Abstract
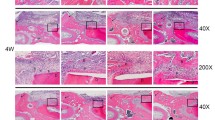
Progranulin (PGRN) has been proved to play a crucial role in anti-inflammation and osteogenesis promotion; thus, it was hypothesized that PGRN could promote bone regeneration in periodontal disease. In this experiment, the periodontal bone defects were established in periodontitis rats; recombinant human progranulin (rhPGRN), tumor necrosis factor alpha inhibitor (anti-TNF-α), or phosphate buffer saline (PBS)-loaded collagen membrane scaffolds were implanted within defects and the rats were sacrificed at scheduled time points. Volume of new bone was assessed by radiological and histomorphometric analyses. Expression of osteogenesis-related markers and tumor necrosis factor-α (TNF-α) was evaluated using immunohistochemistry. Tartrate-resistant acid phosphatase (TRAP) staining was also performed to determine the number of osteoclasts. Immunofluorescence (IF) staining was performed to explore the interaction between rhPGRN and tumor necrosis factor receptors (TNFRs). The results showed that the rhPGRN group had significantly superior quantity and quality of newly formed bone, higher expression of alkaline phosphatase (ALP), runt-related transcription factor 2 (Runx2), and TNFR2 compared with the PBS group and the anti-TNF-α group. Similarly to the anti-TNF-α group, the rhPGRN group also exhibited the significant inhibitory effect on the expression of TNF-α and the number of TRAP-positive cells compared with the PBS group. Hence, our experiment suggests that PGRN promotes regeneration of inflammatory periodontal bone defect in rats via anti-inflammation, osteoclastogenic inhibition, and osteogenic promotion. Local administration of PGRN may provide a new therapeutic strategy for periodontal bone regeneration.








Similar content being viewed by others
References
Chapple, I.L., F. Van der Weijden, C. Doerfer, et al. 2015. Primary prevention of periodontitis: Managing gingivitis. Journal of Clinical Periodontology 42 (Suppl 16): S71–S76.
Bartold, P.M., M.D. Cantley, and D.R. Haynes. 2010. Mechanisms and control of pathologic bone loss in periodontitis. Periodontology 53 (1): 55–69.
Nakajima, T., and K. Yamazaki. 2009. Periodontal disease and risk of atherosclerotic coronary heart disease. Odontology 97 (2): 84–91.
Mercado, F.B., R.I. Marshall, and P.M. Bartold. 2003. Inter-relationships between rheumatoid arthritis and periodontal disease. A review. Journal of Clinical Periodontology 30 (9): 761–772.
Chapple, I.L., and R. Genco. 2013. Diabetes and periodontal diseases: Consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. Journal of Clinical Periodontology 84 (s14): 106–112.
Zhang, H., S. Liu, B. Zhu, Q. Xu, Y. Ding, and Y. Jin. 2016. Composite cell sheet for periodontal regeneration: Crosstalk between different types of MSCs in cell sheet facilitates complex periodontal-like tissue regeneration. Stem Cell Research & Therapy 7 (1): 168.
Hu, J., C. Yu, Y. Xie, et al. 2016. Periodontal regeneration in swine after cell injection and cell sheet transplantation of human dental pulp stem cells following good manufacturing practice. Stem Cell Research & Therapy 7 (1): 130.
Su, F., S.S. Liu, J.L. Ma, et al. 2015. Enhancement of periodontal tissue regeneration by transplantation of osteoprotegerin-engineered periodontal ligament stem cells. Stem Cell Research & Therapy 6 (1): 1–14.
Choung, P.H., H. Jin, B. Jin, et al. 2015. Recombinant human plasminogen activator inhibitor-1 induces cementogenic differentiation of human periodontal ligament stem cells. Tissue Engineering. Part A 21 (23–24).
Garlet, G.P. 2010. Destructive and protective roles of cytokines in periodontitis: A re-appraisal from host defense and tissue destruction viewpoints. Journal of Dental Research 89 (12): 1349–1363.
Cekici, A., A. Kantarci, H. Hasturk, and T.E. Van Dyke. 2014. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontology 64 (1): 57–80.
Zhou, R., L. Shen, C. Yang, et al. 2018. Periodontitis may restrain the mandibular bone healing via disturbing osteogenic and osteoclastic balance. Inflammation 1: 1–12.
Wang, Nan, Zubin Zhou, Tianyi Wu, Wei Liu, Peipei Yin, Chenhao Pan, and Xiaowei Yu. 2016. TNF-α-induced NF-κB activation upregulates microRNA-150-3p and inhibits osteogenesis of mesenchymal stem cells by targeting β-catenin. Open Biology 6 (3): 150258.
