Abstract
The emergence and global spread of drug resistant Acinetobacter (A.) baumannii is a cause of great concern. The current knowledge on antibiotic resistance in A. baumannii from animal origin is mostly based on few internationally published case reports, investigations of strain collections and several whole genome analyses. This lack of data results in a somewhat sketchy picture on how to assess the possible impact of drug resistant A. baumannii strains on veterinary and public health in Germany. Consequently, there is an urgent need to intensify the surveillance of A. baumannii in pet animals, the farm animal population and wildlife.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acinetobacter (A.) baumannii is a gram-negative opportunistic nosocomial pathogen belonging to the genus Acinetobacter and a member of the family Moraxellaceae. Acinetobacter spp. are non-motile, non-fastidious Gram-negative, non-fermenting, catalase positive, oxidase negative, strictly aerobic coccobacilli with a DNA G + C content between 39 and 47% (Peleg et al. 2008). Currently, there are 57 validly published species names (including 4 synonymous species) (Parte 2018). Of these, the species A. baumannii, A. nosocomialis and A. pittii are of clinical importance, as they have been isolated from human infections and hospital outbreaks (Visca et al. 2011). According to Bergogne-Bérézin and Towner (1996) the first reports on severe infections most likely caused by A. baumannii date back to the 1970ies. However, due to the numerous taxonomic changes the genus Acinetobacter has been subjected to, these earlier reports have to be regarded with caution as the species A. baumannii was formally just designated in 1986 by Bouvet and Grimont.
Strain typing by different techniques has revealed genotypic diversity within the species A. baumannii, however, only a limited number of widespread clones appear to be responsible for hospital outbreaks in many countries (Diancourt et al. 2010). Eight international clonal lineages have been described so far and comparative typing of outbreak strains obtained all over Europe revealed the dominance of three clones, originally named European clones I-III (Dijkshoorn et al. 1996; Karah et al. 2012). These clones were re-named “international clones (IC) 1-3” after identifying them throughout the world. IC 1–3 correspond to the multi-locus sequence typing (MLST) clonal complexes (ST1–3) (Diancourt et al. 2010; Antunes et al. 2014).
In humans, A. baumannii can cause a multitude of severe nosocomial infections of the skin and soft tissue, wound infections, urinary tract infections and secondary meningitis. The highest mortality rates however, are seen in ventilator-associated pneumonia and bloodstream infections (Dijkshoorn et al. 2007). In comparison to human medicine, the data obtained from veterinary medicine are relatively limited (Müller et al. 2014; van der Kolk et al. 2018). In livestock (cattle, pig), A. baumannii has been observed as a cause of mastitis, pneumonia, and sepsis. Horses have been reported to develop wound infections, septicaemia, and bronchopneumonia as well as neonatal encephalopathy and eye infections. In dogs and cats A. baumannii has been isolated from wound, bloodstream and urinary tract infections (Müller et al. 2014; van der Kolk et al. 2018).
The genus Acinetobacter has the tendency to develop antibiotic resistance very rapidly, possibly due to its long-term evolutionary exposure to antibiotic-producing organisms in the soil environment (Bergogne-Bérézin and Towner 1996). Moreover, a major feature of A. baumannii, enabling its prolonged survival and spread within the healthcare system, is its ability to not only upregulate intrinsic but also to acquire foreign mechanisms of antimicrobial resistance (Pogue et al. 2013). The European Committee on Antimicrobial Susceptibility Testing (EUCAST) expert rules V 3.1 state that A. baumannii is naturally (or intrinsically) resistant to the following antimicrobials: ampicillin, amoxicillin-clavulanic acid, cefazolin, cefalothin, cephalexin, cefadroxil, cefotaxime, ceftriaxone, aztreonam, ertapenem, trimethoprim and fosfomycin. It is still a matter of debate as to whether the augmented antimicrobial resistance found in clinical Acinetobacter baumannii isolates may also lead to reduced susceptibility to disinfectants. While Ivancovic et al. (2017), Babaei et al. (2015) and Kawamura-Sato et al. (2010) were able to demonstrate reduced susceptibility to disinfectants, no correlation was found by Martro et al. (2003).
