Abstract
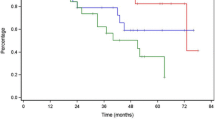
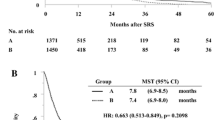
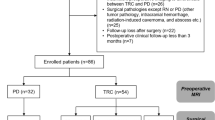
Radionecrosis is a well-characterized effect of stereotactic radiosurgery (SRS) and is occasionally associated with serious neurologic sequelae. Here, we investigated the incidence of and clinical variables associated with the development of radionecrosis and related radiographic changes after SRS for brain metastases in a cohort of patients with long-term follow up. 271 brain metastases treated with single-fraction linear accelerator-based SRS were analyzed. Radionecrosis was diagnosed either pathologically or radiographically. Univariate and multivariate Cox regression was performed to determine the association between radionecrosis and clinical factors available prior to treatment planning. After median follow up of 17.2 months, radionecrosis was observed in 70 (25.8 %) lesions, including 47 (17.3 %) symptomatic cases. 22 of 70 cases (31.4 %) were diagnosed pathologically and 48 (68.6 %) were diagnosed radiographically. The actuarial incidence of radionecrosis was 5.2 % at 6 months, 17.2 % at 12 months and 34.0 % at 24 months. On univariate analysis, radionecrosis was associated with maximum tumor diameter (HR 3.55, p < 0.001), prior whole brain radiotherapy (HR 2.21, p = 0.004), prescription dose (HR 0.56, p = 0.02) and histology other than non-small cell lung, breast or melanoma (HR 1.85, p = 0.04). On multivariate analysis, only maximum tumor diameter (HR 3.10, p < 0.001) was associated with radionecrosis risk. This data demonstrates that with close imaging follow-up, radionecrosis after single-fraction SRS for brain metastases is not uncommon. Maximum tumor diameter on pre-treatment MR imaging can provide a reliable estimate of radionecrosis risk prior to treatment planning, with the greatest risk among tumors measuring >1 cm.


Similar content being viewed by others
References
Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Ben Hassel M, Kouri M, Valeinis E, van den Berge D, Collette S, Collette L, Mueller RP (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29:134–141. doi:10.1200/JCO.2010.30.1655
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA, J Am Med Assoc 295:2483–2491. doi:10.1001/jama.295.21.2483
Korytko T, Radivoyevitch T, Colussi V, Wessels BW, Pillai K, Maciunas RJ, Einstein DB (2006) 12 Gy gamma knife radiosurgical volume is a predictor for radiation necrosis in non-AVM intracranial tumors. Int J Radiat Oncol Biol Phys 64:419–424. doi:10.1016/j.ijrobp.2005.07.980
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 77:996–1001. doi:10.1016/j.ijrobp.2009.06.006
Minniti G, Clarke E, Lanzetta G, Osti MF, Trasimeni G, Bozzao A, Romano A, Enrici RM (2011) Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol 6:48. doi:10.1186/1748-717X-6-48
Ohtakara K, Hayashi S, Nakayama N, Ohe N, Yano H, Iwama T, Hoshi H (2012) Significance of target location relative to the depth from the brain surface and high-dose irradiated volume in the development of brain radionecrosis after micromultileaf collimator-based stereotactic radiosurgery for brain metastases. J Neurooncol 108:201–209. doi:10.1007/s11060-012-0834-3
Schuttrumpf LH, Niyazi M, Nachbichler SB, Manapov F, Jansen N, Siefert A, Belka C (2014) Prognostic factors for survival and radiation necrosis after stereotactic radiosurgery alone or in combination with whole brain radiation therapy for 1–3 cerebral metastases. Radiat Oncol 9:105. doi:10.1186/1748-717X-9-105
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys 47:291–298
Flickinger JC, Kondziolka D, Pollock BE, Maitz AH, Lunsford LD (1997) Complications from arteriovenous malformation radiosurgery: multivariate analysis and risk modeling. Int J Radiat Oncol Biol Phys 38:485–490
Miyawaki L, Dowd C, Wara W, Goldsmith B, Albright N, Gutin P, Halbach V, Hieshima G, Higashida R, Lulu B, Pitts L, Schell M, Smith V, Weaver K, Wilson C, Larson D (1999) Five year results of LINAC radiosurgery for arteriovenous malformations: outcome for large AVMS. Int J Radiat Oncol Biol Phys 44:1089–1106
Voges J, Treuer H, Sturm V, Buchner C, Lehrke R, Kocher M, Staar S, Kuchta J, Muller RP (1996) Risk analysis of linear accelerator radiosurgery. Int J Radiat Oncol Biol Phys 36:1055–1063
Nakamura JL, Verhey LJ, Smith V, Petti PL, Lamborn KR, Larson DA, Wara WM, McDermott MW, Sneed PK (2001) Dose conformity of gamma knife radiosurgery and risk factors for complications. Int J Radiat Oncol Biol Phys 51:1313–1319
Barker FG 2nd, Butler WE, Lyons S, Cascio E, Ogilvy CS, Loeffler JS, Chapman PH (2003) Dose-volume prediction of radiation-related complications after proton beam radiosurgery for cerebral arteriovenous malformations. J Neurosurg 99:254–263. doi:10.3171/jns.2003.99.2.0254
