Abstract
Purpose
The development of particle-based carriers for transepidermal drug delivery has become a field of major interest in dermatology. In this study, we investigated the suitability of biodegradable poly-lactic acid (PLA) particles loaded with fluorescent dyes as carriers for transepidermal drug delivery.
Methods
The penetration profiles of PLA particles (228 and 365 nm) and the release of dye from the particles were investigated in human skin explants using fluorescence microscopy, confocal laser scanning microscopy and flow cytometry.
Results
PLA particles penetrated into 50% of the vellus hair follicles, reaching a maximal depth corresponding to the entry of the sebaceous gland in 12–15% of all observed follicles. The accumulation of particles in the follicular ducts was accompanied by the release of dye to the viable epidermis and its retention in the sebaceous glands for up to 24 h. Kinetic studies in vitro as well as in skin explants revealed, that, although stable in aqueous solution, destabilization of the particles and significant release of incorporated dye occurred upon contact with organic solvents and the skin surface.
Conclusions
These results suggest that particles based on PLA polymers may be ideal carriers for hair follicle and sebaceous gland targeting.





Similar content being viewed by others
Abbreviations
- Coum-6:
-
coumarin-6
- Coum-6_PLA_365:
-
coumarin-6-loaded 365 nm PLA particles
- CSSS:
-
cyanoacrylate skin surface stripping
- IPM:
-
isopropylmiristate
- MFI:
-
mean fluorescence intensity
- NPs:
-
nanoparticles
- NR:
-
nile red
- NR_PLA_228:
-
nile red-loaded 228 nm PLA particles
- PCL:
-
poly- ε-caprolactone
- PLA:
-
poly lactic-acid
- PLGA:
-
poly-lactic-co-glycolic acid
- SLN:
-
solid lipid nanoparticles
- VHF:
-
vellus hair follicle
References
Li L, Lishko V, Hoffman RM. Liposome targeting of high molecular weight DNA to the hair follicles of histocultured skin: a model for gene therapy of the hair growth processes. In Vitro Cell Dev Biol Anim. 1993;29:258–260.
Bernard E, Dubois JL, Wepierre J. Importance of sebaceous glands in cutaneous penetration of an antiandrogen: target effect of liposomes. J Pharm Sci. 1997;86:573–578.
Li L, Hoffman RM. Topical liposome delivery of molecules to hair follicles in mice. J Dermatol Sci. 1997;14:101–108.
Alvarez-Román R, Naik A, Kalia YN, Guy RH, Fessi H. Skin penetration and distribution of polymeric nanoparticles. J Controll Release. 2004;99:53–62.
Vogt A, Mandt N, Lademann J, Schaefer H, Blume-Peytavi U. Follicular targeting-A promising tool in selective dermatotherapy. J Invest Dermatol Symp Proc. 2005;10:252–255.
Rolland A, Wagner N, Chatelus A, Shroot B, Schaefer H. Site-specific drug delivery to pilosebaceous structures using polymeric microspheres. Pharm Res. 1993;10:1738–44.
Lauer AC, Ramachandran C, Lieb LM, Niemiec S, Weiner ND. Targeted delivery to the pilosebaceous unit via liposomes. Adv Drug Deliv Rev. 1996;18:311–324.
Mordon S, Sumian Ch, Devoisselle JM. Site-specific methylene blue delivery to pilosebaceous structures using highly porous nylon microspheres an experimental evaluation. Lasers Surg Med. 2004;33:119–125.
Lademann J, Knorr F, Richter H, Blume-Peytavi U, Vogt A, Antoniou C, et al. Hair follicles: an efficient storage and penetration pathway for topically applied substances. Skin Pharmacol Physiol. 2008;21:150–155.
Michel M, L’Heureux L, Pouliot R, Xu W, Auger FA, Germain L. Characterization of a new tissue-engineered human skin equivalent with hair. In Vitro Cell Dev Biol Anim. 1999;35:318–326.
Teichmann A, Otberg N, Jacobi U, Sterry W, Lademann J. Follicular penetration: development of a method to block the follicles selectively against the penetration of topically applied substances. Skin Pharmacol Physiol. 2006;19:216–223.
