Abstract
For many years viral causes of community-acquired pneumonia were often been given limited attention. The number of published studies on influenza alone increased fivefold from 2001 to 2010. Specifically several studies have underlined that the involvement of viruses in community-acquired pneumonia has been underestimated, and this underestimation has been attributed to a lack of appropriate diagnostic methods. Now, with the advent of modern molecular assays, it is well recognized that viruses account for the largest proportion of community-acquired pneumonia in preschool children in both developed and developing countries. Respiratory syncytial virus, influenza virus, adenovirus, and parainfluenza virus are the major pathogens involved, but the relative importance of additional viruses (rhinoviruses, bocavirus, human metapneumovirus) is increasing and will be better defined by future research.
Similar content being viewed by others
Introduction
Pneumonia is the largest cause of death in children worldwide causing 1.396 million deaths and accounting for 18.3 % of total deaths in children younger than 5 years, especially in developing countries [1]. Despite the frequency, the causes of pneumonia are seldom identified in clinical practice and assessing the etiology of pneumonia is a complex issue since appropriate representative specimens can rarely be obtained and the sensitivity of blood cultures is generally low [2]. However, despite the obstacles to precise definition of the etiology, bacteria (e.g., Streptococcus pneumoniae, Haemophilus influenzae type b) have usually been considered as the major pathogens involved in community-acquired pneumonia (CAP) in children [3]. For many years limited attention was given to viral microorganisms involved in CAP, and viral etiologies were largely overlooked and underestimated. Recently the importance of viral etiological agents of pneumonia among pediatric patients has been brought to light, and the view of viral pneumonia has begun to change. Certainly the emergence of severe acute respiratory syndrome (SARS), avian influenza H5N1 and the pandemic swine influenza H1N1 virus have contributed to emphasizing the role of viruses as the cause of life-threatening pneumonia.
Viral Community-Acquired Pneumonia: A Diagnostic Challenge
If making the clinical and radiographic diagnosis of pneumonia is quite easy, assessing the specific viral etiology is harder, especially in clinical settings. The laboratory diagnosis of lower respiratory infections (LRTIs) poses different challenges [4]. The first challenge is how to obtain a representative sample of lower respiratory tract pathogens. Samples taken directly from the lungs through bronchoalveolar lavage and thoracentesis are ideally the best quality specimens to identify the pathogenic flora because they come from the site of infection and are less frequently contaminated; however, the procedure to obtain such samples is invasive and requires patient collaboration [5, 6]. Because of their poor applicability in clinical practice, especially in children, the tests are reserved for critically ill patients in whom standard treatments have failed. Samples taken from the upper respiratory tract through nasopharyngeal swabs or aspirates are certainly less invasive, but the detection of a virus in the nasopharynx might represent a coincidental upper respiratory infection instead of a pneumonia pathogen. However, considering that viral nasopharyngeal carriage in healthy children is considered to be rare, the finding of a respiratory virus in an upper airway sample could be considered as diagnostic for the etiology of LTRI. Certainly the lack of epidemiological studies regarding the prevalence and relevance of nasopharyngeal viral carriage in healthy children of various ages should be taken into consideration; filling this knowledge gap will help clarify the size of this diagnostic issue at a population level.
The second challenge is determining which method should be used to identify a virus from a microbiological sample. Diagnostic tests for viruses have been divided into three main categories: (1) direct examination of the sample (antigen detection, microscopy), (2) indirect tests (cell culture techniques and animal tests), and (3) serology. Usually the preferred method depends on the individual virus. For decades, specific antibody titers and viral culture were the only available tests for identification of a respiratory virus. Viral culture has been considered the “gold standard”, but this procedure has several limitations. Virus cultures are slow (up to 14 days to obtain a negative result) and no preliminary reports are generated. Moreover, the test outcome is closely related to the amount and viability of the viruses in the sample [7].