Mullins ME, Barest GD, Schaefer PW, Hochberg FH, Gonzalez RG, Lev MH (2005) Radiation necrosis versus glioma recurrence: conventional MR imaging clues to diagnosis. AJNR Am J Neuroradiol 26:1967–1972
Fatterpekar GM, Galheigo D, Narayana A, Johnson G, Knopp E (2012) Treatment-related change versus tumor recurrence in high-grade gliomas: a diagnostic conundrum–use of dynamic susceptibility contrast-enhanced (DSC) perfusion MRI. AJR Am J Roentgenol 198:19–26. doi:10.2214/AJR.11.7417
Barajas RF, Chang JS, Sneed PK, Segal MR, McDermott MW, Cha S (2009) Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 30:367–372. doi:10.3174/ajnr.A1362
Gasparetto EL, Pawlak MA, Patel SH, Huse J, Woo JH, Krejza J, Rosenfeld MR, O’Rourke DM, Lustig R, Melhem ER, Wolf RL (2009) Posttreatment recurrence of malignant brain neoplasm: accuracy of relative cerebral blood volume fraction in discriminating low from high malignant histologic volume fraction. Radiology 250:887–896. doi:10.1148/radiol.2502071444
Enslow MS, Zollinger LV, Morton KA, Butterfield RI, Kadrmas DJ, Christian PE, Boucher KM, Heilbrun ME, Jensen RL, Hoffman JM (2012) Comparison of 18F-fluorodeoxyglucose and 18F-fluorothymidine PET in differentiating radiation necrosis from recurrent glioma. Clin Nucl Med 37:854–861. doi:10.1097/RLU.0b013e318262c76a
Hatzoglou V, Ulaner GA, Zhang Z, Beal K, Holodny AI, Young RJ (2013) Comparison of the effectiveness of MRI perfusion and fluorine-18 FDG PET-CT for differentiating radiation injury from viable brain tumor: a preliminary retrospective analysis with pathologic correlation in all patients. Clin Imaging 37:451–457. doi:10.1016/j.clinimag.2012.08.008
Nedzi LA, Kooy H, Alexander E 3rd, Gelman RS, Loeffler JS (1991) Variables associated with the development of complications from radiosurgery of intracranial tumors. Int J Radiat Oncol Biol Phys 21:591–599
Varlotto JM, Flickinger JC, Niranjan A, Bhatnagar AK, Kondziolka D, Lunsford LD (2003) Analysis of tumor control and toxicity in patients who have survived at least one year after radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 57:452–464
Varlotto JM, Flickinger JC, Niranjan A, Bhatnagar A, Kondziolka D, Lunsford LD (2005) The impact of whole-brain radiation therapy on the long-term control and morbidity of patients surviving more than one year after gamma knife radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 62:1125–1132. doi:10.1016/j.ijrobp.2004.12.092
Kjellberg RN, Hanamura T, Davis KR, Lyons SL, Adams RD (1983) Bragg-peak proton-beam therapy for arteriovenous malformations of the brain. N Engl J Med 309:269–274. doi:10.1056/NEJM198308043090503
Flickinger JC, Lunsford LD, Kondziolka D, Maitz AH, Epstein AH, Simons SR, Wu A (1992) Radiosurgery and brain tolerance: an analysis of neurodiagnostic imaging changes after gamma knife radiosurgery for arteriovenous malformations. Int J Radiat Oncol Biol Phys 23:19–26
Lawrence YR, Li XA, el Naqa I, Hahn CA, Marks LB, Merchant TE, Dicker AP (2010) Radiation dose-volume effects in the brain. Int J Radiat Oncol Biol Phys 76:S20–S27. doi:10.1016/j.ijrobp.2009.02.091
Chin LS, Ma L, DiBiase S (2001) Radiation necrosis following gamma knife surgery: a case-controlled comparison of treatment parameters and long-term clinical follow up. J Neurosurg 94:899–904. doi:10.3171/jns.2001.94.6.0899
Boothe D, Young R, Yamada Y, Prager A, Chan T, Beal K (2013) Bevacizumab as a treatment for radiation necrosis of brain metastases post stereotactic radiosurgery. Neuro-oncology 15:1257–1263. doi:10.1093/neuonc/not085
Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele BN, Grewal J, Prabhu S, Loghin M, Gilbert MR, Jackson EF (2011) Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys 79:1487–1495. doi:10.1016/j.ijrobp.2009.12.061
Belohlavek O, Simonova G, Kantorova I, Novotny J Jr, Liscak R (2003) Brain metastases after stereotactic radiosurgery using the Leksell gamma knife: can FDG PET help to differentiate radionecrosis from tumour progression? Eur J Nucl Med Mol Imaging 30:96–100. doi:10.1007/s00259-002-1011-2
Langleben DD, Segall GM (2000) PET in differentiation of recurrent brain tumor from radiation injury. J Nucl Med 41:1861–1867
Memorial Sloan-Kettering Cancer Center; National Institutes of Health. 18F-Fluorocholine (18F-FCho) to Distinguish Necrosis From Recurrence in Brain Metastases. In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). 2000—[cited 2014 Oct 26]. Available from: https://clinicaltrials.gov/ct2/show/NCT02037945. NLM Identifier: NCT02037945
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kohutek, Z.A., Yamada, Y., Chan, T.A. et al. Long-term risk of radionecrosis and imaging changes after stereotactic radiosurgery for brain metastases. J Neurooncol 125, 149–156 (2015). https://doi.org/10.1007/s11060-015-1881-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1881-3