A wide array of resistance mechanisms have been described for A. baumannii such as ß-lactamases, outer membrane proteins (OMPs), efflux influencing proteins, aminoglycoside modifying enzymes, chromosomal mutations in the quinolone resistance determining region (QRDR), enzymes targeting tetracycline-specific efflux, glycocyclines as well as ribosomal methylation (Peleg et al. 2008; Evans et al. 2013). A particular challenge is the resistance to carbapenems, which is predominantly mediated by Ambler Class D ß-lactamases, such as the intrinsic carbapenem-hydrolysing oxacillinase OXA-51, which confers resistance to carbapenems when overexpressed or the acquisition and production of the oxacillinases OXA-23-like, OXA-24/40-like, OXA-58-like, OXA-143-like and OXA-235-like (da Silva et al. 2016). Their corresponding genes can be upregulated by insertion sequences (IS) located upstream of these genes, e.g. ISAba-1. Metallo-ß-lactamases such as imipemenase (IMP), Verona integrin-encoded-metallo-ß-lactamase (VIM) and New Delhi metallo-ß-lactamase (NDM) have been reported in Europe but currently appear to play a minor role (Evans et al. 2013). The production of K. pneumoniae carbapenemase (KPC) and OXA-48 oxacillinase has been reported from the Middle East and South America, respectively (Elsherif et al. 2016; Martinez et al. 2016).
The emergence of drug resistant Acinetobacter spp., especially A. baumannii in hospitals, but also in veterinary clinics and the environment has been observed throughout the world and has become a cause of concern (Dijkshoorn et al. 2007; Diancourt et al. 2010; Müller et al. 2014; van der Kolk et al. 2018). Severe nosocomial infections are recurrently associated with epidemic spread, outbreak strains are frequently multi-drug resistant (MDR) and the increasing occurrence of strains resistant to carbapenems or to last resource antimicrobial agents such as colistin is alarming (Diancourt et al. 2010; Zordan et al. 2011; Zarrilli et al. 2013; Guerra et al. 2014).
The aim of this short review is to summarise the current knowledge and data on antimicrobial resistance determined in A. baumannii strains isolated from animal and environmental sources in Germany.
Antimicrobial resistance in A. baumannii originating from animal hosts
To date, only few reports exist on the prevalence of antibiotic resistance in A. baumannii isolated from animal origin in Germany (Table 1). The earliest study on multidrug resistant Acinetobacter spp. in Germany analysed 52 A. baumannii, 3 A. pittii strains and one non defined Acinetobacter isolate from hospitalised animals (dog, cat, horse, cow) collected between 2000 and 2008. The isolates could be allocated to the international clones 1, 2 and 3, respectively, and were resistant to oxacillin, penicillin, cephaloitin, erythromycin, clindamycin, chloramphenicol, and, with the exception of two isolates, to colistin. Bar of one isolate, all strains were sensitive to imipenem and amikacin, respectively. This study also revealed the possible endemic occurrence of Acinetobacter spp. within an animal clinic (Zordan et al. 2011).