Later in the 1990s, a new era began in viral diagnostics. The introduction of molecular detection of viral genomes through highly sensitive nucleic acid amplification tests has improved diagnostic possibilities [8]. The polymerase chain reaction (PCR) is the best-known nucleic acid amplification test platform. PCR and related methods require less time (for both sample preparation and execution), and require less operator skill and training to carry out and provide opportunities for rapid diagnosis. The tests are highly specific, have the highest sensitivity compared to other diagnostic approaches and do not depend upon viral viability. Nevertheless, they have some limitations, such as vulnerability to contamination and inability to distinguish between viruses causing true disease and those which are merely colonized. Moreover, most PCR methods are expensive [9].
The last challenge is determining why infectious agents are still difficult to identify in a substantial proportion of respiratory samples from children with respiratory tract diseases despite the recent availability of sensitive diagnostic methods. This fact most likely suggests the existence of unknown respiratory pathogens that have not been previously considered. In fact, the second era in the discovery of respiratory viruses did not begin until the early 2000s. Several new respiratory viruses have been found: human metapneumovirus, coronavirus NL63 and HKU1, human bocavirus, and human rhinovirus C and D groups [10]. The contribution of these new viruses will be clarified over the next several years. Recently the discovery of a new enterovirus C-117 strain in a 45-month old girl hospitalized with CAP suggests that the viral impact of CAP is far from being completely defined, and the hypothesis that an unknown virus could be involved in disease pathogenesis is not so remote. In addition, this report suggested that a recombinant origin of the virus reactivated the virus's ability to combine and form new pathogenic variants [11••].
Despite all these critical points, efforts should be made to make an accurate and timely diagnosis of the cause of LTRI in children because of the potential benefits including improved treatment of the child, decreasing the cost of care and reducing selection for multidrug-resistant pathogens due to excessive and inappropriate antibiotic use.
Epidemiology of Viral Community-Acquired Pneumonia in Children
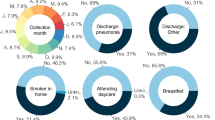
Studies investigating the etiology of childhood CAP have been performed in populations of various ages (infant, children and adolescent), in various settings (industrialized and developing countries), and with differing health conditions (healthy and immunocompromised patients). They have also been performed with the use of a variety of microbiological techniques (molecular assays, serology, culture) and sample collection methods (nasopharyngeal swabs and aspirates, expectorated and induced sputum, bronchoalveolar lavage and lung puncture). The variables have highly influenced the microbial findings. Despite these limits, some consistent trends and conclusions have been identified regarding the etiology of CAP in children. Firstly, after the introduction of PCR, viruses have been recognized to be the most common cause of CAP in young children, especially in those younger than 2 years [12]. The incidence of a viral etiology tends to decrease with age, and the incidence of a bacterial etiology tends to remain stable or increase slightly with age [13, 14••]. Secondly, respiratory syncytial virus (RSV) has been identified as the largest single pathogen leading to hospitalization for CAP in both developed and developing countries in infants and preschool children [15]. We analyzed in more detail the impact of viral infection in CAP in children and critically reviewed data coming from industrialized and developing countries.
Industrialized Countries
The annual incidence of pneumonia in children younger than 5 years is 34 to 40 cases per 1,000 population in Europe and North America, which is higher than at any other period of life, except perhaps in the elderly [16]. In developed countries the burden of pneumonia is large. This disease is responsible for a high rate of hospitalization, high medical expenditure (drugs and medical assistance) and indirect costs (lost work and productivity) [17–19]. In the USA, the Centers for Disease Control and Prevention monitors pneumonia hospitalizations using data from the Nationwide Inpatient Sample. In 2005/2006 the rates of all-cause pneumonia hospitalization per 1,000 children younger than 2 years were 9 % in 2005 and 8 % in 2006 [17]. In the USA alone, the economic burden of CAP has been estimated to be more than $17 billion annually in the adult population and $1,464 per episode in children [18, 19]. The mean cost for patients requiring hospitalization is $12,000 per episode [19]. Indirect costs (lost work and productivity) attributed to pneumonia are significant: parental days of work lost range from 2 days for CAP treated in the ambulatory setting to 4 days for CAP requiring hospitalization [19].
