Abstract
Background
Normobaric oxygen therapy is frequently applied in neurocritical care, however, whether supplemental FiO2 has beneficial cerebral effects is still controversial. We examined in patients with severe traumatic brain injury (TBI) the effect of incremental FiO2 on cerebral excitotoxicity, quantified by cerebral microdialysis (CMD) glutamate.
Methods
This was a retrospective analysis of a database of severe TBI patients monitored with CMD and brain tissue oxygen (PbtO2). The relationship of FiO2—categorized into four separate ranges (<40, 41–60, 61–80, and >80 %)—with CMD glutamate was examined using ANOVA with Tukey’s post hoc test.
Results
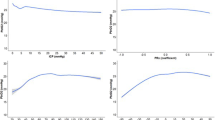
A total of 1,130 CMD samples from 36 patients—monitored for a median of 4 days—were examined. After adjusting for brain (PbtO2, intracranial pressure, cerebral perfusion pressure, lactate/pyruvate ratio, Marshall CT score) and systemic (PaCO2, PaO2, hemoglobin, APACHE score) covariates, high FiO2 was associated with a progressive increase in CMD glutamate [8.8 (95 % confidence interval 7.4–10.2) µmol/L at FiO2 < 40 % vs. 12.8 (10.9–14.7) µmol/L at 41–60 % FiO2, 19.3 (15.6–23) µmol/L at 61–80 % FiO2, and 22.6 (16.7–28.5) µmol/L at FiO2 > 80 %; multivariate-adjusted p < 0.05]. The threshold of FiO2-related increase in CMD glutamate was lower for samples with normal versus low PbtO2 < 20 mmHg (FiO2 > 40 % vs. FiO2 > 60 %). Hyperoxia (PaO2 > 150 mmHg) was also associated with increased CMD glutamate (adjusted p < 0.001).
Conclusions
Incremental normobaric FiO2 levels were associated with increased cerebral excitotoxicity in patients with severe TBI, independent from PbtO2 and other important cerebral and systemic determinants. These data suggest that supra-normal oxygen may aggravate secondary brain damage after severe TBI.




Similar content being viewed by others
References
Oddo M, Levine JM, Mackenzie L, et al. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery. 2011;69:1037–45 discussion 45.
McCarthy MC, Moncrief H, Sands JM, et al. Neurologic outcomes with cerebral oxygen monitoring in traumatic brain injury. Surgery. 2009;146:585–90; discussion 90-1.
Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg. 2009;111:672–82.
Spiotta AM, Stiefel MF, Gracias VH, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113:571–80.
Stiefel MF, Spiotta A, Gracias VH, et al. Reduced mortality rate in patients with severe traumatic brain injury treated with brain tissue oxygen monitoring. J Neurosurg. 2005;103:805–11.
Fletcher JJ, Bergman K, Blostein PA, Kramer AH. Fluid balance, complications, and brain tissue oxygen tension monitoring following severe traumatic brain injury. Neurocrit Care. 2010;13:47–56.
Martini RP, Deem S, Yanez ND, et al. Management guided by brain tissue oxygen monitoring and outcome following severe traumatic brain injury. J Neurosurg. 2009;111:644–9.
Meixensberger J, Jaeger M, Vath A, Dings J, Kunze E, Roosen K. Brain tissue oxygen guided treatment supplementing ICP/CPP therapy after traumatic brain injury. J Neurol Neurosurg Psychiatry. 2003;74:760–4.
Bohman LE, Heuer GG, Macyszyn L, et al. Medical management of compromised brain oxygen in patients with severe traumatic brain injury. Neurocrit Care. 2011;14:361–9.
Kumaria A, Tolias CM. Normobaric hyperoxia therapy for traumatic brain injury and stroke: a review. Br J Neurosurg. 2009;23:576–84.
Diringer MN. Hyperoxia: good or bad for the injured brain? Curr Opin Crit Care. 2008;14:167–71.
Beynon C, Kiening KL, Orakcioglu B, Unterberg AW, Sakowitz OW. Brain tissue oxygen monitoring and hyperoxic treatment in patients with traumatic brain injury. J Neurotrauma. 2012;29:2109–23.
Sjoberg F, Singer M. The medical use of oxygen: a time for critical reappraisal. J Intern Med. 2013;274:505–28.