The first description and genome sequence of a carbapenem-resistant A. baumannii strain isolated in 2000 and originating from a cat was in 2016 by Ewers and co-workers. Phylogenetic analyses revealed that the isolate belonged to the globally distributed international clone IC1 and displayed a close resemblance to clonal lineages causing severe infections in humans. The strain harboured a plasmid encoding for blaoxa-23; other resistance coding genes detected in the genome were aminoglycoside resistance genes, blaoxa-51-like gene encoding OXA-69, a phenicol resitance gene (catA1), a sulfonamide (sul1) and a tetracycline (tetA) resistance coding gene, respectively. High MIC breakpoints were determined for imipenem, piperacillin, cefpirome, gentamycin, tetracycline and trimethoprim/sulfamethoxazole (Ewers et al. 2016). A later study by the same group screened 223 A. baumannii isolates collected between 2000 and 2013 from companion animals (dog, cat, rabbit, ferret, snake, rat, duck) for carbapenem-non-susceptibility testing (Ewers et al. 2017). Fifty-eight isolates carried blaoxa-66 with the upstream insertion sequence element ISAba1; further three isolates (cat; dogs) harboured blaoxa-23, belonged to the IC 1 and 8, respectively, and were resistant to piperacillin, piperacillin/tazobactam, ampicillin/sulbactam, ceftazidime, cefuroxime, cefpodoxime, imipenem, meropenem and trimethoprim/sulphametazole. All three isolates carried the aminoglycoside-modifying enzyme gene aadA1, and one isolate aacC1. The 58 ISAba1- blaoxa-66-positive isolates belonged to the IC 2, 53 were resistant to piperacillin, 11 to piperacillin/tazobactam, 20 to ampicillin/sulbactam, 9 to ceftazidime, 22 to cefuroxime, 21 to cefpodoxime, 0 to imipenem, 0 to meropenem, 53 to gentamycin, 5 to levofloxacin and 28 to trimethoprim/sulphametazole. Of the 58 isolates 35 carried the aminoglycoside-modifying enzyme gene aadA1, and 55 isolates aacC1. This study demonstrated that two of the most common mechanisms of carbapenem-non-susceptibility found in human A. baumannii isolates, i.e. the acquisition of the carbapenemase-hydrolysing enzyme blaoxa-23 and possession of the insertion sequence ISAba1 upstream of the blaoxa-51-like gene, are also found in isolates originating from companion animals.
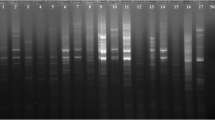
A further study tested the hypothesis whether birds might be a reservoir for A. baumannii (Wilharm et al. 2018). Two hundred and twenty chickens from 37 flocks were sampled between 2012 and 2013, yielding six A. baumannii isolates from three independent farms. Three isolates originated from the same farm from chicks at fledgling state, two from a flock at a different farm with 1 day old chicks and one from a hen at a further farm. The isolates of the fledglings and the hen were closely related as determined by ApaI macrorestriction analyses, but distinct from the closely related isolates obtained from the 1 day old chicks. These results were further corroborated by sequencing of the blaoxa-51-like gene, revealing an OXA-68 variant in the fledglings and the hen. The isolates of the one day old chicks harboured a novel blaoxa-51-like gene variant, OXA-385 and were resistant to gentamycin and kanamycin. None of the chicken isolates could be matched to the international clonal lineages. Further screening of 40 goslings at a single farm yielded three A. baumannii isolates carrying different variants of the blaoxa-51-like gene encoding OXA-314, OXA-71 and OXA-95, respectively. Also here a match to the international clonal lineages was not possible. Only one of the isolates was submitted to antimicrobial resistance testing to reveal intermediate susceptibility to kanamycin and resistance to sulfamerazine and sulfamerazine/trimethoprim.
The most recent published work studying extended spectrum ß-lactamase producing E. coli (ESBL) in 341 horses entering a veterinary teaching hospital between 2014 and 2015, found nine A. baumannii isolates (Walther et al. 2018). No carbapenemase activity was observed in these isolates, one isolate displayed a MDR phenotype (ceftiofur, gentamycin, tetracycline, tobramycin, trimethoprim/sulphametazole), whereas the remaining eight were resistant to ceftiofur. The authors stated that veterinary infection control measures must be implemented into the clinical setting.
Antimicrobial resistance in A. baumannii originating from non-clinical samples
Several publications on A. baumannii from non-clinical origin exist (Table 1). A short note by Hauer et al. (1999), reports on the isolation of A. baumannii from tap water and anti-splash nozzles in a hospital in 1998, which ultimately contaminated the tea used for mouth washes. The isolates were sensitive to cotrimaxole, no further information on antimicrobial resistance testing was provided.
