Abstract
Whether critically ill human immunodeficiency virus (HIV)-infected patients are at risk of acquiring nosocomial infections and resistant or potentially resistant microorganisms (RPRMs) remains to be clarified. The aim was to compare the acquisition of RPRMs, infections and mortality in critically ill HIV-infected and non-infected patients. An observational, prospective cohort study of patients admitted to a medical intensive care unit (ICU) was undertaken. Swabbing of nares, pharynx and rectum, and culture of respiratory secretions were obtained within 48 h of admission and thrice weekly thereafter. Clinical samples were obtained as deemed necessary by the attending physician. Clinical variables, severity scores on admission and exposures during ICU stay were collected. Logistic regression was used to evaluate ICU mortality. Out of the 969 included patients, 64 (6.6 %) were HIV-infected. These patients had a higher Acute Physiology and Chronic Health Evaluation (APACHE) II score on admission (19.5 ± 6.6 vs. 21.1 ± 5.4, p = 0.02), stayed longer in the care unit and were more exposed to several invasive devices and antibiotics. There were no differences in the rate of acquisition of RPRMs and the only difference in ICU-acquired infections was a significantly higher incidence of catheter-related bacteraemia (3 % vs. 9 %, p = 0.03). The ICU-related mortality was similar in both groups (14 % vs. 16 %, p = 0.70) and in HIV-infected patients, it tended to be associated with a lower CD4 cell count (p = 0.06). Despite a longer ICU stay, critically ill HIV-infected patients did not show a higher rate of RPRMs acquisition. The rate of ICU-acquired infection was similar between HIV-infected and non-infected patients, except for catheter-related bacteraemia, which was higher in the HIV-infected population. Mortality was similar in both groups.
Similar content being viewed by others
Introduction
Since the advent of the potent combination of antiretroviral therapy (ART) in 1996, several studies have reported an increased admission rate of human immunodeficiency virus (HIV)-infected patients to the intensive care unit (ICU), as well as a better survival. It has been estimated that 4–12 % of hospitalised HIV-infected patients require ICU care. The reasons for admission have also changed, being less often related to opportunistic infections and more to problems unrelated to HIV infection [1, 2]. In some series, more than half of ICU admissions were for non-HIV-related critical illnesses [1–7]. These patients may also require critical care due to other co-morbidities. such as hepatitis or chronic obstructive pulmonary disease (COPD) [3, 4].
The extent to which HIV-infected patients in comparison to other critically ill medical patients behave regarding the acquisition of nosocomial infections and resistant or potentially resistant microorganisms (RPRMs) remains to be clarified. In addition to the characteristic cellular immune dysfunction, HIV-infected patients present other immune disturbances, such as inadequate humoral immunity, abnormal chemotaxis, phagocytosis and bactericidal activity, as well as a higher rate of colonisation by Staphylococcus aureus, which may lead to an increased susceptibility to bacterial infections inside the ICU [8, 9]. In fact, immunosuppression is often considered to be a risk factor of acquiring infections by resistant organisms and poor prognosis [10].
The main objective of this study was to compare the ICU acquisition of RPRMs, infections and mortality in critically ill HIV-infected and non-HIV-infected patients.
Materials and methods
Study population
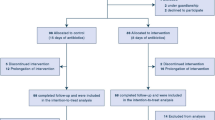
From February 14th, 2006 to December 31st, 2008, all patients admitted to an eight-bed adult medical ICU of a 700-bed university hospital who stayed in the unit for at least 24 h were prospectively included in the study. The study protocol was approved by the Research Ethics Committee of the Hospital Clinic of Barcelona.
Data collection and definitions
Swabbing of nares, pharynx and rectum, and culture of respiratory secretions (tracheobronchial aspirates or sputum) were obtained within 48 h of admission and thrice weekly thereafter until discharge or the first two months of ICU stay. Other clinical samples were obtained as deemed necessary by the attending physician. No environmental cultures were taken. Susceptibility testing was done by a microdilution technique according to the Clinical and Laboratory Standards Institute (CLSI) guidelines [11]. For the purpose of analysis, intermediate susceptibility was considered as resistance.
