Controlled Trials 2nd Quarter 2009 using “fetal version.mp. AND anesthesia OR regional anesthesia.mp OR epidural.mp OR spinal.mp”; and in CINAHL on July 4, 2009 limited to female “Fetal version AND Anesthesia, Epidural OR Anesthesia, Spinal”. Reference lists of all studies as well as those of previous meta-analysis on the same topic were also checked. The flow diagram of the study selection is provided in Figure 1 (available as Electronic Supplementary Material (ESM)). Randomized controlled trials were graded on the Jadad score2 (Table 1), and authors were contacted for studies published in abstract form only.Footnote 1 , Footnote 2 The optimal information size (OIS) was calculated with a basal failure rate of 50% and a relative reduction of 25% (α 0.05 two-tailed, β 0.2) (http://www.stat.ubc.ca/~rollin/stats/ssize/b2.html).3 Data were extracted independently by the two investigators, and any disagreements were resolved by discussion. Data were entered on the side (benefit or harm) giving the lowest value for heterogeneity on the risk ratio and were analyzed with Comprehensive Meta Analysis Version 2.2.044 (www.Meta-Analysis.com) with a random effects model. Heterogeneity was assessed by dividing the studies into subgroups, i.e., those where an anesthetic dose of local anesthetic was used (capable of producing a motor block)4 - 6 and those with an analgesic dose of local anestheticA,B, 3 , 7 (Table 1). The two subgroups were analyzed with the Lan-deMets (O’Brien-Fleming) method for group sequential boundaries calculated at a cumulative α of 0.05 (2-sided symmetric) with the Lan-DeMets Group Sequential Calculations software Version 2 (Department of Biostatistics, University of Wisconsin, Madison, WI, USA). Also, a sensitivity analysis was performed that excluded study(ies) with any potentially significant and relevant disparity across study groups. The numbers needed-to-treat (NNT) were calculated from the odds ratio obtained from the meta-analysis (fixed models) entering success as the event and with a basal success rate of 37% for the analgesic group and 33% for the anesthetic group (http://www.nntonline.net/visualrx/). Instead of the risk ratio, odds ratios were chosen to calculate the NNT because they are less dependent on whether the data are entered as beneficial or adverse outcomes.8
Results
Main outcome
The OIS was 494. Seven RCTs (one identified during the review process) were found, including 681 pregnant women with a Jadad score from 1 to 3 (Table 1). In all seven studies, the position of the fetus pre- and post-attempt was confirmed by ultrasonography. An equal amount of fluid (500, 1,000, or 1,500 mL) was given in both groups for three studies only.4 , 6 , 7 (Table 2). The experience of the operator was similar for both groups in all studies but varied from one study to another (Table 2). In one study, tocolytic agents were used significantly more frequently in the control group (P < 0.0001; Chi square; GraphPad Software, San Diego, CA, USA).A In one study, the maternal age was older in the control group, but age was not a significant factor influencing the success rate at the univariate analysis (OR = 0.9; 95% CI = 0.8-1.0; P = 0.08).6 CNBs increase the success rate of fetal versions (risk ratio [RR] = 1.44; 95% CI = 1.16-1.79; P = 0.001); (random effects model; I2 = 30.25%; P value for heterogeneity = 0.20). Three studies that included 247 patients used a CNB at anesthetic dose of local anesthetic (RR= 1.95; 95% CI = 1.46-2.60; P < 0.001; I2 = 0.00%; P value for heterogeneity = 0.86; NNT = 4; 95% CI = 3-6). Four studies that included 434 patients used an analgesic dose of local anesthetic (RR = 1.18; 95% CI = 0.94-1.49; P = 0.15; I2 = 0.00%; P value for heterogeneity = 0.77; NNT = 14; 95% CI = number needed to harm 53 to number needed to benefit 6). These two subgroups were significantly different one from the other with a P value of 0.007 (Figure 1). If the study by M.F. Delisle et al. were excluded, the results would differ (RR of the analgesic dose subgroup would be 1.09; 95% CI = 0.82-1.45; P = 0.57; I2 = 0.00%; P value for heterogeneity = 0.88; and the NNT based on a success rate of 42% = 26; 95% CI = number needed to harm 12 to number needed to benefit 6).A The funnel plot showed a symmetric distribution of studies reporting either a clinical benefit or no benefit (Figure 2) (available as ESM). Therefore, there is no indication that possible missing studies would have a significant result on the effect size. When studies were divided by subgroups, the number of patients included in both subgroups did not achieve the OIS. However, an analysis with the Lan-deMets boundaries (equivalent to an interim analysis) clearly shows that the difference between CNB and no CNB anesthesia for the anesthetic subgroup is positive enough to state that CNBs at anesthetic dose increase the success rate of fetal versions (Figure 2).
