Abstract
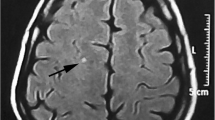
Patients with migraine are at increased risk for white matter hyperintensities detected on magnetic resonance imaging. The presence of nonspecific white matter hyperintensities may cause uncertainty for physicians and anxiety for patients. The pathophysiology and long-term consequences of these lesions are unknown. Occasionally, white matter lesions in a migraineur may indicate an underlying disease such as cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), mitochondrial encephalopathy with lactic acidosis and stroke-like episodes (MELAS), or central nervous system vasculitis. The ability to distinguish between nonspecific and disease-specific patterns of white matter hyperintensities in migraine sufferers is important for the practicing clinician.
Similar content being viewed by others
References and Recommended Reading
Frishberg BM, Rosenberg JH, Matchar DB, et al.: Evidencebased guidelines in the primary care setting: neuroimaging in patients with nonacute headache. URL:http:// www.aan.com/public/practiceguidelines. Accessed May 2005.
Evans RW: Diagnostic testing for headache. Med Clin North Am 2001, 85:865–885.
Fazekas F: Magnetic resonance signal abnormalities in asymptomatic individuals: their incidence and functional correlates. Eur Neurol 1989, 29:164–168.
Schmidt R, Fazekas F, Kleinert G, et al.: Magnetic resonance imaging signal hyperintensities in the deep and subcortical white matter: a comparative study between stroke patients and normal volunteers. Arch Neurol 1992, 49:825–827.
Oyama H, Kida Y, Tanaka T: Incidental white matter lesions identified on magnetic resonance images of normal Japanese individuals: correlation with age and hypertension. Neurol Med Chir (Tokyo) 1994, 34:286–290.
Ketonen LM: Neuroimaging of the aging brain. Neurol Clin 1998, 16:581–598.
de Groot JC, de Leeuw FE, Oudkerk M, et al.: Cerebral white matter lesions and cognitive function: the Rotterdam Scan Study. Ann Neurol 2000, 47:145–151.
Manolio TA, Kronmal RA, Burke GL, et al.: Magnetic resonance abnormalities and cardiovascular disease in older adults. The Cardiovascular Health Study. Stroke 1994, 25:318–327.
Lindgren A, Roijer A, Rudling O, et al.: Cerebral lesions on magnetic resonance imaging, heart disease, and vascular risk factors in subjects without stroke: a population-based study. Stroke 1994, 25:929–934.
Barkhof F, Scheltens P: Imaging of white matter lesions. Cerebrovas Dis 2002, 13(suppl 2):21–30.
Longstreth WT, Manolio TA, Arnold A, et al.: Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people: the Cardiovascular Heath Study. Stroke 1996, 27:1274–1282.
Golomb J, Kluger A, Gianutsos J, et al.: Nonspecific leukoencephalopathy associated with aging. Neuroimaging Clin N Am 1995, 5:33–44.
Vermeer SE, Prins ND, den Heijer T, et al.: Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med 2003, 348:1215–1222.
Osborn RE, Alder DC, Mitchell CS: MR imaging of the brain in patients with migraine headaches. Am J Neuroradiol 1991, 12:521–524.
Ziegler D, Batnitzky S, Barter R, et al.: Magnetic resonance imaging abnormalities in migraine with aura. Cephalalgia 1991, 11:147–150.
Cooney BS, Grossman RI, Farber RE, et al.: Frequency of magnetic resonance imaging abnormalities in patients with migraine. Headache 1996, 36:616–621.
Robbins L, Friedman H. MRI in migraineurs. Headache 1992, 32:507–508.
Igarashi H, Sakai F, Kan S, et al.: Magnetic resonance imaging of the brain in patients with migraine. Cephalalgia 1991, 11:69–74.
Pavese N, Canapicchi R, Nuti A, et al.: White matter MRI hyperintensities in a hundred and 29 consecutive migraine patients. Cephalalgia 1994, 14:342–345.
De Benedittis D, Lorenzetti A, Sina C, et al.: Magnetic resonance imaging in migraine and tension-type headache. Headache 1995, 36:264–248.
Fazekas F, Koch M, Schmidt R, et al.: The prevalence of cerebral damage varies with migraine type: a MRI study. Headache 1992, 32:287–291.
Gozke E, Ore O, Dortcan N, et al.: Cranial magnetic resonance imaging findings in patients with migraine. Headache 2004, 44:166–169.
Swartz RH, Kern RZ: Migraine is associated with MRI white matter abnormalities: a meta-analysis. Arch Neur 2004, 61:1366–1368. Meta-analysis confirms the increased risk of white matter hyperintensities in migraine.
Kruit MC, van Buchem MA, Hofman PA, et al.: Migraine as a risk factor for subclinical brain lesions. JAMA 2004, 291:427–434. Cross-sectional study that analyzes the prevalence of deep and periventricular WMHS and infarction on MRI in migraineurs with and without aura and control subjects.