Brenner M, Stein D, Hu P, Kufera J, Wooford M, Scalea T. Association between early hyperoxia and worse outcomes after traumatic brain injury. Arch Surg. 2012;147:1042–6.
Rincon F, Kang J, Vibbert M, Urtecho J, Athar MK, Jallo J. Significance of arterial hyperoxia and relationship with case fatality in traumatic brain injury: a multicentre cohort study. J Neurol Neurosurg Psychiatry 2014;85(7):799–805.
Davis DP, Meade W, Sise MJ, et al. Both hypoxemia and extreme hyperoxemia may be detrimental in patients with severe traumatic brain injury. J Neurotrauma. 2009;26:2217–23.
Kilgannon JH, Jones AE, Parrillo JE, et al. Relationship between supranormal oxygen tension and outcome after resuscitation from cardiac arrest. Circulation. 2011;123:2717–22.
Solberg R, Longini M, Proietti F, Vezzosi P, Saugstad OD, Buonocore G. Resuscitation with supplementary oxygen induces oxidative injury in the cerebral cortex. Free Radic Biol Med. 2012;53:1061–7.
Blasiole B, Bayr H, Vagni VA, et al. Effect of hyperoxia on resuscitation of experimental combined traumatic brain injury and hemorrhagic shock in mice. Anesthesiology. 2013;118:649–63.
McKenna MC. The glutamate–glutamine cycle is not stoichiometric: fates of glutamate in brain. J Neurosci Res. 2007;85:3347–58.
Schmitz T, Ritter J, Mueller S, Felderhoff-Mueser U, Chew LJ, Gallo V. Cellular changes underlying hyperoxia-induced delay of white matter development. J Neurosci. 2011;31:4327–44.
Hillered L, Vespa PM, Hovda DA. Translational neurochemical research in acute human brain injury: the current status and potential future for cerebral microdialysis. J Neurotrauma. 2005;22:3–41.
Oddo M, Villa F, Citerio G. Brain multimodality monitoring: an update. Curr Opin Crit Care. 2012;18:111–8.
Timofeev I, Carpenter KL, Nortje J, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a microdialysis study of 223 patients. Brain. 2011;134:484–94.
Marshall LF, Marshall SB, Klauber MR, et al. The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma. 1992;9(Suppl 1):S287–92.
Bratton SL, Chestnut RM, Ghajar J, McConnell HF, Harris OA, Hartl R, Manley GT, et al. Guidelines for the management of severe traumatic brain injury. X. Brain oxygen monitoring and thresholds. J Neurotrauma. 2007;24(Suppl 1):S65–70.
Narayan RK, Kishore PR, Becker DP, Ward JD, Enas GG, Greenberg RP, Domingues Da Silva A, et al. Guidelines for the management of severe traumatic brain injury. VII. Intracranial pressure monitoring technology. J Neurotrauma. 2007;24(Suppl 1):S45–54.
Sala N, Suys T, Zerlauth JB, et al. Cerebral extracellular lactate increase is predominantly nonischemic in patients with severe traumatic brain injury. Journal Cereb Blood Flow Metab. 2013;33:1815–22.
Brower RG, Rubenfeld GD. Lung-protective ventilation strategies in acute lung injury. Crit Care Med. 2003;31:S312–6.
Force ADT, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA J Am Med Assoc. 2012;307:2526–33.
Muthuraju S, Pati S, Rafiqul M, Abdullah JM, Jaafar H. Effect of normabaric hyperoxia treatment on neuronal damage following fluid percussion injury in the striatum of mice: a morphological approach. J Biosci. 2013;38:93–103.
Palzur E, Vlodavsky E, Mulla H, Arieli R, Feinsod M, Soustiel JF. Hyperbaric oxygen therapy for reduction of secondary brain damage in head injury: an animal model of brain contusion. J Neurotrauma. 2004;21:41–8.
Moody RA, Mead CO, Ruamsuke S, Mullan S. Therapeutic value of oxygen at normal and hyperbaric pressure in experimental head injury. J Neurosurg. 1970;32:51–4.
Chen T, Qian YZ, Di X, Rice A, Zhu JP, Bullock R. Lactate/glucose dynamics after rat fluid percussion brain injury. J Neurotrauma. 2000;17:135–42.
Rostami E, Rocksen D, Ekberg NR, Goiny M, Ungerstedt U. Brain metabolism and oxygenation in healthy pigs receiving hypoventilation and hyperoxia. Respir Physiol Neurobiol. 2013;189:537–42.
