Abstract
Purpose of Review
Steroid profiling and immunohistochemistry are both promising new tools used to improve diagnostic accuracy in the work-up of primary aldosteronism (PA) and to predict treatment outcomes. Herein, we review the recent literature and present an outlook to the future of diagnostics and therapeutic decision-making in patients with PA.
Recent Finding
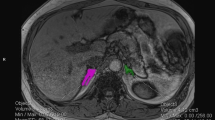
PA is the most common endocrine cause of arterial hypertension and unilateral forms of the disease are potentially curable by surgical resection of the overactive adrenal. Recent studies have shown that adrenal steroid profiling by liquid chromatography-tandem mass spectrometry (LC-MS/MS) can be helpful for subtyping unilateral and bilateral forms of PA, classifying patients with a unilateral aldosterone-producing adenoma (APA) according to the presence of driver mutations of aldosterone production in APAs, and potentially predicting the outcomes of surgical treatment for unilateral PA. Following adrenalectomy, immunohistochemistry of aldosterone synthase (CYP11B2) in resected adrenals is a new tool to analyze “functional” histopathology and may be an indicator of biochemical outcomes after surgery.
Summary
Biochemical and clinical outcomes of therapy in PA vary widely among patients. Peripheral venous steroid profiling at baseline could improve diagnostic accuracy and help in surgical decision-making in cases of a suspected APA; results of “functional” histopathology could help determine which patients are likely to need close post-surgical follow-up for persistent aldosteronism.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Conn JW, Part I. Painting background. Part II. Primary aldosteronism, a new clinical syndrome, 1954. J Lab Clin Med. 1990;116(2):253–67.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(5):1889–916.
Stowasser M, Gordon RD, Gunasekera TG, Cowley DC, Ward G, Archibald C, et al. High rate of detection of primary aldosteronism, including surgically treatable forms, after ‘non-selective’ screening of hypertensive patients. J Hypertens. 2003;21(11):2149–57.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48(11):2293–300.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6(1):41–50.
Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, et al. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension. 2013;62(1):62–9.
Rossi GP, Maiolino G, Flego A, Belfiore A, Bernini G, Fabris B, et al. Adrenalectomy lowers incident atrial fibrillation in primary aldosteronism patients at long term. Hypertension. 2018;71(4):585–91.
•• Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(1):51–9. This study is very important because it reveales that PA is associated with cardiovascular morbidity and mortality independent of elevated blood pressure.
Sukor N, Kogovsek C, Gordon RD, Robson D, Stowasser M. Improved quality of life, blood pressure, and biochemical status following laparoscopic adrenalectomy for unilateral primary aldosteronism. J Clin Endocrinol Metab. 2010;95(3):1360–4.
•• Williams TA, JWM L, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Primary Aldosteronism Surgery Outcome (PASO) investigators. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5(9):689–99. This article is very important because it consists of an international consensus defining biochemical and clinical outcomes in PA, which had not been universally defined previously.
Muth A, Ragnarsson O, Johannsson G, Wängberg B. Systematic review of surgery and outcomes in patients with primary aldosteronism. Br J Surg. 2015;102(4):307–17.
Steichen O, Zinzindohoué F, Plouin PF, Amar L. Outcomes of adrenalectomy in patients with unilateral primary aldosteronism: a review. Horm Metab Res. 2012;44(3):221–7.
• Williams TA, Burrello J, Sechi LA, Fardella CE, Matrozova J, Adolf C, et al. Computed tomography and adrenal venous sampling in the diagnosis of unilateral primary aldosteronism. Hypertension. 2018;72(3):641–9. This study is Important because it uses outcome data from 18 international centers comparing the value of CT and AVS in the diagnosis and for outcome in PA and shows that adrenalectomy based on AVS results in a higher likelihood of biochemical cure than CT based adrenalectomy.
Dekkers T, Prejbisz A, Kool LJS, Groenewoud HJMM, Velema M, Spiering W, et al. Adrenal vein sampling versus CT scan to determine treatment in primary aldosteronism: an outcome-based randomised diagnostic trial. Lancet Diabetes Endocrinol. 2016;4(9):739–46.