The following microorganisms were considered as RPRMs: methicillin-resistant S. aureus (MRSA), vancomycin-resistant enterococci, enteric Gram-negative bacilli resistant to third-generation cephalosporins (cefotaxime, ceftazidime or both) and non-fermentative Gram-negative bacilli (Pseudomonas aeruginosa, Burkholderia cepacia, Stenotrophomonas maltophilia and Acinetobacter baumannii) [11].
Demographics, clinical variables, severity scores (APACHE II: Acute Physiology and Chronic Health Evaluation; APS: Acute Physiology Score; SOFA: Sequential Organ Failure Assessment) on admission and exposures during ICU stay were prospectively collected from all admitted patients [12–14]. From HIV-infected patients, specific data about ART, and the most recent CD4 cell count and plasma HIV RNA viral load were also recorded. The primary outcome variables were the acquisition of RPRMs and infections during ICU stay, as well as mortality.
Patients with positive surveillance cultures within 48 h of ICU admission were considered to be colonised on admission. Colonisation was defined as the isolation of a target microorganism from a surveillance culture or non-sterile clinical sample. Microorganisms isolated after 48 h in patients with previous negative specimens for those bacteria were considered as ICU-acquired. Infections diagnosed within 48 h of admission were considered as being of non-ICU origin and those diagnosed after 48 h as ICU-acquired. Exposure to antibiotics meant at least 24 h of treatment.
In our institution, HIV infection was not, by itself, a reason for denial of ICU admission to patients requiring critical care. Patients not suspected to be HIV-infected in whom a specific test for the diagnosis of HIV infection was not deemed necessary by the attending physician were considered as non-HIV-infected. Prior ART use was defined as receiving at least two types of antiretroviral drugs at the time of hospital admission [15].
Infection was considered the reason for admission when the organic failure leading to critical care was meant to be a direct consequence of either the dysfunction of the infected organ or sepsis. Septic shock was defined according to the SCCM/ESICM/ACCP/ATS/SIS consensus conference [16]. ICU-acquired sepsis was defined as sepsis occurring more than 48 h after admission to the ICU. Catheter-related bacteraemia was defined according to the Infectious Diseases Society of America (IDSA) guidelines [17]. The diagnosis of pneumonia required the presence of new and/or progressive infiltrates on chest radiographs, and at least two of the following criteria: fever ≥38 °C or hypothermia ≤35 °C, leucocytosis ≥12,000/μL or leucopaenia <4,000/μL, or purulent respiratory secretions. When the patient was invasively ventilated for more than 48 h, pneumonia was considered ventilator-associated pneumonia (VAP) [18]. Patients without radiological criteria of pneumonia but fulfilling the above-mentioned clinical criteria were considered to have tracheobronchitis. The diagnosis of Pneumocystis jirovecii pneumonia was based on the identification of Pneumocystis in bronchoalveolar lavage fluid [19]. Other infections were diagnosed according to the Centers for Disease Control and Prevention (CDC) criteria [20].
Statistical analysis
Clinical variables and exposures were compared between HIV-infected and non-HIV-infected patients. Proportions were compared by using the χ2 or Fisher’s exact test. Continuous variables were compared by using the t-test (or Mann–Whitney test) and analysis of variance (ANOVA) (or Kruskal–Wallis test). Correlations between continuous variables were assessed by the non-parametric Spearman correlation coefficient. Multivariable logistic regression analysis (step-forward procedure) was used to evaluate patient characteristics associated with ICU mortality. In these models, potential explanatory variables included age, gender, diagnosis at admission, HIV status, lymphoma, cirrhosis, diabetes, previous corticosteroids, other previous immunosuppressors, previous antibiotics, septic shock on admission, APACHE II and SOFA scores on admission, orotracheal intubation (as a marker of invasive devices), corticosteroids and immunosuppressors during ICU stay, enteral and parenteral nutrition, exposure to selected antibiotics (antipseudomonal agents, trimethoprim–sulfamethoxazole, non-antipseudomonal third-generation cephalosporins), status of having on admission or acquiring an RPRM during ICU stay and having a clinical infection on admission or acquiring one during ICU stay. Variables with a p-value <0.3 in the univariate analysis were introduced in the multivariate model. During analysis, a significant interaction between the APACHE II score and having a haematological malignancy (HM) was found, meaning that mortality in these particular patients was much less associated with an increasing APACHE score than in other patients. In order to address this interaction, the APACHE score was dichotomised by the median of the entire population (19 points) and a logistic model was built in which an interaction “APACHE by HM” variable stratified in four categories (“low APACHE and non-HM”, “low APACHE and HM”, “high APACHE and HM”, “high APACHE and non-HM”) was introduced. Calculations were done by using the SPSS version 17.0 statistical package. p-values less than 0.05 were considered statistically significant.