Virus have been most commonly associated with pneumonia in young infants (up to 83 % in children younger than 18 months), with the predominance of RSV, followed by influenza A and B and parainfluenza viruses types 1, 2 and 3, and adenovirus [20, 21]. The exact percentage contribution from each virus depends on the age of the children recruited, and the method used in virus detection (PCR has increased detection of rhinovirus and enteroviruses) [14]. Also, the season influences study results and should not be neglected. Indeed, respiratory viruses usually follow seasonal patterns of activity causing disease during times of activity especially in temperate climates. This is particularly true for influenza virus whose winter seasonality in temperate climates is one of the most widely recognized patterns [22].
The impact of rhinovirus in children with CAP has recently come to light after the introduction of PCR for respiratory viral screening. Rhinoviruses are certainly the most common cause of the common cold, and have been associated with different infections of the upper respiratory tract, such as otitis media and sinusitis [23]. Furthermore, the high prevalence of rhinovirus in hospitalized children with LTRIs has also been documented recently. Rhinovirus RNA has been detected in 45 % of school-age children (5–14 years of age) through nasopharyngeal washes [24]. An age-specific distribution has been reported by Esposito et al. [25•]. Rhinovirus was found in 36 % of children aged <1 year, in 27 % of children aged 1–3 years and in 26 % of children aged ≥4 years with radiographically confirmed CAP. Rhinovirus type A was the strain most frequently associated with the disease [25•]. These studies have clearly shown that the association between rhinoviruses and LRTIs is significantly more frequent than previously thought, and that rhinovirus CAP is frequent, not only in younger, but also in older children.
With regard to the six newly described viruses associated with respiratory infection (human metapneumovirus, SARS coronavirus, human coronavirus NL63 and HKU1, parainfluenza 4, and bocavirus), an increasing number of studies have been published in recent years [26]. High detection rates of human metapneumovirus (range 4.9–8.3 %) and human bocavirus (range 2.9–18 %) have been found in children with CAP [20, 21, 27–32].
An epidemiological aspect that should not be neglected is the presence of a mixed microbial etiology (e.g., viral/bacterial) or combined etiology (e.g., viral/viral). A better definition of the true incidence of these infections is partly derived from recent advances in diagnostic methods [33]. Studies suggested that mixed infections are very common (35 %) with at least one pathogen involved. The majority of mixed infections are mixed viral/bacterial infections [13, 25•]. Indeed, a viral infection that appears either concurrently or immediately before a bacterial infection is able to augment the bacterial colonization into a superinfection. Mixed viral/bacterial infections are especially common in younger children (younger than 2 years) probably as a result of the high frequency of RSV infections and their tendency to induce bacterial coinfections.
The most common combination infection is S. pneumoniae with one of a variety of respiratory viruses. This was recently highlighted by the pandemic H1N1 virus [34]. However, whereas the relevance of bacterial and viral coinfections is well known, information on viral coinfections is not well defined. Multiple viral infections are more prevalent during the first three years of life [33]. Human bocavirus has been associated with the highest percentage of coinfection, followed by adenovirus and rhinovirus [20, 35]. The clinical implication of mixed microbial infections remains largely unresolved, and the association with more severe disease and treatment failure is uncertain [21, 28].
Middle and Low-Income Countries
The incidence rates of pneumonia in developing countries are up to ten times greater than in industrialized countries. Three quarters of all pneumonia episodes worldwide among children younger than 5 years occur in just 15 countries (India, China, Nigeria, Pakistan, Bangladesh, Indonesia, Brazil, Ethiopia, Congo, Philippines, Afghanistan, Egypt, Mexico, Sudan, Vietnam), which have huge barriers to health-care access, and are plagued with malnutrition [36]. South-East Asia and sub-Saharan Africa together bear the burden of more than half the total number of pneumonia episodes worldwide [36].