Nortje J, Coles JP, Timofeev I, et al. Effect of hyperoxia on regional oxygenation and metabolism after severe traumatic brain injury: preliminary findings. Crit Care Med. 2008;36:273–81.
Diringer MN, Aiyagari V, Zazulia AR, Videen TO, Powers WJ. Effect of hyperoxia on cerebral metabolic rate for oxygen measured using positron emission tomography in patients with acute severe head injury. J Neurosurg. 2007;106:526–9.
Magnoni S, Ghisoni L, Locatelli M, et al. Lack of improvement in cerebral metabolism after hyperoxia in severe head injury: a microdialysis study. J Neurosurg. 2003;98:952–8.
Kilgannon JH, Jones AE, Shapiro NI, et al. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA J Am Med Assoc. 2010;303:2165–71.
Rincon F, Kang J, Maltenfort M, et al. Association between hyperoxia and mortality after stroke: a multicenter cohort study. Crit Care Med. 2014;42:387–96.
de Jonge E, Peelen L, Keijzers PJ, et al. Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care. 2008;12:R156.
Rangel-Castilla L, Lara LR, Gopinath S, Swank PR, Valadka A, Robertson C. Cerebral hemodynamic effects of acute hyperoxia and hyperventilation after severe traumatic brain injury. J Neurotrauma. 2010;27:1853–63.
Wang M, Luo Z, Liu S, et al. Glutamate mediates hyperoxia-induced newborn rat lung injury through N-methyl-d-aspartate receptors. Am J Respir Cell Mol Biol. 2009;40:260–7.
D’Agostino DP, Pilla R, Held HE, et al. Therapeutic ketosis with ketone ester delays central nervous system oxygen toxicity seizures in rats. Am J Physiol Regul Integr Comp Physiol. 2013;304:R829–36.
Vespa P, Prins M, Ronne-Engstrom E, et al. Increase in extracellular glutamate caused by reduced cerebral perfusion pressure and seizures after human traumatic brain injury: a microdialysis study. J Neurosurg. 1998;89:971–82.
Thomas PM, Phillips JP, Delanty N, O’Connor WT. Elevated extracellular levels of glutamate, aspartate and gamma-aminobutyric acid within the intraoperative, spontaneously epileptiform human hippocampus. Epilepsy Res. 2003;54:73–9.
Puccio AM, Hoffman LA, Bayir H, et al. Effect of short periods of normobaric hyperoxia on local brain tissue oxygenation and cerebrospinal fluid oxidative stress markers in severe traumatic brain injury. J Neurotrauma. 2009;26:1241–9.
Tisdall MM, Tachtsidis I, Leung TS, Elwell CE, Smith M. Increase in cerebral aerobic metabolism by normobaric hyperoxia after traumatic brain injury. J Neurosurg. 2008;109:424–32.
Tolias CM, Reinert M, Seiler R, Gilman C, Scharf A, Bullock MR. Normobaric hyperoxia-induced improvement in cerebral metabolism and reduction in intracranial pressure in patients with severe head injury: a prospective historical cohort-matched study. J Neurosurg. 2004;101:435–44.
Rockswold SB, Rockswold GL, Zaun DA, et al. A prospective, randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism, intracranial pressure, and oxygen toxicity in severe traumatic brain injury. J Neurosurg. 2010;112:1080–94.
Rockswold SB, Rockswold GL, Zaun DA, Liu J. A prospective, randomized phase II clinical trial to evaluate the effect of combined hyperbaric and normobaric hyperoxia on cerebral metabolism, intracranial pressure, oxygen toxicity, and clinical outcome in severe traumatic brain injury. J Neurosurg. 2013;118:1317–28.
Acknowledgments
This work was supported by grants from the Swiss National Science Foundation (Grant No. 320030_138191, to Mauro Oddo), the Novartis Foundation for Biomedical Research (to Mauro Oddo) and the Société Française d’Anesthésie et Réanimation (SFAR) (to Hervé Quintard). The authors thank Professor Lucas Liaudet, MD, for helpful scientific discussion.
Conflict of interest
All authors declare they have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quintard, H., Patet, C., Suys, T. et al. Normobaric Hyperoxia is Associated with Increased Cerebral Excitotoxicity After Severe Traumatic Brain Injury. Neurocrit Care 22, 243–250 (2015). https://doi.org/10.1007/s12028-014-0062-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0062-0