Results
Demographic and clinical characteristics
During the 35-month study period, 969 patients were admitted to the ICU, of which 64 (6.6 %) were HIV-infected. The clinical and epidemiological characteristics on admission are shown in Table 1. Compared with non-HIV-infected patients, those with HIV infection were significantly younger (the mean age was 45.2 vs. 61 years), more frequently were smokers, had an alcohol and intravenous drug addiction, more often had cirrhosis, had more infections in the last year and had more frequently received antibiotics in the previous month. On the other hand, non-HIV-infected patients more often had diabetes, heart failure and COPD. HIV-infected patients were more frequently admitted to the unit due to an infection and presented a higher prevalence of septic shock. They were also more severely ill with higher APACHE II and APS scores, even though the SOFA score was similar to non-HIV-infected patients.
The median [interquartile range (IQR)] pre-admission CD4 cell count and viral load were 200 cells/μL (78–392) and 2,752 HIV RNA copies/mL (0–59,054), respectively, and there was a modest but significant negative correlation between these two variables (Spearman R = −0.29, p = 0.02). In the present study, 44 (69 %) patients were under ART before admission (12 for less than six months and 32 for more than six months). Pre-admission receipt of ART was not significantly associated with the CD4 cell count (median 208 cells/μL, IQR = 101–399, in patients with ART vs. 158, IQR = 28–389, in those without ART, p = 0.2), but it was strongly associated with the viral load (median 100 copies/mL, IQR = 0–3,589, in patients with ART vs. 111,350, IQR = 23,061–325,550, in those without ART, p < 0.001). Pre-admission CD4 count or HIV viraemia was not associated to the previous time a patient was under ART. Sixteen (25 %) patients under ART received it during ICU admission, while it was temporally discontinued in the remaining patients, mainly due to difficulty in oral administration or intestinal absorption.
The reasons for admission of HIV-infected patients are shown in Table 2. Among the 49 patients admitted with an infection (77 % of cases), the most prevalent diagnosis was pneumonia (n = 33, 52 %). Pneumonia was due to P. jirovecii in six patients (three of which required intubation and died) and in two due to cytomegalovirus, one with P. jirovecii as a co-pathogen and another with P. aeruginosa. Six patients had meningitis, of which two were caused by Cryptococcus neoformans. One patient presented Guillain–Barré syndrome associated with cytomegalovirus infection and two patients had ART toxicity. A total of 12 (19 %) patients were admitted for reasons directly related to HIV infection.
Exposures during ICU stay
During admission, patients with HIV infection were significantly exposed for longer to central venous, arterial and urinary catheters, nasogastric tube, parenteral nutrition, corticosteroids, orotracheal intubation, mechanical ventilation and to certain antibiotics, such as clindamycin, piperacillin–tazobactam, trimethoprim–sulfamethoxazole, levofloxacin, non-antipseudomonal cephalosporins and fluconazole (Table 3).
Outcomes
Methicillin-susceptible S. aureus colonisation was more frequently recorded on admission in HIV-infected patients (11 [17 %] vs. 68 [8 %] in non-HIV patients, p = 0.01). However, no acquisition of methicillin-susceptible S. aureus was observed in this population during their ICU stay (0 vs. 3.1 % in non-HIV patients, p = 0.3) and no infections due to this microorganism were diagnosed. There were no differences in the rate of RPRMs neither at admission nor during the patient’s stay in the unit. Regarding ICU-acquired infections, the only difference observed was a significantly higher incidence of catheter-related bacteraemia in HIV-infected patients (Table 4), which was due to Gram-positive cocci in all cases (five episodes caused by S. epidermidis and one by E. faecium). The median length of stay in the ICU was longer in patients with HIV infection (8 vs. 5 days, p = 0.0009).