• Meyer LS, Wang X, Sušnik E, Burrello J, Burrello A, Castellano I, et al. Immunohistopathology and steroid profiles associated with biochemical outcomes after adrenalectomy for unilateral primary aldosteronism. Hypertension. 2018;72(3):650–7. This study is essential because it relates to the main topic of this review analyzing the value of steroid profiling and immunohistopathology for outcome prediction (including 97 adrenals from 9 international studies).
Stowasser M, Gordon RD. Primary aldosteronism: changing definitions and new concepts of physiology and pathophysiology both inside and outside the kidney. Physiol Rev. 2016;96(4):1327–84.
Williams TA, Reincke M. Management of endocrine disease: diagnosis and management of primary aldosteronism: the Endocrine Society guideline 2016 revisited. Eur J Endocrinol. 2018;179(1):R19–29.
Nishimoto K, Koga M, Seki T, Oki K, Gomez-Sanchez EP, Gomez-Sanchez CE, et al. Immunohistochemistry of aldosterone synthase leads the way to the pathogenesis of primary aldosteronism. Mol Cell Endocrinol. 2017;441:124–33.
Nakamura Y, Kitada M, Satoh F, Maekawa T, Morimoto R, Yamazaki Y, et al. Intratumoral heterogeneity of steroidogenesis in aldosterone-producing adenoma revealed by intensive double- and triple-immunostaining for CYP11B2/B1 and CYP17. Mol Cell Endocrinol. 2016;422:57–63.
• Nanba K, Vaidya A, Williams GH, Zheng I, Else T, Rainey WE. Age-related autonomous aldosteronism. Circulation. 2017;136(4):347–55. This study is important because it adds to the knowledge we have about APCCs, one important immunohistopathological finding that – as we know from this study - increases with age.
Nishimoto K, Tomlins SA, Kuick R, Cani AK, Giordano TJ, Hovelson DH, et al. Aldosterone-stimulating somatic gene mutations are common in normal adrenal glands. Proc Natl Acad Sci. 2015;112(33):E4591–9.
Nishimoto K, Seki T, Kurihara I, Yokota K, Omura M, Nishikawa T, et al. Case report: nodule development from subcapsular aldosterone-producing cell clusters causes hyperaldosteronism. J Clin Endocrinol Metab. 2016;101(1):6–9.
Nishimoto K, Nakagawa K, Li D, Kosaka T, Oya M, Mikami S, et al. Adrenocortical zonation in humans under normal and pathological conditions. J Clin Endocrinol Metab. 2010;95(5):2296–305.
• Arlt W, Lang K, Sitch AJ, Dietz AS, Rhayem Y, Bancos I, et al. Steroid metabolome analysis reveals prevalent glucocorticoid excess in primary aldosteronism. JCI Insight. 2017;2(8). This study is important because it uses steroid profiling and reveals prevalent glucocorticoid synthesis in PA, which was not known to this extent previously.
•• Williams TA, Peitzsch M, Dietz AS, Dekkers T, Bidlingmaier M, Riester A, et al. Genotype-specific steroid profiles associated with aldosterone-producing adenomas. Hypertension. 2016;67(1):139–45. This study is very important because it analyzes and reveals that steroid profiles are specific for certain driver mutations in APAs, very relevant for this review.
Mulatero P, Curnow K, Aupetit-Faisant B, Foekling M, Gomez-Sanchez C, Veglio F, et al. Recombinant CYP11B genes encode enzymes that can catalyze conversion of 11-deoxycortisol to cortisol, 18-hydroxycortisol, and 18-oxocortisol. J Clin Endocrinol Metab. 1998;83(11):3996–4001.
Lenders JWM, Williams TA, Reincke M, Gomez-Sanchez CE. Diagnosis of endocrine disease: 18-oxocortisol and 18-hydroxycortisol: is there clinical utility of these steroids? Eur J Endocrinol. 2018;178(1):R1–9.