There are very few studies on the incidence of viral CAP in developing countries, probably due to the paucity of modern diagnostic molecular techniques. Data available show that viral agents play an important role in acute LTRIs. Viral detection rates in pediatric CAP show a very large variation (up to 77 %) with a mean of 40 %. RSV is the most frequent etiological agent identified, especially in children younger than 2 years. Other viruses such as influenza A and B, parainfluenza and adenovirus are also frequently identified.
In Africa, few studies have been performed in children hospitalized with LTRIs. In Ghana, 26 % of hospitalized children aged 6–24 months had a viral CAP. RSV was the predominant virus isolated (14 %), followed by adenoviruses (10 %), parainfluenza types 1, 2 and 3 (3 %), and influenza B viruses (1 %) [37]. In Burundi, rhinovirus is frequently detected in children aged 1 month to 14 years with LTRIs. Rhinovirus type A seems to be the most important species and is identified mainly in patients with CAP [38]. Rhinovirus was also the predominant virus detected in a rural area of Madagascar in children aged 2–59 months [39]. Viral pathogens also predominated in severe CAP in children younger than 5 years in South Africa and Kenya, with RSV being the most common pathogen isolated [40–42].
In tropical countries (Southeast Asian countries) available data indicate that more than about one-third of LTRIs are due to viruses [43–45]. In Cambodia the great majority of hospitalized children younger than 5 years with LTRI have a viral infection; rhinovirus and RSV are the principal viral pathogens isolated. A single virus was detected in 89 % of patients while infections with multiple viruses were detected in 6 % [46]. Similar results were obtained in a study in young children younger than 3 years living in a rural community in Bangladesh where 45 % of nasopharyngeal aspirates were positive for viral agents, and RSV was the predominant pathogen (81 %) [47]. However, more recently Homaira et al. found an increased prevalence (77 %) of viral CAP in children younger than 2 years with an overall incidence of pneumonia associated with a respiratory virus infection of 40/100 child-years. The annual incidences of pneumonia/100 child-years associated with specific respiratory viruses were 12.5 for RSV, 6 for rhinoviruses, 6 for human metapneumovirus, 4 for influenza viruses, 3 for parainfluenza viruses and 2 for adenoviruses [48••].
In Brazil, viral infection was found in 60 % of children younger than 5 years hospitalized for CAP, and was more frequent than bacterial infection. A sole viral infection was identified in 36 % of patients, and mixed viral/bacterial infections in 23 % of children with CAP [49]. To identify specific viruses, Nascimento-Carvalho et al. analyzed blood samples and nasopharyngeal aspirates using PCR assay and virus-specific serum antibody titers. Rhinovirus was the most frequent viral agent detected followed by parainfluenza virus.
In Mexico, Noyola et al. found that in children younger than 15 years admitted with a diagnosis of LTRIs, viruses were responsible for at least 47 % of cases, with RSV as the most common pathogen (86 %) [50]. However, the high detection rate of RSV was influenced by the high percentage of children younger than 1 year included in this study.
The contribution of recently identified respiratory viruses, such as human metapneumovirus, human bocavirus and human coronavirus, to CAP etiology in developing countries needs to be clarified. Few studies have examined the role of these microorganisms in the pathogenesis of CAP. In a rural community in Senegal, metapneumovirus was not detected in children younger than 5 years, probably due to the small number of children with LTRI examined [51]. In Madagascar, metapneumovirus and coronaviruses were isolated from 14 % and 12 % of children with CAP, respectively [39]. A larger epidemiological studies that provided more comprehensive data on new, unidentified viruses in very young children (younger than 2 years) with CAP was performed in Bangladesh [48••]. In this study, human metapneumovirus was individually detected in 9 % of episodes of pneumonia. Human bocavirus accounted for 12 % of all pneumonia episodes requiring hospitalization in Thai children younger than 5 years [52••]. In Brazil, primary human bocavirus infection was diagnosed in 8 % of children (median age 16 months) and metapneumovirus in 4 % of children younger than 5 years hospitalized with CAP [53, 54].