Vogt A, Blume-Peytavi U. Die Biologie des menschlichen Haarfollikels. Hautarzt. 2003;54:692–698.
Toll R, Jacobi U, Richter H, Lademann J, Schaefer H, Blume-Peytavi U. Penetration profile of microspheres in follicular targeting of terminal hair follicles. J Invest Dermatol. 2004;123:168–176.
Vogt A, Combadiere B, Hadam S, Stieler KM, Lademann J, Schaefer H, et al. 40 nm, but not 750 or 1, 500 nm, Nanoparticles enter epidermal CD1a+ cells after transcutaneous application on human skin. J Invest Dermatol. 2006;126:1316–1322.
Lademann J, Richter H, Schaefer H, Blume-Peytavi U, Teichmann A, Otberg N, et al. Hair follicles—a long-term reservoir for drug delivery. Skin Pharmacol Physiol. 2006;19:232–236.
Schäfer-Korting M, Mehnert W, Korting HC. Lipid nanoparticles for improved topical application of drugs for skin diseases. Adv Drug Deliv Rev. 2007;59:427–443.
Warheit DB, Borm PJ, Hennes C, Lademann J. Testing strategies to establish the safety of nanomaterials: conclusions of an ECETOC workshop. Inhal Toxicol. 2007;19:631–643.
Cross SE, Innes B, Roberts MS, Tsuzuki T, Robertson TA, McCormick P. Human skin penetration of sunscreen nanoparticles: in-vitro assessment of a novel micronized zinc oxide formulation. Skin Pharmacol Physiol. 2007;20:148–154.
Baroli B, Ennas MG, Loffredo F, Isola M, Pinna R, López-Quintela MA. Penetration of metallic nanoparticles in human full-thickness skin. J Invest Dermatol. 2007;127:1701–1712.
Zhang LW, Monteiro-Riviere NA. Assessment of quantum dot penetration into intact, tape-stripped, abraded and flexed rat skin. Skin Pharmacol Physiol. 2008;21:166–180.
Rouse JG, Yang J, Ryman-Rasmussen JP, Barron AR, Monteiro-Riviere NA. Effects of mechanical flexion on the penetration of fullerene amino acid-derivatized peptide nanoparticles through skin. Nano Lett. 2007;7:155–160.
Ryman-Rasmussen J, Riviere JE, Monteiro-Riviere NA. Surface coatings determine cytotoxicity and irritation potential of quantum dot nanoparticles in epidermal keratinocytes. J Invest Dermatol. 2007;127:143–153.
Maurus PB, Kaeding ChC. Bioabsorbable implant material review. Oper Tech in Sport Med. 2004;12:158–160.
Burgess CM, Quiroga RM. Assessment of the safety and efficacy of poly-L-lactic acid for the treatment of HIV-associated facial lipoatrophy. J Am Acad Dermatol. 2005;52:233–239.
Beer KR, Rendon MI. Use of Sculptra™ in esthetic rejuvenation. Semin Cutan Med Surg. 2006;25:127–131.
Mohamed F, Van der Walle CF. Engineering biodegradable polyester particles with specific drug targeting and drug release properties. J Pharm Sci. 2008;97:71–87.
Lamalle-Bernard D, Munier S, Compagnon C, Charles MH, Kalyanaraman KS, Delair T, et al. Co-adsorption of HIV-1 p24 and gp120 proteins to surfactant-free anionic PLA nanoparticles preserves antigenicity and immunogenicity. J Control Release. 2006;115:57–67.
Peiser M, Grutzkau A, Wanner R, Kolde G. CD1a and CD1c cell sorting yields a homogenous population of immature human Langerhans cells. J Immunol Methods. 2003;279:41–53.
Alvarez-Román R, Naik A, Kalia YN, Guy RH, Fessi H. Enhancement of topical delivery from biodegradable nanoparticles. Pharm Res. 2004;21:1818–1825.
Vogt A, Hadam S, Heiderhoff M, Audring H, Lademann J, Sterry W, et al. Morphometry of human terminal and vellus hair follicles. Exp Dermatol. 2007;16:946–950.
Lademann J, Otberg N, Richter H, Weigmann H-J, Lindemann U, Schaefer H, et al. Investigation of follicular penetration of topically applied substances. Skin Pharmacol Appl Skin Physiol. 2001;14:17–22.