In 2013, Faulde and Spiesberger reported on the role of the moth fly Clogima (C.) albipunctata as a mechanical vector of bacterial pathogens in four infested hospitals. A total of 15 A. baumannii strains was isolated from 271 adult C. albipunctata collected between 2011 and 2012 from shower cubicles, patient wards, rest rooms and hospital kitchens. Antimicrobial resistance testing revealed comparable cephalosporinase and ß-lactamase-positive resistance patterns, one strain showed partial drug resistance to three groups of antibiotics, i.e. third-generation cephalosporins, penicillins and two aminoglycosides and thus qualified as a MDR strain. The authors stated that C. albipunctata is an indicator of poor hygiene, water and pest control in hospitals, but that bacterial investigation of the moth flies might be an option for monitoring contaminated hospital environments and for nosocomial pathogens.
The most recent study on A. baumannii in Germany addressed the question whether isolates from food harboured antibiotic resistances and if the food route had an impact on the dissemination of resistance genes (Cho et al. 20,018). Forty-two A. baumannii isolates obtained from dry milk samples were tested for antimicrobial resistance by means of the Kirby-Bauer disc diffusion method. All strains could be allocated to the European clonal lineages II and III, were PCR positive for blaoxa-51 and resistant to chloramphenicol and oxacillin. Genome sequencing of nine A. baumannii isolates revealed four isolates to be positive for blaoxa-530 and further four to be positive for blaoxa-91 and blaoxa-430 genes, all belonging to the blaoxa-51-like family. The strains moreover contained a blaADC-25-like gene encoding for an intrinsic AmpC beta-lactamase. As the tested strains were generally not resistant to clinically relevant antibiotics such as tobramycin, ciprofloxacin, cefepime and meropenem, the authors concluded that the food route currently poses only a low risk for MDR Acinetobacter strains and transmission of resistance genes.
Discussion
Antibiotic resistance in human A. baumannii infections is closely monitored among the medical profession in Germany and numerous case studies, epidemiological surveys and reviews are regularly published (Huenges et al. 2016; Katchanov et al. 2018; Schleicher et al. 2012). This however, does not apply to veterinary medicine. The current knowledge on antibiotic resistance in A. baumannii from animal origin is mostly based on internationally published case reports, investigations of strain collections and several whole genome analyses as summarised by Müller et al. (2014) and van der Kolk et al. (2018). This lack of data results in a somewhat sketchy picture on how to assess the impact of drug resistant A. baumannii strains on veterinary and public health. It is not yet clear if animals indeed pose a risk as reservoir for A. baumannii; genetically distinct animal isolates have been reported by Wilharm et al. (2018) and by van der Kolk et al. (2018), whereas companion animals have been found to carry isolates more closely related to human strains (Ewers et al. 2017; Walther et al. 2018), which could be an indication for humans possibly infecting their pets.
Hardly any data exist regarding the presence of drug resistant A. baumannii in food and food-producing animals in Germany. A. baumannii are regularly found in milk samples, however the majority of antimicrobial susceptibility patterns detected were not against clinically relevant antibiotics (Cho et al. 2018), which is in agreement with a similar study from Korea (Gurung et al. 2013). In a recent study, Klotz et al. (2018) isolated carbapenem-resistant Acinetobacter indicus harbouring blaoxa-23 on transposable elements from cattle. Despite the presumptive low pathogenicity of A. indicus, these isolates could contribute to the spreading of the blaoxa-23 gene to other receptive bacterial species and to their dissemination into the environment via manure, thus further contributing to the contamination of e g. vegetables for human consumption.
Notwithstanding the global distribution of drug resistant A. baumannii in the animal population, it is still not clear if the higher reporting rates are due to increased awareness of the agent, close human animal contact, changes in animal husbandry, a spill over from humans to animals or the detection of the agent in a statistically skewed population.