Gozke E, Ore O, Dortcan N, et al.: Cranial magnetic resonance imaging findings in patients with migraine. Headache 2004, 44:166–169.
Swartz RH, Kern RZ: Migraine is associated with MRI white matter abnormalities: a meta-analysis. Arch Neurol 2004, 61:1366–1368.
Goadsby PJ: Migraine pathophysiology. Headache 2005, 45(suppl 1):S14-S24.
Crassard I, Conard J, Bousser MG: Migriane and haemostasis. Cephalalgia 2001, 21:630–636.
Tzourio C, El Amrani M, Poirier O, et al.: Association between migraine and endothelin type A receptor (ETA-231 A/G) gene polymorphism. Neurology 2001, 56:1273–1277.
Cutrer FM, Sorensen AG, Weisskoff RM, et al.: Perfusionweighted imaging defects during spontaneous migrainous aura. Ann Neurol 1998, 43:25–31.
Bednarczyk EM, Remier B, Weikart C, et al.: Global cerebral blood flow, blood volume, and oxygen metabolism in patients with migraine headache. Neurology 1998, 50:1736–1740.
Gladstone JP, Dodick DW. Migraine and cerebral white matter lesions: when to suspect cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). Neurologist 2005, 11:19–29.
Gursoy-Ozdemir Y, Qiu J, Matsuoka N, et al.: Cortical spreading depression activates and upregulates MMP-9. J Clin Invest 2004, 113:1447–1455.
Anzola GP, Magoni M, Guidani M, et al.: Potential source of cerebral embolism in migraine with aura: a transcranial Doppler study. Neurology 1999, 52:1622–1625.
Schwerzmann M, Wiher S, Nedeltchev K, et al.: Percutaneous closure of patent foramen ovale reduces the frequency of migraine attacks. Neurology 2004, 62:1399–1401.
Diener HC, Weimar C, Katsarava Z: Patent foramen ovale: paradoxical connection to migraine and stroke. Curr Opin Neurol 2005, 18:299–304.
Tsimikas S: Transcatheter closure of patent foramen ovale for migraine prophylaxis: hope or hype? J Am Coll Cardiol 2005, 45:496–498.
Holmes DR Jr: Strokes and holes and headaches: Are they a package deal? Lancet 2004, 364:1840–1842.
Chabriat H, Bousser MG: Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Adv Neurol 2003, 92:147–150.
Dichigans M: CADASIL: a monogenic condition causing stroke and subcortical vascular dementia. Cerebrovasc Dis 2002, 13(suppl 2):37–41.
Dichigans M: Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy: phenotypic and mutational spectrum. J Neurol Sci 2002, 203:77–80.
Dichigans M, Mayer M, Uttner I, et al.: The phenotypic spectrum of CADASIL: clinical findings in 102 cases. Ann Neurol 1998, 44:731–739.
Desmond DW, Moroney JT, Lynch T, et al.: The natural history of CADASIL: a pooled analysis of previously published cases. Stroke 1999, 30:1230–1233.
Razvi SS, Muir KW: Cerebral autosomal dominant arteriopathy with sucortical infarcts and leukoencephalopathy (CADASIL). Pract Neurol 2004, 4:50–55.
O’Sullivan M, Jarosz JM, Martin RJ, et al.: MRI hyperintensities of the temporal lobe and external capsule in patients with CADASIL. Neurology 2001, 56:628–634.
Dichgans M, Holtmannspotter M, Herzog J, et al.: Cerebral microbleeds in CADASIL: a gradient-echo magnetic resonance imaging and autopsy study. Stroke 2002, 33:67–71.
Chawda SJ, De Lange RP, Hourihan MD, et al.: Diagnosing CADASIL using MRI: evidence from families with known mutations of Notch 3 gene. Neuroradiology 2000, 42:249–255.
Paty DW, Oger JJ, Kastrukoff LF, et al.: Magnetic resonance imaging in the diagnosis of multiple sclerosis: a prospective study of comparison with clinical evaluation, evoked potential, oligoclonal banding, and CT. Neurology 1988, 38:180–185.
Barkhof F, Filippi M, Miller DH, et al.: Comparison of MRI criteria at first presentation to predict conversion to clinical definite multiple sclerosis. Brain 1997, 120:2059–2069.
Clark JM, Marks MP, Adalsteinsson E, et al.: MELAS: clinical and pathologic correlations with MRI, Xenon/CT, and MR spectroscopy. Neurology 1996, 46:223–227.
Iizuka T, Sakai F, Kan S, Suzuki N: Slowly progressive spread of the stroke-like lesions in MELAS. Neurology 2003, 61:1238–1244.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Porter, A., Gladstone, J.P. & Dodick, D.W. Migraine and white matter hyperintensities. Current Science Inc 9, 289–293 (2005). https://doi.org/10.1007/s11916-005-0039-y
Issue Date:
DOI: https://doi.org/10.1007/s11916-005-0039-y