Abstract
Purpose
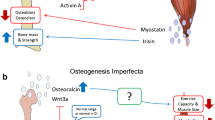
Here, we review the skeletal effects of pediatric muscle disorders as well as muscle impairment in pediatric bone disorders.
Recent Findings
When starting in utero, muscle disorders can lead to congenital multiple contractures. Pediatric-onset muscle weakness such as cerebral palsy, Duchenne muscular dystrophy, spinal muscular atrophy, or spina bifida typically are associated with small diameter of long-bone shafts, low density of metaphyseal bone, and increased fracture incidence in the lower extremities, in particular, the distal femur. Primary bone diseases can affect muscles through generic mechanisms, such as decreased physical activity or in disease-specific ways. For example, the collagen defect underlying the bone fragility of osteogenesis imperfecta may also affect muscle force generation or transmission. Transforming growth factor beta released from bone in Camurati Engelman disease may decrease muscle function.
Future Directions
Considering muscle-bone interactions does not only contribute to the understanding of musculoskeletal disorders but also can identify new targets for therapeutic interventions.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •Of importance ••Of major importance
Frost HM. Bone’s mechanostat: a 2003 update. Anat Rec A Discov Mol Cell Evol Biol. 2003;275:1081–101.
Hall JG, Aldinger KA, Tanaka KI. Amyoplasia revisited. Am J Med Genet A. 2014;164a:700–30.
Hall JG. Arthrogryposis (multiple congenital contractures): diagnostic approach to etiology, classification, genetics, and general principles. Eur J Med Genet. 2014;57:464–72.
Spencer HT, Bowen RE, Caputo K, Green TA, Lawrence JF. Bone mineral density and functional measures in patients with arthrogryposis. J Pediatr Orthop. 2010;30:514–8.
Simone C, Ramirez A, Bucchia M, Rinchetti P, Rideout H, Papadimitriou D, et al. Is spinal muscular atrophy a disease of the motor neurons only: pathogenesis and therapeutic implications? Cell Mol Life Sci. 2016;73:1003–20.
Knierim E, Hirata H, Wolf NI, Morales-Gonzalez S, Schottmann G, Tanaka Y, et al. Mutations in subunits of the activating signal cointegrator 1 complex are associated with prenatal spinal muscular atrophy and congenital bone fractures. Am J Hum Genet. 2016;98:473–89.
Moon RJ, Harvey NC, Curtis EM, de Vries F, van Staa T, Cooper C. Ethnic and geographic variations in the epidemiology of childhood fractures in the United Kingdom. Bone. 2016;85:9–14.
Colver A, Fairhurst C, Pharoah PO. Cerebral palsy. Lancet. 2014;383:1240–9.
Mughal MZ. Fractures in children with cerebral palsy. Curr Osteoporos Rep. 2014;12:313–8.
Uddenfeldt Wort U, Nordmark E, Wagner P, Duppe H, Westbom L. Fractures in children with cerebral palsy: a total population study. Dev Med Child Neurol. 2013;55:821–6.
• Modlesky CM, Whitney DG, Singh H, Barbe MF, Kirby JT, Miller F. Underdevelopment of trabecular bone microarchitecture in the distal femur of nonambulatory children with cerebral palsy becomes more pronounced with distance from the growth plate. Osteoporos Int. 2015;26:505–12. This study provides MRI-based structural data that underpin the low metaphyseal femoral bone density in children with cerebral palsy.
Modlesky CM, Kanoff SA, Johnson DL, Subramanian P, Miller F. Evaluation of the femoral midshaft in children with cerebral palsy using magnetic resonance imaging. Osteoporos Int. 2009;20:609–15.
Binkley T, Johnson J, Vogel L, Kecskemethy H, Henderson R, Specker B. Bone measurements by peripheral quantitative computed tomography (pQCT) in children with cerebral palsy. J Pediatr. 2005;147:791–6.
Whitney DG, Singh H, Miller F, Barbe MF, Slade JM, Pohlig RT, et al. Cortical bone deficit and fat infiltration of bone marrow and skeletal muscle in ambulatory children with mild spastic cerebral palsy. Bone. 2017;94:90–7.