Etiological data coming from middle-income and low-income countries are difficult to compare due to variability in the tests used for identification, and the frequency of etiological agents, which depends on a number of factors, such as differences in case definition across studies, the types of sample collected for each laboratory test, the methods used in microbiological analysis, and the ages of the patients. Moreover, the health status (malnutrition and HIV status) of the patients can affect study results, and contribute to the variability of the results. Finally, geography and season are other factors that need to be considered. In tropical countries, the correlation between respiratory viral activity and climatic factors is not so well defined, which may suggest that more complex interactions are involved. Rainfall and drought can affect virus circulation, but currently there are no studies that exactly define the seasonality of the respiratory viruses in these countries.
Conclusions
Viruses have gained attention as important causes of CAP in childhood, both in industrialized and in middle-income and low-income countries. Probably a wider variety of new unidentified viruses will also be implicated in viral pneumonia in the next few years, increasing the public health burden of this disease. Despite the availability of molecular assays, there is a need for new and cost-effective diagnostic strategies, especially for populations living in areas where access to primary health care is more difficult.
Better surveillance to monitor the etiology is necessary to improve children’s health and rationalize the use of antimicrobial agents. Further research should focus on the development of effective antiviral drugs and modulation of host immune responses to reduce the human and economic burden of childhood CAP.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. Pneumonia. Fact sheet no. 331, November 2012. Geneva: World Health Organization. Available from: http://www.who.int/mediacentre/factsheets/fs331/en/index.html.
Hammitt LL, Murdoch DR, Scott JA, et al. Pneumonia Methods Working Group. Specimen collection for the diagnosis of pediatric pneumonia. Clin Infect Dis. 2012;54 Suppl 2:S132–9.
Stein RT, Marostica PJ. Community-acquired pneumonia: a review and recent advances. Pediatr Pulmonol. 2007;42:1095–103.
Carroll KC. Laboratory diagnosis of lower respiratory tract infections: controversy and conundrums. J Clin Microbiol. 2002;40:3115–20.
Vuori-Holopainen E, Salo E, Saxén H, et al. Etiological diagnosis of childhood pneumonia by use of transthoracic needle aspiration and modern microbiological methods. Clin Infect Dis. 2002;34:583–90.
Baselski VS, Wunderink RG. Bronchoscopic diagnosis of pneumonia. Clin Microbiol Rev. 1994;7:533–58.
Leland DS, Ginocchio CC. Role of cell culture for virus detection in the age of technology. Clin Microbiol Rev. 2007;20:49–78.
Saranglao A, Smith PR. Diagnostic tests for CAP: current approaches and future perspectives. Expert Rev Mol Diagn. 2002;2:329–36.
Mahony JB. Detection of respiratory viruses by molecular methods. Clin Microbiol Rev. 2008;21:716–47.
Jartti T, Jartti L, Ruuskanen O, Söderlund-Venermo M. New respiratory viral infections. Curr Opin Pulm Med. 2012;18:271–8.
•• Daleno C, Piralla A, Scala A, et al. Complete genome sequence of a novel human enterovirus C (HEV-C117) identified in a child with community-acquired pneumonia. J Virol. 2012;86:10888–9. This study showed that a new entorovirus is implicated in CAP etiology.
Don M, Canciani M, Korppi M. Community-acquired pneumonia in children: what's old? What's new? Acta Paediatr. 2010;99:1602–8.
Juvén T, Mertsola J, Waris M, et al. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19:293–8.
•• Ruuskanen O, Lahti E, Jennings LC, Murdoch DR. Viral pneumonia. Lancet. 2011;377:1264–75. An excellent review of this topic from a clinical perspective.
Sinaniotis CA. Viral pneumoniae in children: incidence and aetiology. Paediatr Respir Rev. 2004;5(Suppl A):S197–200.