Qin, Z., Z. Fang, Z. Lei, et al. 2015. High dose of TNF-α suppressed osteogenic differentiation of human dental pulp stem cells by activating the Wnt/β-catenin signaling. Journal of Molecular Histology 46 (4–5): 409–420.
Wang, L.M., N. Zhao, J. Zhang, et al. 2017. Tumor necrosis factor-alpha inhibits osteogenic differentiation of pre-osteoblasts by downregulation of EphB4 signaling via activated nuclear factor-kappaB signaling pathway. Journal of Periodontal Research 53 (1).
Huang, H., N. Zhao, X. Xu, Y. Xu, S. Li, J. Zhang, and P. Yang. 2011. Dose-specific effects of tumor necrosis factor alpha on osteogenic differentiation of mesenchymal stem cells. Cell Proliferation 44 (5): 420–427.
Mukai, T., F. Otsuka, H. Otani, M. Yamashita, K. Takasugi, K. Inagaki, M. Yamamura, and H. Makino. 2007. TNF-alpha inhibits BMP-induced osteoblast differentiation through activating SAPK/JNK signaling. Biochemical and Biophysical Research Communications 356 (4): 1004–1010.
Feng, J.Q., F.J. Guo, B.C. Jiang, Y. Zhang, S. Frenkel, D.W. Wang, W. Tang, Y. Xie, and C.J. Liu. 2010. Granulin epithelin precursor: A bone morphogenic protein 2-inducible growth factor that activates ERK1/2 signaling and JunB transcription factor in chondrogenesis. FASEB Journal 24 (6): 1879–1892.
He, Z., C.H. Ong, J. Halper, and A. Bateman. 2003. Progranulin is a mediator of the wound response. Nature Medicine 9 (2): 225–229.
Guo, Z., Li, Q., Han, Y., et al. 2012. Prevention of LPS-induced acute lung injury in mice by progranulin. Mediators of Inflammation 2012,(2012-8-15), 2012(962–9351): 540794.
Yin, F., R. Banerjee, B. Thomas, P. Zhou, L. Qian, T. Jia, X. Ma, Y. Ma, C. Iadecola, M.F. Beal, C. Nathan, and A. Ding. 2010. Exaggerated inflammation, impaired host defense, and neuropathology in progranulin-deficient mice. Journal of Experimental Medicine 207 (1): 117–128.
Tang, W., Y. Lu, Q.Y. Tian, Y. Zhang, F.J. Guo, G.Y. Liu, N.M. Syed, Y. Lai, E.A. Lin, L. Kong, J. Su, F. Yin, A.H. Ding, A. Zanin-Zhorov, M.L. Dustin, J. Tao, J. Craft, Z. Yin, J.Q. Feng, S.B. Abramson, X.P. Yu, and C.J. Liu. 2011. The growth factor progranulin binds to TNF receptors and is therapeutic against inflammatory arthritis in mice. Science 332 (6028): 478–484.
Zhao, Y.P., Q.Y. Tian, S. Frenkel, and C.J. Liu. 2013. The promotion of bone healing by progranulin, a downstream molecule of BMP-2, through interacting with TNF/TNFR signaling. Biomaterials 34 (27): 6412–6421.
Noguchi, T., K. Ebina, M. Hirao, R. Kawase, T. Ohama, S. Yamashita, T. Morimoto, K. Koizumi, K. Kitaguchi, H. Matsuoka, S. Kaneshiro, and H. Yoshikawa. 2015. Progranulin plays crucial roles in preserving bone mass by inhibiting TNF-α-induced osteoclastogenesis and promoting osteoblastic differentiation in mice. Biochemical & Biophysical Research Communications 465 (3): 638–643.
Zhao, Yunpeng, Ben Liu, Qingyun Tian, Jian-lu Wei, Brendon Richbourgh, and Chuan-ju Liu. 2015. Progranulin protects against osteoarthritis through interacting with TNF-α and β-catenin signalling. Annals of the Rheumatic Diseases 74 (12): 2244–2253.
Lehmann, N., T. Christ, A. Daugs, O. Bloch, and S. Holinski. 2017. EDC-crosslinking of decellularized tissue-a promising approach? Tissue Engineering Part A 23 (13): 675–682.