Gomez-Sanchez CE, Qi X, Gomez-Sanchez EP, Sasano H, Bohlen MO, Wisgerhof M. Disordered zonal and cellular CYP11B2 enzyme expression in familial hyperaldosteronism type 3. Mol Cell Endocrinol. 2017;439:74–80.
Azizan EAB, Lam BYH, Newhouse SJ, Zhou J, Kuc RE, Clarke J, et al. Microarray, qPCR, and KCNJ5 sequencing of aldosterone-producing adenomas reveal differences in genotype and phenotype between zona glomerulosa- and zona fasciculata-like tumors. J Clin Endocrinol Metab. 2012;97(5):E819–29.
Monticone S, Castellano I, Versace K, Lucatello B, Veglio F, Gomez-Sanchez CE, et al. Immunohistochemical, genetic and clinical characterization of sporadic aldosterone-producing adenomas. Mol Cell Endocrinol. 2015;411:146–54.
Geller DS, Zhang J, Wisgerhof MV, Shackleton C, Kashgarian M, Lifton RP. A novel form of human mendelian hypertension featuring nonglucocorticoid-remediable aldosteronism. J Clin Endocrinol Metab. 2008;93(8):3117–23.
Fischer E, Beuschlein F, Bidlingmaier M, Reincke M. Commentary on the Endocrine Society practice guidelines: consequences of adjustment of antihypertensive medication in screening of primary aldosteronism. Rev Endocr Metab Disord. 2011;12(1):43–8.
Li Q, Song Y, Yang S, Zhang A. Diagnostic accuracy of three confirmatory tests for primary aldosteronism: a prospective study and systematic review. Endocr Abstr. 2017.
Song Y, Yang S, He W, Hu J, Cheng Q, Wang Y, et al. Confirmatory tests for the diagnosis of primary aldosteronism. Hypertension. 2018;71(1):118–24.
Schirpenbach C, Seiler L, Maser-Gluth C, Rüdiger F, Nickel C, Beuschlein F, et al. Confirmatory testing in normokalaemic primary aldosteronism: the value of the saline infusion test and urinary aldosterone metabolites. Eur J Endocrinol. 2006;154(6):865–73.
Kempers MJE, Lenders JWM, van Outheusden L, van der Wilt GJ, Schultze Kool LJ, Hermus ARMM, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med. 2009;151(5):329–37.
Deinum J, Prejbisz A, Lenders JW, van der Wilt GJ. Adrenal vein sampling is the preferred method to select patients with primary aldosteronism for adrenalectomy: con side of the argument. Hypertension. 2018;71(1):10–4.
Rossi GP, Funder JW. Adrenal vein sampling is the preferred method to select patients with primary aldosteronism for adrenalectomy: pro side of the argument. Hypertension. 2018;71(1):5–9.
Lim V, Guo Q, Grant CS, Thompson GB, Richards ML, Farley DR, et al. Accuracy of adrenal imaging and adrenal venous sampling in predicting surgical cure of primary aldosteronism. J Clin Endocrinol Metab. 2014;99(8):2712–9.
Ladurner R, Sommerey S, Buechner S, Dietz A, Degenhart C, Hallfeldt K, et al. Accuracy of adrenal imaging and adrenal venous sampling in diagnosing unilateral primary aldosteronism. Eur J Clin Investig. 2017;47(5):372–7.
Rossi GP, Auchus RJ, Brown M, Lenders JW, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63(1):151–60.
Fujii Y, on behalf of W-JSG, Umakoshi H, Wada N, Ichijo T, Kamemura K, et al. Subtype prediction of primary aldosteronism by combining aldosterone concentrations in the left adrenal vein and inferior vena cava: a multicenter collaborative study on adrenal venous sampling. J Hum Hypertens. 2017;32(1):12–9.
Lubitz CC, Economopoulos KP, Sy S, Johanson C, Kunzel HE, Reincke M, et al. Cost-effectiveness of screening for primary aldosteronism and subtype diagnosis in the resistant hypertensive patients. Circ Cardiovasc Qual Outcomes. 2015;8(6):621–30.
Rossi GP, Barisa M, Allolio B, Auchus RJ, Amar L, Cohen D, et al. The Adrenal Vein Sampling International Study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012;97(5):1606–14.