McIntosh K. Community-acquired pneumonia in children. N Engl J Med. 2002;346:429–37.
Centers for Disease Control and Prevention (CDC). Pneumonia hospitalizations among young children before and after introduction of pneumococcal conjugate vaccine – United States, 1997-2006. MMWR Morb Mortal Wkly Rep. 2009;58:1–4.
File Jr TM, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;22:130–41.
Bradley JS, Byington CL, Shah SS, et al. Executive summary: the management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:617–30.
García-García ML, Calvo C, Pozo F, et al. Spectrum of respiratory viruses in children with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31:808–13.
Honkinen M, Lahti E, Österback R, et al. Viruses and bacteria in sputum samples of children with community-acquired pneumonia. Clin Microbiol Infect. 2012;18:300–7.
Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3:1470–6.
Papadopoulos NG. Do rhinoviruses cause pneumonia in children? Paediatr Respir Rev. 2004; Suppl A:S191–S5.
Tsolia MN, Psarras S, Bossios A, et al. Etiology of community-acquired pneumonia in hospitalized school-age children: evidence for high prevalence of viral infections. Clin Infect Dis. 2004;39:681–6.
• Esposito S, Daleno C, Tagliabue C, et al. Impact of rhinoviruses on pediatric community-acquired pneumonia. Eur J Clin Microbiol Infect Dis. 2012;31:1637–45. This study highlights the importance of rhinovirus on childhood community acquired pneumonia.
Pavia AT. Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis. 2011;52 Suppl 4:S284–9.
Wolf DG, Greenberg D, Shemer-Avni Y, et al. Association of human metapneumovirus with radiologically diagnosed community-acquired alveolar pneumonia in young children. J Pediatr. 2010;156:115–20.
Esposito S, Daleno C, Prunotto G, et al. Impact of viral infections in children with community-acquired pneumonia: results of a study of 17 respiratory viruses. Influenza Other Respi Viruses. 2013;7:18–26.
Don M, Korppi M, Valent F, et al. Human metapneumovirus pneumonia in children: results of an Italian study and mini-review. Scand J Infect Dis. 2008;40:821–6.
Don M, Fasoli L, Paldanius M, et al. Aetiology of community-acquired pneumonia: serological results of a paediatric survey. Scand J Infect Dis. 2005;37:806–12.
Lin PY, Lin TY, Huang YC, et al. Human metapneumovirus and community-acquired pneumonia in children. Chang Gung Med J. 2005;28:683–8.
Hamano-Hasegawa K, Morozumi M, Nakayama E, et al. Acute Respiratory Diseases Study Group. Comprehensive detection of causative pathogens using real-time PCR to diagnose pediatric community-acquired pneumonia. J Infect Chemother. 2008;14:424–32.
Korppi M. Mixed microbial aetiology of community-acquired pneumonia in children. APMIS. 2002;110:515–22.
Yazer J, Giacomantonio M, Macdonald N, Lopushinsky S. Severe necrotizing pneumonia in a child with pandemic (H1N1) influenza. CMAJ. 2011;183:215–9.
Ray C, Holberg C, Minnich L, et al. Acute lower respiratory illnesses during the first three years of life: potential roles for various etiologic agents. Pediatr Infect Dis J. 1993;12:104.
Wardlaw TM, Johansson E, Hodge M, World Health Organization, UNICEF. Pneumonia: The forgotten killer of children. Geneva: World Health Organization; 2006.
Kwofie TB, Anane YA, Nkrumah B, et al. Respiratory viruses in children hospitalized for acute lower respiratory tract infection in Ghana. Virol J. 2012;9:78.
Esposito S, Daleno C, Baggi E, et al. Circulation of different rhinovirus groups among children with lower respiratory tract infection in Kiremba, Burundi. Eur J Clin Microbiol Infect Dis. 2012;31:3251–6.