Lan-deMets sequential boundaries for studies with an analgesic (A) or an anesthetic dose of local anesthetic (B). Yellow triangles represent each study data point. By adding the third study in their chronological order, the Z line (red line with yellow triangles) crosses the upper boundary line (blue dotted lines) in the anesthetic dose studies but never crosses the upper boundary line in the analgesic dose studies
Secondary outcomes
Results are available for threeB , 6 , 7 of the four studies where pain induced by the procedure was measured,A,B, 6 , 7 and they show that the CNBs statistically reduced pain scores in all three studies.
Adverse events
There was no fetal or maternal death attributed to the procedure in any of the seven RCTs, although only five of them specifically reported an absence of fetal death.A, 3 - 6 Fetal bradycardia was reported in four studies;A, 3 , 4 , 7 the incidence of transient bradycardia was 13 and 22% for the treatment groups and 11 and 15% for the control groups.3 , 7 The incidence of persistent bradycardia was 4, 15, and 29% for the treatment groups and 6, 11, and 15% for the control groups.4 , 7 The incidence of placental abruption was mentioned in four studies, with only one occurring in each treatment group (n = 2 total for all studies).B, 3 , 5 , 6 The incidence of emergency Cesarean delivery was reported in three studies, with one occurring in each treatment group (n = 2 total for all studies).3 , 6 , 7 Maternal hypotension secondary to the CNB was reported in four studies with an incidence of 0,4 8,3 19,6 and 64%.7 Two cases of post-dural puncture headache were reported, with one requiring an epidural blood patch.6
Discussion
The efficacy of CNBs in reducing the failure rate of fetal versions has been examined in prior meta-analyses (including four or five studies).9 , 10 A significant heterogeneity between studies was mentioned without any definitive explanation. In the present meta-analysis, heterogeneity disappeared when the studies were divided into those where an anesthetic dose of local anesthetic was administered that was capable of producing a motor block (spinal bupivacaine 7.5 mg, or 2% epidural lidocaine to induce a sensory level at T6, or epidural lidocaine 260 mg) or where an analgesic dose of local anesthetic was administered (spinal bupivacaine 2.5 mg, with or without epidural lidocaine 45 mg, or spinal lidocaine 6 mg) (Table 1). In earlier texts, however, there was recognition of the importance of motor blockade on the use of general anesthesia to facilitate fetal versions where suxamethonium was added when the procedure failed after a combination of thiopental and nitrous oxide.11 Although this was not a major outcome of the study by Sullivan et al., their subjective assessment of abdominal relaxation was said to have been greater in patients who had successful version.7 A fluid bolus is usually administered before a CNB, and this may increase the amount of amniotic fluid.12 However, it seems unlikely that this would explain the increased rate of successful fetal version with CNBs at anesthetic dose. In three of the studies, the same amount of fluid was administered in both groups, and two of the three studies reported an increased rate of success with CNBs (Table 2).4 , 6 , 7
When the studies were subdivided into anesthetic dose of local anesthetic vs no anesthetic dose, the number of patients in each subgroup fell below the OIS. However, when the anesthetic dose subgroup of studies was submitted for analysis with the Lan-deMets sequential boundaries (equivalent to an interim analysis) to verify that the subgroup’s significant P value was not merely a lucky finding, it became obvious that the effect could be considered significant even if there were fewer patients than the calculated OIS (Figure 2).13 With the criteria defined in our method section, it is possible that the number of patients included in the analgesic dose subgroup was insufficient to eliminate a difference between the CNB group and the control group. However, with a NNT of 14 compared with four in the anesthetic dose subgroup, if a CNB had an effect at analgesic dose, it can be concluded that the effect would be too small to be of clinical relevance.
None of the studies were blinded. As noted by one group of investigators, blinding would probably be difficult to achieve for this type of study because the obstetrician would be aware of the randomization due to the difference in patient comfort during the procedure.6 Likewise, with the exception of one study, a clear analgesia protocol is lacking for the control groups.7 However, if we consider the subgroup of studies of CNBs at analgesic dose as a group with optimal analgesia, we can conclude that an anesthetic dose is useful because it reduces the NNT from 14 to four. When measured, pain was said to be significantly lower with a neuraxial block. Adequate pain treatment may not only affect the patient’s overall experience during the procedure, but it may also prevent premature cessation of the procedure.