Trudel G, Payne M, Madler B, Ramachandran N, Lecompte M, Wade C, et al. Bone marrow fat accumulation after 60 days of bed rest persisted 1 year after activities were resumed along with hemopoietic stimulation: the women international space simulation for exploration study. J Appl Physiol. 2009;107:540–8.
Rantalainen T, Nikander R, Heinonen A, Cervinka T, Sievanen H, Daly RM. Differential effects of exercise on tibial shaft marrow density in young female athletes. J Clin Endocrinol Metab. 2013;98:2037–44.
Mah JK. Current and emerging treatment strategies for Duchenne muscular dystrophy. Neuropsychiatr Dis Treat. 2016;12:1795–807.
Matthews E, Brassington R, Kuntzer T, Jichi F, Manzur AY. Corticosteroids for the treatment of Duchenne muscular dystrophy. Cochrane Database Syst Rev. 2016;5:Cd003725.
Tian C, Wong BL, Hornung L, Khoury JC, Miller L, Bange J, et al. Bone health measures in glucocorticoid-treated ambulatory boys with Duchenne muscular dystrophy. Neuromuscul Disord. 2016;26:760–7.
Ma J, McMillan HJ, Karaguzel G, Goodin C, Wasson J, Matzinger MA, et al. The time to and determinants of first fractures in boys with Duchenne muscular dystrophy. Osteoporos Int. 2017;28:597–608.
Singh A, Schaeffer EK, Reilly CW. Vertebral fractures in Duchenne muscular dystrophy patients managed with deflazacort. J Pediatr Orthop. 2016. doi:https://doi.org/10.1097/BPO.0000000000000817
King WM, Kissel JT, Visy D, Goel PK, Matkovic V. Skeletal health in Duchenne dystrophy: bone-size and subcranial dual-energy X-ray absorptiometry analyses. Muscle Nerve. 2014;49:512–9.
Wong BL, Rybalsky I, Shellenbarger KC, Tian C, McMahon MA, Rutter MM, et al. Long-term outcome of interdisciplinary management of patients with Duchenne muscular dystrophy receiving daily glucocorticoid treatment. J Pediatr. 2017;182:296–303 e1.
• Misof BM, Roschger P, McMillan HJ, Ma J, Klaushofer K, Rauch F, et al. Histomorphometry and bone matrix mineralization before and after bisphosphonate treatment in boys with Duchenne muscular dystrophy: a paired transiliac biopsy study. J Bone Miner Res. 2016;31:1060–9. This bone tissue study shows that bone turnover is low in boys with Duchenne muscular dystrophy but that material bone properties are largely normal.
Vai S, Bianchi ML, Moroni I, Mastella C, Broggi F, Morandi L, et al. Bone and spinal muscular atrophy. Bone. 2015;79:116–20.
Vestergaard P, Glerup H, Steffensen BF, Rejnmark L, Rahbek J, Moseklide L. Fracture risk in patients with muscular dystrophy and spinal muscular atrophy. J Rehabil Med. 2001;33:150–5.
Trinh A, Wong P, Brown J, Hennel S, Ebeling PR, Fuller PJ, et al. Fractures in spina bifida from childhood to young adulthood. Osteoporos Int. 2017;28:399–406.
Dosa NP, Eckrich M, Katz DA, Turk M, Liptak GS. Incidence, prevalence, and characteristics of fractures in children, adolescents, and adults with spina bifida. J Spinal Cord Med. 2007;30(Suppl 1):S5–9.
• Horenstein RE, Shefelbine SJ, Mueske NM, Fisher CL, Wren TA. An approach for determining quantitative measures for bone volume and bone mass in the pediatric spina bifida population. Clin Biomech (Bristol, Avon). 2015;30:748–54. This study used CT images to study three-dimensional geometry and density along the entire tibia in children with spina bifida. Non-ambulatory children had decreased bone mass in the diaphysis and proximal and distal epiphyses compared to ambulatory and control children.
Folkestad L, Hald JD, Ersboll AK, Gram J, Hermann AP, Langdahl B, et al. Fracture rates and fracture sites in patients with osteogenesis Imperfecta: a nationwide register-based cohort study. J Bone Miner Res. 2017;32:125–34.