Monticone S, Satoh F, Dietz AS, Goupil R, Lang K, Pizzolo F, et al. Clinical management and outcomes of adrenal hemorrhage following adrenal vein sampling in primary aldosteronism. Hypertension. 2016;67(1):146–52.
Vonend O, Ockenfels N, Gao X, Allolio B, Lang K, Mai K, et al. Adrenal venous sampling: evaluation of the German Conn’s registry. Hypertension. 2011;57(5):990–5.
Lenders JWM, Eisenhofer G, Reincke M. Subtyping of patients with primary aldosteronism: an update. Horm Metab Res. 2017;49(12):922–8.
Naruse M, Umakoshi H, Tsuiki M, Yokomoto M, Tagami T, Tanabe A, et al. The latest developments of functional molecular imaging in the diagnosis of primary aldosteronism. Horm Metab Res. 2017;49(12):929–35.
Hahner S, Kreissl MC, Fassnacht M, Haenscheid H, Bock S, Verburg FA, et al. Functional characterization of adrenal lesions using [123I]IMTO-SPECT/CT. J Clin Endocrinol Metab. 2013;98(4):1508–18.
Burton TJ, Mackenzie IS, Balan K, Koo B, Bird N, Soloviev DV, et al. Evaluation of the sensitivity and specificity of (11)C-metomidate positron emission tomography (PET)-CT for lateralizing aldosterone secretion by Conn’s adenomas. J Clin Endocrinol Metab. 2012;97(1):100–9.
Abe T, Naruse M, Young WF Jr, Kobashi N, Doi Y, Izawa A, et al. A novel CYP11B2-specific imaging agent for detection of unilateral subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2016;101(3):1008–15.
Bergström M, Bonasera TA, Lu L, Bergström E, Backlin C, Juhlin C, et al. In vitro and in vivo primate evaluation of carbon-11-etomidate and carbon-11-metomidate as potential tracers for PET imaging of the adrenal cortex and its tumors. J Nucl Med. 1998;39(6):982–9.
Gross MD, Shapiro B, Kloos RT, Dwamena B. PET imaging of adrenal cortical tumors with the 11ß-hydroxylase tracer 11C-metomidate. J Nucl Med. 2000;41(11):1933–4.
Zettinig G, Mitterhauser M, Wadsak W, Becherer A, Pirich C, Vierhapper H, et al. Positron emission tomography imaging of adrenal masses: 18 F-fluorodeoxyglucose and the 11β-hydroxylase tracer 11 C-metomidate. Eur J Nucl Med Mol Imaging. 2004;31(9):1224–30.
Hahner S, Stuermer A, Kreissl M, Reiners C, Fassnacht M, Haenscheid H, et al. [123I] Iodometomidate for molecular imaging of adrenocortical cytochrome P450 family 11B enzymes. J Clin Endocrinol Metab. 2008;93(6):2358–65.
Burton TJ, Mackenzie IS, Balan K, Koo B, Bird N, Soloviev DV, et al. Evaluation of the sensitivity and specificity of 11C-metomidate positron emission tomography (PET)-CT for lateralizing aldosterone secretion by Conn’s adenomas. J Clin Endocrinol Metab. 2012;97(1):100–9.
Bongarzone S, Basagni F, Sementa T, Singh N, Gakpetor C, Faugeras V, et al. Development of [18F] FAMTO: a novel fluorine-18 labelled positron emission tomography (PET) radiotracer for imaging CYP11B1 and CYP11B2 enzymes in adrenal glands. Nucl Med Biol. 2019;68:14–21.
Hennings J, Sundin A, Hägg A, Hellman P. 11 C-metomidate positron emission tomography after dexamethasone suppression for detection of small adrenocortical adenomas in primary aldosteronism. Langenbeck's Arch Surg. 2010;395(7):963–7.
Bluemel C, Hahner S, Heinze B, Fassnacht M, Kroiss M, Bley TA, et al. Investigating the chemokine receptor 4 as potential theranostic target in adrenocortical cancer patients. Clin Nucl Med. 2017;42(1):e29–34.