Conclusions
Data on the general distribution of A. baumannii in the farm animal population in Germany are next to none and scarce for pet animals. Information on A. baumannii in wildlife, i.e. game and birds is missing and the possible influence of these animals on the dissemination of the agent to livestock and pets is unknown. Due to the ability of A. baumannii to survive in the environment for prolonged time and its ability to acquire resistance genes with relative ease, screening and implementation of hygiene strategies to minimise transmission and spread is recommended.
Several mechanisms conferring resistance to carbapenems in A. baumannii have been detected both in isolates originating from humans and companion animals in Germany. However, the impact of these findings on German veterinary and public health is difficult to assess, as conclusive data on antibiotic resistance in A. baumannii from animal and environmental origin in Germany are limited.
References
Antunes LC, Visca P, Towner KJ (2014) Acinetobacter baumannii: evolution of a global pathogen. Pathog Dis 71:292–301. https://doi.org/10.1111/2049-632X.12125
Babaei M, Sulong A, Hamat R, Nordin S, Neela V (2015) Extremely high prevalence of antiseptic resistant Quaternary Ammonium Compound E gene among clinical isolates of multiple drug resistant Acinetobacter baumannii in Malaysia. Ann Clin Microbiol Antimicrob 14:11. https://doi.org/10.1186/s12941-015-0071-7
Bergogne-Bérézin E, Towner KJ (1996) Acinetobacter spp. as nosocomial pathogens: microbiological, clinical, and epidemiological features. CMR 9:148–165. https://doi.org/10.1128/CMR.9.2.148
Cho GS, Li B, Rostalsky A, Fiedler G, Rösch N, Igbinosa E, Kabisch J, Bockelmann W, Hammer P, Huys G, Franz CMAP (2018) Diversity and antibiotic susceptibility of Acinetobacter strains from Milk powder produced in Germany. Front Microbiol 9:536. https://doi.org/10.3389/fmicb.2018.00536
Da Silva GJ, Domingues S (2016) Insights on the Horizontal Gene Transfer of Carbapenemase Determinants in the Opportunistic Pathogen Acinetobacter baumannii. Microorganisms 4(3). https://doi.org/10.3390/microorganisms4030029
Diancourt L, Passet V, Nemec A, Dijkshoorn L, Brisse S (2010) The population structure of Acinetobacter baumannii: expanding multiresistant clones from an ancestral susceptible genetic pool. PLoS One 5(4):e10034. https://doi.org/10.1371/journal.pone.0010034
Dijkshoorn L, Aucken H, Gerner-Smidt P, Janssen P, Kaufmann ME, Garaizar J, Ursing J, Pitt TL (1996) Comparison of outbreak and nonoutbreak Acinetobacter baumannii strains by genotypic and phenotypic methods. JCM 34:1519–1525
Dijkshoorn L, Nemec A, Seifert H (2007) An increasing threat in hospitals: multidrug-resistant Acinetobacter baumannii. Nat Rev Microbiol 5:939–951. https://doi.org/10.1038/nrmicro1789
Elsherif R, Ismail D, Elawady S, Jastaniah S, Al-Masaudi S, Harakeh S, Karrouf G (2016) Boronic acid disk diffusion for the phenotypic detection of polymerase chain reaction-confirmed, carbapenem-resistant, gram-negative bacilli isolates. BMC Microbiol 16:135
Evans BA, Hamouda A, Amyes SG (2013) The rise of carbapenem-resistant Acinetobacter baumannii. Curr Pharm Des 19:223–238. https://doi.org/10.2174/1381612811306020223