Trejo P, Rauch F. Osteogenesis imperfecta in children and adolescents-new developments in diagnosis and treatment. Osteoporos Int. 2016;27:3427–37.
Ben Amor IM, Roughley P, Glorieux FH, Rauch F. Skeletal clinical characteristics of osteogenesis imperfecta caused by haploinsufficiency mutations in COL1A1. J Bone Miner Res. 2013;28:2001–7.
Graf A, Hassani S, Krzak J, Caudill A, Flanagan A, Bajorunaite R, et al. Gait characteristics and functional assessment of children with type I osteogenesis imperfecta. J Orthop Res. 2009;27:1182–90.
Caudill A, Flanagan A, Hassani S, Graf A, Bajorunaite R, Harris G, et al. Ankle strength and functional limitations in children and adolescents with type I osteogenesis imperfecta. Pediatr Phys Ther. 2010;22:288–95.
Veilleux LN, Lemay M, Pouliot-Laforte A, Cheung MS, Glorieux FH, Rauch F. Muscle anatomy and dynamic muscle function in osteogenesis imperfecta type I. J Clin Endocrinol Metab. 2014;99:E356–62.
Pouliot-Laforte A, Veilleux LN, Rauch F, Lemay M. Physical activity in youth with osteogenesis imperfecta type I. J Musculoskelet Neuronal Interact. 2015;15:171–6.
Veilleux LN, Pouliot-Laforte A, Lemay M, Cheung MS, Glorieux FH, Rauch F. The functional muscle-bone unit in patients with osteogenesis imperfecta type I. Bone. 2015;79:52–7.
Gillies AR, Lieber RL. Structure and function of the skeletal muscle extracellular matrix. Muscle Nerve. 2011;44:318–31.
Light N, Champion AE. Characterization of muscle epimysium, perimysium and endomysium collagens. Biochem J. 1984;219:1017–26.
Huijing PA. Muscle as a collagen fiber reinforced composite: a review of force transmission in muscle and whole limb. J Biomech. 1999;32:329–45.
Misof K, Landis WJ, Klaushofer K, Fratzl P. Collagen from the osteogenesis imperfecta mouse model (oim) shows reduced resistance against tensile stress. J Clin Invest. 1997;100:40–5.
Sims TJ, Miles CA, Bailey AJ, Camacho NP. Properties of collagen in OIM mouse tissues. Connect Tissue Res. 2003;44(Suppl 1):202–5.
Montpetit K, Plotkin H, Rauch F, Bilodeau N, Cloutier S, Rabzel M, et al. Rapid increase in grip force after start of pamidronate therapy in children and adolescents with severe osteogenesis imperfecta. Pediatrics. 2003;111:E601–3.
Hoggarth CR, Bennett R, Daley-Yates PT. The pharmacokinetics and distribution of pamidronate for a range of doses in the mouse. Calcif Tissue Int. 1991;49:416–20.
Hodges PW, Smeets RJ. Interaction between pain, movement, and physical activity: short-term benefits, long-term consequences, and targets for treatment. Clin J Pain. 2015;31:97–107.
•• Waning DL, Mohammad KS, Reiken S, Xie W, Andersson DC, John S, et al. Excess TGF-beta mediates muscle weakness associated with bone metastases in mice. Nat Med. 2015;21:1262–71. This is an experimental study demonstrating the adverse muscle effect of transforming growth factor beta released from bone.
Imel EA, Carpenter TO. A practical clinical approach to paediatric phosphate disorders. Endocr Dev. 2015;28:134–61.
Amanzadeh J, Reilly RF Jr. Hypophosphatemia: an evidence-based approach to its clinical consequences and management. Nat Clin Pract Nephrol. 2006;2:136–48.
Singhal PC, Kumar A, Desroches L, Gibbons N, Mattana J. Prevalence and predictors of rhabdomyolysis in patients with hypophosphatemia. Am J Med. 1992;92:458–64.
Veilleux LN, Cheung MS, Glorieux FH, Rauch F. The muscle-bone relationship in x-linked hypophosphatemic rickets. J Clin Endocrinol Metab. 2013;98:E990–5.
Thom JM, Morse CI, Birch KM, Narici MV. Triceps surae muscle power, volume, and quality in older versus younger healthy men. J Gerontol A Biol Sci Med Sci. 2005;60:1111–7.