Heinze B, Fuss CT, Mulatero P, Beuschlein F, Reincke M, Mustafa M, et al. Targeting CXCR4 (CXC chemokine receptor type 4) for molecular imaging of aldosterone-producing adenoma. Hypertension. 2018;71(2):317–25.
Shackleton C. Clinical steroid mass spectrometry: a 45-year history culminating in HPLC-MS/MS becoming an essential tool for patient diagnosis. J Steroid Biochem Mol Biol. 2010;121(3–5):481–90.
Peitzsch M, Dekkers T, Haase M, Sweep FCGJ, Quack I, Antoch G, et al. An LC-MS/MS method for steroid profiling during adrenal venous sampling for investigation of primary aldosteronism. J Steroid Biochem Mol Biol. 2015;145:75–84.
Eisenhofer G, Masjkur J, Peitzsch M, Di Dalmazi G, Bidlingmaier M, Grüber M, et al. Plasma steroid metabolome profiling for diagnosis and subtyping patients with Cushing syndrome. Clin Chem. 2018;64(3):586–96.
Gomez-Sanchez CE, Gomez-Sanchez EP, Holland OB. Role of 18-hydroxylated cortisols in hypertension. J Steroid Biochem. 1987;27(4–6):971–5.
Hamlet SM, Gordon RD, Gomez-Sanchez CE, Tunny TJ, Klemm SA. Adrenal transitional zone steroids, 18-oxo and 18-hydroxycortisol, useful in the diagnosis of primary aldosteronism, are ACTH-dependent. Clin Exp Pharmacol Physiol. 1988;15(4):317–22.
Stowasser M, Bachmann AW, Tunny TJ, Gordon RD. Production of 18-oxo-cortisol in subtypes of primary aldosteronism. Clin Exp Pharmacol Physiol. 1996;23(6–7):591–3.
Raman PB, Sharma DC, Dorfman RI, Gabrilove JL. Biosynthesis of C-18-oxygenated steroids by an aldosterone-secreting human adrenal tumor. Metabolism of [4-14C] progesterone, [1,2-3H]11-deoxycorticosterone, and [4-14C] pregnenolone. Biochemistry. 1965;4(7):1376–85.
Ulick S, Chu MD. Hypersecretion of a new corticosteroid, 18-hydroxycortisol in two types of adrenocortical hypertension. Clin Exp Hypertens A. 1982;4(9–10):1771–7.
Gordon RD, Hamlet SM, Tunny TJ, Gomez-Sanchez CE, Jayasinghe LS. Distinguishing aldosterone-producing adenoma from other forms of hyperaldosteronism and lateralizing the tumour pre-operatively. Clin Exp Pharmacol Physiol. 1986;13(4):325–8.
Ulick S, Blumenfeld JD, Atlas SA, Wang JZ, Vaughan ED Jr. The unique steroidogenesis of the aldosteronoma in the differential diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 1993;76(4):873–8.
Nakamura Y, Satoh F, Morimoto R, Kudo M, Takase K, Gomez-Sanchez CE, et al. 18-oxocortisol measurement in adrenal vein sampling as a biomarker for subclassifying primary aldosteronism. J Clin Endocrinol Metab. 2011;96(8):E1272–8.
Mulatero P, di Cella SM, Monticone S, Schiavone D, Manzo M, Mengozzi G, et al. 18-Hydroxycorticosterone, 18-hydroxycortisol, and 18-oxocortisol in the diagnosis of primary aldosteronism and its subtypes. J Clin Endocrinol Metab. 2012;97(3):881–9.
• Satoh F, Morimoto R, Ono Y, Iwakura Y, Omata K, Kudo M, et al. Measurement of peripheral plasma 18-oxocortisol can discriminate unilateral adenoma from bilateral diseases in patients with primary aldosteronism. Hypertension. 2015;65(5):1096–102. This study is very important because it uses measuring of the adrenal steroid 18oxoF for subtyping and reveales a high specifity and sensitivity for distinction of uni- and bilateral disease with just this one biomarker, very relevant for this review.