Patzelt A, Richter H, Buettemeyer R, Roewert Huber HJ, Blume-Peytavi U, Sterry W, et al. Differential stripping demonstrate a significant reduction of the hair follicle reservoir in vitro compared to in vivo. Eur J Pharm Biopharm. 2008;70:234–238.
Starcher B, Aycock RL, Hill CH. Multiple roles for elastic fibers in the skin. J Histochem Cytochem. 2005;53:431–443.
Chen H, Kim S, He W, Wang H, Low PS, Park K, et al. Fast release of lipophilic agents from circulating PEG-PDLLA micelles revealed by in vivo Förster resonance energy transfer imaging. Langmuir. 2008;24:5213–5217.
Matsumoto A, Matsukawa Y, Suzuki T, Yoshino H. Drug release characteristic of multi-reservoir type microspheres, with poly(dl-lactide-co-glycolide) and poly(dl-lactide). J Control Rel. 2005;106:172–180.
Liu SQ, Yang YY, Liu XM, Tong YW. Preparation and characterization of temperature-sensitive poly(N-isopropylacrylamide)-b-poly(D, L-lactide) microspheres for protein delivery. Biomacromolecules. 2003;4:1784–1793.
Lassalle V, Ferreira ML. PLA nano- and microparticles for drug delivery: an overview of the methods of preparation. Macromol Biosci. 2007;7:767–783.
Sawicki JA, Anderson DG, Langer R. Nanoparticle delivery of suicide DNA for epithelial ovarian cancer therapy. Adv Exp Med Biol. 2008;622:209–219.
Sanvicens N, Marco MP. Multifunctional nanoparticles–properties and prospects for their use in human medicine. Trends in Biotechnol. 2008;26:425–33.
Vogt A, Mahé B, Costagliola D, Bonduelle O, Hadam S, Schaefer G, et al. Transcutaneous anti-influenza vaccination promotes both CD4 and CD8 T cell immune responses in humans. J Immunol. 2008;180:1482–1489.
Prausnitz MR. Microneedles for transdermal drug delivery. Adv Drug Del Rev. 2004;56:581–587.
Almeida AJ, Souto E. Solid lipid nanoparticles as a drug delivery system for peptides and proteins. Adv Drug Del Rev. 2007;59:478–490.
Acknowledgements
This work was partially supported by European funding to B. Verrier through the FP6 STREP Munanovac programme. C. Primard was supported by a fellowship from the Region Rhone-Alpes (France).
Author information
Authors and Affiliations
Corresponding author
Additional information
Fiorenza Rancan and Dimitrios Papakosta have contributed equally to this work
Electronic supplementary material
Below is the link to the electronic supplementary material.
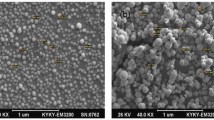
Fig S1
Cryosections of human skin after topical application of NR_PLA_228 (a-c), Coum-6_PLA_365 (d-f) and 200 nm polystyrene (PS, g-i,) particles and 16 h incubation at 37°C. Images c,f and i show the 4 time magnified image of the marked region in the corresponding sample. Most PLA particles aggregate on the follicle openings while the fluorescent dye diffused into the epidermis. On the contrary, PS particles accumulated in the follicle duct without leaking of the loaded fluorescent dye. (PPT 4160 kb)
Fig S2
NR_PLA_228 (a), Coum-6_PLA_365 (b) and polystyrene particles (c,d, Fluospheres, 200 nm) suspended in PBS were incubated 24 h with IPM. Aliquots were then collected at the PBS/IPM interface and observed with a fluorescence microscope. PLA particles form clusters at the water/IPM interface (a,b) while no clusters of PS particles were visible at the interfaces between the two phases. PS particles, in contrast, remained in dispersion in the aqueous buffer phase (c,d). (PPT 755 kb)
Rights and permissions
About this article
Cite this article
Rancan, F., Papakostas, D., Hadam, S. et al. Investigation of Polylactic Acid (PLA) Nanoparticles as Drug Delivery Systems for Local Dermatotherapy. Pharm Res 26, 2027–2036 (2009). https://doi.org/10.1007/s11095-009-9919-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-009-9919-x