Hoffmann J, Rabezanahary H, Randriamarotia M, et al. Viral and atypical bacterial etiology of acute respiratory infections in children under 5 years old living in a rural tropical area of Madagascar. PLoS One. 2012;7:e43666.
Delport SD, Brisley T. Aetiology and outcome of severe community-acquired pneumonia in children admitted to a paediatric intensive care unit. S Afr Med J. 2002;92:907–11.
Berkley JA, Munywoki P, Ngama M, et al. Viral etiology of severe pneumonia among Kenyan infants and children. JAMA. 2010;303:2051–7.
Hammitt LL, Kazungu S, Morpeth SC, et al. A preliminary study of pneumonia etiology among hospitalized children in Kenya. Clin Infect Dis. 2012;54 Suppl 2:S190–9.
Sung RY, Chan RC, Tam JS, et al. Epidemiology and aetiology of acute bronchiolitis in Hong Kong infants. Epidemiol Infect. 1992;108:147–54.
Sung CC, Chi H, Chiu NC, et al. Viral etiology of acute lower respiratory tract infections in hospitalized young children in Northern Taiwan. J Microbiol Immunol Infect. 2011;44:184–90.
Ekalaksananan T, Pientong C, Kongyingyoes B, et al. Etiology of acute lower respiratory tract infection in children at Srinagarind Hospital, Khon Kaen, Thailand. Southeast Asian J Trop Med Public Health. 2003;32:513–9.
Guerrier G, Goyet S, Chheng ET, et al. Acute viral lower respiratory tract infections in Cambodian children: clinical and epidemiological characteristics. Pediatr Infect Dis J. 2013;32:e8–13.
Hasan K, Jolly P, Marquis G, et al. Viral etiology of pneumonia in a cohort of newborns till 24 months of age in Rural Mirzapur, Bangladesh. Scand J Infect Dis. 2006;38:690–5.
•• Homaira N, Luby SP, Petri WA, et al. Incidence of respiratory virus-associated pneumonia in urban poor young children of Dhaka, Bangladesh, 2009–2011. PLoS One. 2012;7:e32056. This study showed the importance of RSV in CAP etiology in Bangladesh.
Nascimento-Carvalho CM, Ribeiro CT, Cardoso MR, et al. The role of respiratory viral infections among children hospitalized for community-acquired pneumonia in a developing country. Pediatr Infect Dis J. 2008;27:939–41.
Noyola DE, Rodríguez-Moreno G, Sánchez-Alvarado J, et al. Viral etiology of lower respiratory tract infections in hospitalized children in Mexico. Pediatr Infect Dis J. 2004;23:118–23.
Niang MN, Diop OM, Sarr FD, et al. Viral etiology of respiratory infections in children under 5 years old living in tropical rural areas of Senegal: The EVIRA project. J Med Virol. 2010;82:866–72.
•• Fry AM, Lu X, Chittaganpitch M, et al. Human bocavirus: a novel parvovirus epidemiologically associated with pneumonia requiring hospitalization in Thailand. J Infect Dis. 2007;195:1038–45. This study showed that human bocavirus is epidemiologically associated with community-acquired pneumonia.
Nascimento-Carvalho CM, Cardoso MR, Meriluoto M, et al. Human bocavirus infection diagnosed serologically among children admitted to hospital with community-acquired pneumonia in a tropical region. J Med Virol. 2012;84:253–8.
Nascimento-Carvalho CM, Cardoso MR, Ruuskanen O, et al. Sole infection by human metapneumovirus among children with radiographically diagnosed community-acquired pneumonia in a tropical region. Influenza Other Respi Viruses. 2011;5:285–7.
Conflict of Interest
Chiara Mameli declares that she has no conflict of interest.
Gian Vincenzo Zuccotti declares that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mameli, C., Zuccotti, G.V. The Impact of Viral Infections in Children with Community-Acquired Pneumonia. Curr Infect Dis Rep 15, 197–202 (2013). https://doi.org/10.1007/s11908-013-0339-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-013-0339-z