Ewers C, Klotz P, Scheufen S, Leidner U, Göttig S, Semmler T (2016) Genome sequence of OXA-23 producing Acinetobacter baumannii IHIT7853, a carbapenem-resistant strain from a cat belonging to international clone IC1. Gut Pathog 8:37. https://doi.org/10.1186/s13099-016-0119-z
Ewers C, Klotz P, Leidner U, Stamm I, Prenger-Berninghoff E, Göttig S, Semmler T, Scheufen S (2017) OXA-23 and ISAba1-OXA-66 class D β-lactamases in Acinetobacter baumannii isolates from companion animals. Int J Antimicrob Agents 49:37–44. https://doi.org/10.1016/j.ijantimicag.2016.09.033
Faulde M, Spiesberger M (2013) Role of the moth fly Clogmia albipunctata (Diptera: Psychodinae) as a mechanical vector of bacterial pathogens in German hospitals. J Hosp Infect 83:51–60. https://doi.org/10.1016/j.jhin.2012.09.019
Guerra B, Fischer J, Helmuth R (2014) An emerging public health problem: acquired carbapenemaseproducing microorganisms are present in food-producing animals, their environment, companion animals and wild birds. Vet Microbiol 171:290–297. https://doi.org/10.1016/j.vetmic.2014.02.001
Gurung M, Nam HM, Tamang MD, Chae MH, Jang GC, Jung SC, Lim SK (2013) Prevalence and antimicrobial susceptibility of Acinetobacter from raw bulk tank milk in Korea. J Dairy Sci 96:1997–2002. https://doi.org/10.3168/jds.2012-5965
Hauer T, Jonas D, Dettenkofer M, Daschner FD (1999) Tea as a source of Acinetobacter baumannii ventilator-associated pneumonia? Infect Control Hosp Epidemiol 20:594. https://doi.org/10.1086/503149
Huenges K, Reinecke A, Bewig B, Haneya A, Cremer J (2016) Lung Transplantation in a Multidrug-Resistant Gram-Negative Acinetobacter Baumannii-Colonized Patient: A Case Report. Thorac Cardiovasc Surg Rep 5:16–17. https://doi.org/10.1055/s-0035-1569993
Ivanković T, Goić-Barišić I, Hrenović J (2017) Reduced susceptibility to disinfectants of Acinetobacter baumannii biofilms on glass and ceramic. Arh Hig Rada Toksikol 68:99–108. https://doi.org/10.1515/aiht-2017-68-2946
Karah N, Sundsfjord A, Towner K, Samuelsen Ø (2012) Insights into the global molecular epidemiology of carbapenem non-susceptible clones of Acinetobacter baumannii. Drug Resist Updat 15:237–247. https://doi.org/10.1016/j.drup.2012.06.001
Kawamura-Sato K, Wachino J, Kondo T, Ito H, Arakawa Y (2010) Correlation between reduced susceptibility to disinfectants and multidrug resistance among clinical isolates of Acinetobacter species. J Antimicrob Chemother 65(9):1975–1983. https://doi.org/10.1093/jac/dkq227
Katchanov J, Asar L, Klupp EM, Both A, Rothe C, König C, Rohde H, Kluge S, Maurer FP (2018) Carbapenem-resistant Gram-negative pathogens in a German university medical center: Prevalence, clinical implications and the role of novel β-lactam/β-lactamase inhibitor combinations. PLoS One 13(4):e0195757. https://doi.org/10.1371/journal.pone.0195757
Klotz P, Jacobmeyer L, Stamm I, Leidner U, Pfeifer Y, Semmler T, Prenger-Berninghoff E, Ewers C (2018) Carbapenem-resistant Acinetobacter baumannii ST294 harbouring the OXA-72 carbapenemase from a captive grey parrot. J Antimicrob Chemother 73:1098–1100. https://doi.org/10.1093/jac/dkx490
Martínez T, Ropelewski AJ, González-Mendez R, Vázquez GJ, Robledo IE (2016) Draft Genome Sequence of a Multidrug-Resistant Klebsiella pneumoniae Carbapenemase-Producing Acinetobacter baumannii Sequence Type 2 Isolate from Puerto Rico. Genome Announc 4(4). https://mra.asm.org/content/4/4/e00758-16. Accessed 9 Oct 2018