Ducher G, Daly RM, Hill B, Eser P, Naughton GA, Gravenmaker KJ, et al. Relationship between indices of adiposity obtained by peripheral quantitative computed tomography and dual-energy X-ray absorptiometry in pre-pubertal children. Ann Hum Biol. 2009;36:705–16.
Farr JN, Funk JL, Chen Z, Lisse JR, Blew RM, Lee VR, et al. Skeletal muscle fat content is inversely associated with bone strength in young girls. J Bone Miner Res. 2011;26:2217–25.
Goodpaster BH, Kelley DE, Thaete FL, He J, Ross R. Skeletal muscle attenuation determined by computed tomography is associated with skeletal muscle lipid content. J Appl Physiol. 2000;89:104–10.
Finol H, De Venanzi F, Pereyra B, Alfonso C, Sanchez J. Effects of phosphorus deficiency on the ultrastructure of the rat fast twitch skeletal muscle. Interciencia. 2001;26:62–6.
Fuller TJ, Carter NW, Barcenas C, Knochel JP. Reversible changes of the muscle cell in experimental phosphorus deficiency. J Clin Invest. 1976;57:1019–24.
Whyte MP. Hypophosphatasia—aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol. 2016;12:233–46.
Phillips D, Case LE, Griffin D, Hamilton K, Lara SL, Leiro B, et al. Physical therapy management of infants and children with hypophosphatasia. Mol Genet Metab. 2016;119:14–9.
Weber TJ, Sawyer EK, Moseley S, Odrljin T, Kishnani PS. Burden of disease in adult patients with hypophosphatasia: results from two patient-reported surveys. Metabolism. 2016;65:1522–30.
Whyte MP, Madson KL, Phillips D, Reeves AL, McAlister WH, Yakimoski A, et al. Asfotase alfa therapy for children with hypophosphatasia. JCI Insight. 2016;1:e85971.
Janssens K, Vanhoenacker F, Bonduelle M, Verbruggen L, Van Maldergem L, Ralston S, et al. Camurati-Engelmann disease: review of the clinical, radiological, and molecular data of 24 families and implications for diagnosis and treatment. J Med Genet. 2006;43:1–11.
Ayyavoo A, Derraik JG, Cutfield WS, Hofman PL. Elimination of pain and improvement of exercise capacity in Camurati-Engelmann disease with losartan. J Clin Endocrinol Metab. 2014;99:3978–82.
Simsek-Kiper PO, Dikoglu E, Campos-Xavier B, Utine GE, Bonafe L, Unger S, et al. Positive effects of an angiotensin II type 1 receptor antagonist in Camurati-Engelmann disease: a single case observation. Am J Med Genet A. 2014;164a:2667–71.
Werkstetter KJ, Pozza SB, Filipiak-Pittroff B, Schatz SB, Prell C, Bufler P, et al. Long-term development of bone geometry and muscle in pediatric inflammatory bowel disease. Am J Gastroenterol. 2011;106:988–98.
Lee DY, Wetzsteon RJ, Zemel BS, Shults J, Organ JM, Foster BJ, et al. Muscle torque relative to cross-sectional area and the functional muscle-bone unit in children and adolescents with chronic disease. J Bone Miner Res. 2015;30:575–83.
Griffin LM, Thayu M, Baldassano RN, DeBoer MD, Zemel BS, Denburg MR, et al. Improvements in bone density and structure during anti-TNF-alpha therapy in pediatric Crohn’s disease. J Clin Endocrinol Metab. 2015;100:2630–9.
Oestreich AK, Carleton SM, Yao X, Gentry BA, Raw CE, Brown M, et al. Myostatin deficiency partially rescues the bone phenotype of osteogenesis imperfecta model mice. Osteoporos Int. 2016;27:161–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Louis-Nicolas Veilleux and Frank Rauch declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pediatrics
Rights and permissions
About this article
Cite this article
Veilleux, LN., Rauch, F. Muscle-Bone Interactions in Pediatric Bone Diseases. Curr Osteoporos Rep 15, 425–432 (2017). https://doi.org/10.1007/s11914-017-0396-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-017-0396-6