Zheng F-F, Zhu L-M, Nie A-F, Li X-Y, Lin J-R, Zhang K, et al. Clinical characteristics of somatic mutations in Chinese patients with aldosterone-producing adenoma. Hypertension. 2015;65(3):622–8.
Williams TA, Monticone S, Mulatero P. KCNJ5 mutations are the most frequent genetic alteration in primary aldosteronism. Am Heart Assoc; 2015.
•• Eisenhofer G, Dekkers T, Peitzsch M, Dietz AS, Bidlingmaier M, Treitl M, et al. Mass spectrometry-based adrenal and peripheral venous steroid profiling for subtyping primary aldosteronism. Clin Chem. 2016;62(3):514–24. This study is very important because it analyzes the use of LC-MS/MS steroid profiling for subtyping PA in a large patient cohort, very relevant for this review.
Yang Y, Burrello J, Burrello A, Eisenhofer G, Peitzsch M, Tetti M, et al. Classification of microadenomas in patients with primary aldosteronism by steroid profiling. J Steroid Biochem Mol. 2019;189:274–82.
Lenzini L, Rossitto G, Maiolino G, Letizia C, Funder JW, Rossi GP. A meta-analysis of somatic KCNJ5 K+ channel mutations in 1636 patients with an aldosterone-producing adenoma. J Clin Endocrinol Metab. 2015;100(8):E1089–95.
Franco L, Mario E, Basso SM, Decio A, Maurizio I, Gennaro F. Long-term results of adrenalectomy in patients with aldosterone-producing adenomas: multivariate analysis of factors affecting unresolved hypertension and review of the literature. Am Surg. 2005;71(10):864–9.
Zarnegar R, Young WF Jr, Lee J, Sweet MP, Kebebew E, Farley DR, et al. The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg. 2008;247(3):511–8.
• Burrello J, Burrello A, Stowasser M, Nishikawa T, Quinkler M, Prejbisz A, Lenders JW, Satoh F, Mulatero P, Reincke M. The primary aldosteronism surgical outcome score for the prediction of clinical outcomes after adrenalectomy for unilateral primary aldosteronism. Ann Surg 2019. In press. This study is very important because it uses different (clinical) parameters for prediction of outcome in PA, very relevant to the topic of this review.
Quillo AR, Grant CS, Thompson GB, Farley DR, Richards ML, Young WF. Primary aldosteronism: results of adrenalectomy for nonsingle adenoma. J Am Coll Surg. 2011;213(1):106–12.
Citton M, Viel G, Rossi GP, Mantero F, Nitti D, Iacobone M. Outcome of surgical treatment of primary aldosteronism. Langenbeck's Arch Surg. 2015;400(3):325–31.
Grytaas MA, Strømsøy SS, Rørvik JT, Arnes JB, Heie A, Arnesen T, et al. Clinical characteristics and long-term outcome of primary aldosteronism in a Norwegian population. Horm Metab Res. 2017;49(11):838–46.
Volpe C, Hamberger B, Höög A, Mukai K, Calissendorff J, Wahrenberg H, et al. Primary aldosteronism: functional histopathology and long-term follow-up after unilateral adrenalectomy. Clin Endocrinol. 2015;82(5):639–47.
Funding
This work was supported by the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation program (grant agreement no. 694913 to MR) and by the Deutsche Forschungsgemeinschaft (DFG) (within the CRC/Transregio 205/1 “The Adrenal: Central Relay in Health and Disease” to GE, MR, and TAW and grant RE 752/20-1 to MR) and the Else Kröner-Fresenius Stiftung in support of the German Conns Registry-Else-Kröner Hyperaldosteronism Registry (2013_A182 and 2015_A171 to MR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Hypertension and the Kidney
Rights and permissions
About this article
Cite this article
Holler, F., Heinrich, D.A., Adolf, C. et al. Steroid Profiling and Immunohistochemistry for Subtyping and Outcome Prediction in Primary Aldosteronism—a Review. Curr Hypertens Rep 21, 77 (2019). https://doi.org/10.1007/s11906-019-0985-0
Published:
DOI: https://doi.org/10.1007/s11906-019-0985-0