Chen, S., Xin, Y., Yu, X., Xu, Q., Pan, K., et al. 2015. Co-culture with periodontal ligament stem cells enhanced osteoblastic differentiation of MC3T3-E1 cells and osteoclastic differentiation of RAW264.7 cells. International Journal of Clinical & Experimental Pathology, 8(11): 14596.
Fentoğlu, O., F.Y. Kirzioğlu, M. Ozdem, et al. 2012. Proinflammatory cytokine levels in hyperlipidemic patients with periodontitis after periodontal treatment. Oral Diseases 18 (3): 299–306.
Graves, D.T., A.J. Delima, R. Assuma, S. Amar, T. Oates, and D. Cochran. 1998. Interleukin-1 and tumor necrosis factor antagonists inhibit the progression of inflammatory cell infiltration toward alveolar bone in experimental periodontitis. Journal of Periodontology 69 (12): 1419–1425.
Xin, Y., H. Huang, Z. Ning, Z. Jin, and P. Yang. 2016. Inhibition of Runx2 signaling by TNF-α in ST2 murine bone marrow stromal cells undergoing osteogenic differentiation. Vitro Cellular & Developmental Biology - Animal 52 (10): 1–8.
Delima, A.J., T. Oates, R. Assuma, et al. 2010. Soluble antagonists to interleukin-1 (IL-1) and tumor necrosis factor (TNF) inhibits loss of tissue attachment in experimental periodontitis. Journal of Clinical Periodontology 28 (3): 233–240.
Redlich, K., and J.S. Smolen. 2012. Inflammatory bone loss: Pathogenesis and therapeutic intervention. Nature Reviews Drug Discovery 11 (3): 234–250.
Li, X., Z. Zuo, Q. Chen, et al. 2018. Progranulin is highly expressed in patients with chronic periodontitis and protects against experimental periodontitis in rats. J Periodontol . 2018 Jul 12. https://doi.org/10.1002/JPER.18-0132 [Epub ahead of print].
Kobayashi, K., N. Takahashi, E. Jimi, N. Udagawa, M. Takami, S. Kotake, N. Nakagawa, M. Kinosaki, K. Yamaguchi, N. Shima, H. Yasuda, T. Morinaga, K. Higashio, T.J. Martin, and T. Suda. 2000. Tumor necrosis factor α stimulates osteoclast differentiation by a mechanism independent of the Odf/Rankl–Rank interaction. Journal of Experimental Medicine 191 (2): 275–286.
Lam, J., S. Takeshita, J.E. Barker, O. Kanagawa, F.P. Ross, and S.L. Teitelbaum. 2000. TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. Journal of Clinical Investigation 106 (12): 1481–1488.
Assuma, R., T. Oates, D. Cochran, S. Amar, and D.T. Graves. 1998. IL-1 and TNF antagonists inhibit the inflammatory response and bone loss in experimental periodontitis. J immunol 160: 403–409 160 (1): 403–409.
Wang, N., Z. Zhou, T. Wu, W. Liu, P. Yin, C. Pan, and X. Yu. 2016. TNF-α-induced NF-κB activation upregulates microRNA-150-3p and inhibits osteogenesis of mesenchymal stem cells by targeting β-catenin. Open Biol 6: 150258.
Zhao, Y.P., J.L. Wei, Q.Y. Tian, A.T. Liu, Y.S. Yi, T.A. Einhorn, and C.J. Liu. 2016. Progranulin suppresses titanium particle induced inflammatory osteolysis by targeting TNFα signaling. Scientific Reports 6: 20909.
Wahl, E.C., J. Aronson, L. Liu, R.A. Skinner, M.J. Miller, G.E. Cockrell, J.L. Fowlkes, K.M. Thrailkill, R.C. Bunn, M.J.J. Ronis, and C.K. Lumpkin Jr. 2010. Direct bone formation during distraction osteogenesis does not require TNFα receptors and elevated serum TNFα fails to inhibit bone formation in TNFR1 deficient mice. Bone 46 (2): 410–417.
Acknowledgments
Pishan Yang and Chengzhe Yang contributed equally to this research to be as corresponding authors.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Nos. 81771076, 81702684), Beijing, China, and the Construction Engineering Special Fund of “Taishan Scholars,” Jinan, China.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, Q., Cai, J., Li, X. et al. Progranulin Promotes Regeneration of Inflammatory Periodontal Bone Defect in Rats via Anti-inflammation, Osteoclastogenic Inhibition, and Osteogenic Promotion. Inflammation 42, 221–234 (2019). https://doi.org/10.1007/s10753-018-0886-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-018-0886-4