Martró E, Hernández A, Ariza J, Domínguez MA, Matas L, Argerich MJ, Martin R, Ausina V (2003) Assessment of Acinetobacter baumannii susceptibility to antiseptics and disinfectants. J Hosp Infect 55(1):39–46. https://doi.org/10.1016/S0195-6701(03)00220-2
Müller S, Janssen T, Wieler LH (2014) Multidrug resistant Acinetobacter baumannii in veterinary medicine - emergence of an underestimated pathogen? BMTW 127:435–446
Parte AC (2018) LPSN – list of prokaryotic names with standing in nomenclature (bacterio.net), 20 years on. IJSEM 68:1825–1829. https://doi.org/10.1099/ijsem.0.002786
Peleg AY, Seifert H, Paterson DL (2008) Acinetobacter baumannii: emergence of a successful pathogen. CMR 21:538–582. https://doi.org/10.1128/CMR.00058-07
Pogue JM, Mann T, Barber KE, Kaye KS (2013) Carbapenem-resistant Acinetobacter baumannii: epidemiology, surveillance and management. Expert Rev Anti-Infect Ther 11:383–393. https://doi.org/10.1586/eri.13.14
Schleicher X, Higgins PG, Wisplinghoff H, Körber-Irrgang B, Kresken M, Seifert H (2013) Molecular epidemiology of Acinetobacter baumannii and Acinetobacter nosocomialis in Germany over a 5-year period (2005-2009). Clin Microbiol Infect 19:737–742. https://doi.org/10.1111/1469-0691.12026
van der Kolk JH, Endimiani A, Graubner C, Gerber V, Perreten V (2018) Acinetobacter in Veterinary Medicine with emphasis on A. baumannii. J Glob Antimicrob Resist. https://doi.org/10.1016/j.jgar.2018.08.011
Visca P, Seifert H, Towner KJ (2011) Acinetobacter infection-an emerging threat to human health. IUBMB Life 63:1048–1054. https://doi.org/10.1002/iub.534
Walther B, Klein KS, Barton AK, Semmler T, Huber C, Wolf SA, Tedin K, Merle R, Mitrach F, Guenther S, Lübke-Becker A, Gehlen H (2018) Extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli and Acinetobacter baumannii among horses entering a veterinary teaching hospital: the contemporary "Trojan horse". PLoS One 13:e0191873. https://doi.org/10.1371/journal.pone.0191873
Wilharm G, Skiebe E, Higgins PG, Poppel MT, Blaschke U, Leser S, Heider C, Heindorf M, Brauner P, Jäckel U, Böhland K, Cuny C, Łopińska A, Kaminski P, Kasprzak M, Bochenski M, Ciebiera O, Tobółka M, Żołnierowicz KM, Siekiera J, Seifert H, Gagné S, Salcedo SP, Kaatz M, Layer F, Bender JK, Fuchs S, Semmler T, Pfeifer Y, Jerzak L (2018) Relatedness of wildlife and livestock avian isolates of the nosocomial pathogen Acinetobacter baumannii to lineages spread in hospitals worldwide. Environ Microbiol 19:4349–4364. https://doi.org/10.1111/1462-2920.13931
Zarrilli R, Pournaras S, Giannouli M, Tsakris A (2013) Global evolution of multidrug-resistant Acinetobacter baumannii clonal lineages. Int J Antimicrob Agents 41:11–19. https://doi.org/10.1016/j.ijantimicag.2012.09.008
Zordan S, Prenger-Berninghoff E, Weiss R, van der Reijden T, van den Broek P, Baljer G, Dijkshoorn L (2011) Multidrug-resistant Acinetobacter baumannii in veterinary clinics, Germany. EID 17:1751–1754. https://doi.org/10.3201/eid1709.101931
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wareth, G., Neubauer, H. & Sprague, L.D. Acinetobacter baumannii – a neglected pathogen in veterinary and environmental health in Germany. Vet Res Commun 43, 1–6 (2019). https://doi.org/10.1007/s11259-018-9742-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11259-018-9742-0