Two studies reported an unequal distribution of patients between their treated group and their control group.A, 6 In one study, the maternal age was older in the control group.6 Maternal age, however, is not recognized as a factor known to influence the success rate and did not result as statistically significant.6 In the study by Delisle et al., a greater number of patients received a tocolytic agent in the control group.A The use of routine tocolytic agents has been identified has a factor increasing the success rate of fetal versions.10 If this study were excluded from the analgesic subgroup, the effect of a CNB would remain statistically insignificant, and the potential clinical relevance would decrease rather than increase. Therefore, we do not think that these two inequalities in the groups affect the conclusions of our meta-analysis. Experience of the operators varied significantly from one study to another, but this does not seem to affect the efficacy of the CNB because the heterogeneity of both subgroups was 0%.
Although it is considered a safe procedure, fetal version carries a significant morbidity: transient (5.7%) or persisting (0.37%) abnormal cardiotocography patterns, vaginal bleeding (0.47%), placental abruption (0.12%), fetomaternal transfusion (3.7%), emergency Cesarean deliveries (0.43%), and perinatal mortality (0.16%.).14 , 15 Apart from maternal hypotension, a known side effect of CNBs, CNBs do not appear to increase serious adverse events associated with fetal version.
In conclusion, neuraxial blockade with surgical anesthetic doses increases the likelihood of successful external cephalic version for breech position.
Notes
Delisle MF, Kamani AA, Douglas MJ, Bebbington MW. Antepartum external cephalic version under spinal anesthesia: A randomized controlled study. J Obstet Gynaecol Can 2003; 25(Suppl): S13 (abstract).
Hollard A, Lyons C, Rumney P, Hunter M, Reed E, Nageotte M. The effect of intrathecal anesthesia on the success of external cephalic version (ECV). Am J Obstet Gynecol 2003; 189(Suppl 1): S140 (abstract).
References
Hutton EK, Saunders CA, Tu M, Stoll K, Berkowitz J, Early External Cephalic Version Trial Collaborators Group. Factors associated with a successful external cephalic version in the early ECV trial. J Obstet Gynaecol Can 2008; 30: 23-8.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17: 1-12.
Dugoff L, Stamm CA, Jones OW 3rd, Mohling SI, Hawkins JL. The effect of spinal anesthesia on the success rate of external cephalic version: a randomized trial. Obstet Gynecol 1999; 93: 345-9.
Mancuso KM, Yancey MK, Murphy JA, Markenson GR. Epidural analgesia for cephalic version: a randomized trial. Obstet Gynecol 2000; 95: 648-51.
Schorr SJ, Speights SE, Ross EL, et al. A randomized trial of epidural anesthesia to improve external cephalic version success. Am J Obstet Gynecol 1997; 177: 1133-7.
Weiniger CF, Ginosar Y, Elchalal U, Sharon E, Nokrian M, Ezra Y. External cephalic version for breech presentation with or without spinal analgesia in nulliparous women at term: a randomized controlled trial. Obstet Gynecol 2007; 110: 1343-50.
Sullivan JT, Grobman WA, Bauchat JR, et al. A randomized controlled trial of the effect of combined spinal-epidural analgesia on the success of external cephalic version for breech presentation. Int J Obstet Anesth 2009; 18: 328-34.
Cates CJ. Simpson’s paradox and calculation of number needed to treat from meta-analysis. BMC Med Res Methodol 2002; 2: 1.
Macarthur AJ, Gagnon S, Tureanu LM, Downey KN. Anesthesia facilitation of external cephalic version: a meta-analysis. Am J Obstet Gynecol 2004; 191: 1219-24.
Hofmeyr GJ. Interventions to help external cephalic version for breech presentation at term. Cochrane Database Syst Rev 2004; (1): CD000184
Neely MR. External cephalic version under anaesthesia. Results in a series of 102 cases. J Obstet Gynaecol Br Emp 1961; 68: 490-7.
Modena AB, Fieni S. Amniotic fluid dynamics. Acta Biomed 2004; 75(Suppl 1): 11-3.
Pogue JM, Yusuf S. Cumulating evidence from randomized trials: utilizing sequential monitoring boundaries for cumulative meta-analysis. Control Clin Trials 1997; 18: 580-93.
Collaris RJ, Oei SG. External cephalic version: a safe procedure? A systematic review of version-related risks. Acta Obstet Gynecol Scand 2004; 83: 511-8.
Nassar N, Roberts CL, Barratt A, Bell JC, Olive EC, Peat B. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol 2006; 20: 163-71.
Acknowledgements
The authors are grateful to the University of Montreal and Maisonneuve-Rosemont Hospital for granting access to electronic databases and references.
Disclosure
Access to electronic data-bases and references were provided by University of Montreal and Maisonneuve-Rosemont Hospital. The authors have no other disclosure.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lavoie, A., Guay, J. Anesthetic dose neuraxial blockade increases the success rate of external fetal version: a meta-analysis. Can J Anesth/J Can Anesth 57, 408–414 (2010). https://doi.org/10.1007/s12630-010-9278-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-010-9278-4