In HIV-infected patients, the ICU and hospital mortality were 16 % (10 out of 64 patients) and 28 % (18 out of 64 patients), respectively, and none of these rates were significantly different to those of non-HIV-infected patients (Table 1).
Multivariate analysis showed that having a haematological malignancy with an APACHE II score >19 [odds ratio (OR) 4.59, 2.45–8.63] or ≤19 (OR 9.64, 3–31), an APACHE II score >19 with a non-haematological malignancy condition (OR 3.7, 1.37–9.96), SOFA score (OR 2.21, 1.12–1.29, per increasing point), having bacteraemia of an unknown source on admission (OR 6.1, 1.27–27.1), admission (taking postoperative care/other diagnosis as the reference) due to a respiratory (OR 11.8, 3.21–43.7), cardiovascular (OR 3.06, 1–9.61), infectious (OR 5.6, 2.06–15.2) and neurological (OR 4.99, 1.68–14.8) disease, orotracheal intubation (OR 11.3, 4.98–25.6), receipt of corticosteroids other than hydrocortisone (OR 2.33, 1.33–4.08) during ICU stay, need for renal replacement therapy (OR 2.33, 1.23–4.41), administration of any anti-Aspergillus antifungals (OR 3.37, 1.6–7.1) and administration of linezolid (OR 2.86, 1.23–6.65) were independent predictors of mortality, whereas receipt of antipseudomonal antibiotics (OR 0.25, 0.13–0.47) and non-antipseudomonal third-generation cephalosporins (OR 0.49, 0.27–0.89) were protective. HIV infection, having on admission or acquiring an RPRM during ICU stay and having a clinical infection on admission or acquiring one during ICU stay were not selected as independent predictors of mortality.
HIV-infected patients who died in the ICU had a non-significant trend towards having a lower CD4 cell count than that of those who survived (median 82 cells/μL, IQR = 36–232, vs. 208, IQR = 89–422, p = 0.06). The length of ICU stay tended to be negatively correlated with the CD4 cell count, without reaching statistical significance (Spearman R = −0.21, p = 0.08). In regards to the ICU acquisition of RPRMs, HIV-infected patients who acquired P. aeruginosa had a significantly lower CD4 cell count (median 78 cells/μL, IQR 36–200) than that of those who did not acquire this microorganism (median 208 cells/μL, IQR 90–420, p = 0.04) and also showed a non-significant trend towards having a higher viral load (median 22,381 copies/mL, IQR 1,995–256,200 vs. median 1,500, IQR 0–37,857, p = 0.1). It is of note, however, that the three patients who acquired VAP due to P. aeruginosa had a CD4 cell count ranging from 294 to 578 cells/μL. The ICU acquisition of other RPRMs, development of in-ICU clinical infections and overall hospital mortality were neither significantly associated with the CD4 cell count nor viral load (p > 0.2 for all comparisons, data not shown). Receiving ART before admission was not associated with the acquisition of RPRMs, ICU-acquired infections or ICU mortality (p > 0.3 for all comparisons, data not shown).
Discussion
The main finding of our study was that, in the ICU setting, HIV-infected patients presented a similar risk of acquiring RPRMs or infections as patients without HIV infection, with the exception of catheter-related bacteraemia. In addition, prognosis was neither related to HIV infection nor to the acquisition of RPRMs or infections during ICU stay.
In the present study, HIV-infected patients admitted to the ICU had several demographic and clinical characteristics different from non-HIV-infected patients, such as younger age, male gender predominance and a higher prevalence of smoking, alcohol and intravenous drug addiction, lymphoma, liver cirrhosis, and infection and septic shock on admission. On the other hand, non-HIV-infected patients more often had diabetes and COPD, which may be related to the fact that they were older. These differential traits were not unexpected and respond to the epidemiologic characteristics of HIV infection in developed countries. Men account for 71 % of new HIV infections, two-thirds from homosexual contact and 15–20 % from heterosexual contact. In both men and women, approximately 20 % of new infections are due to intravenous drug use [21]. Besides an increased frequency of lymphoma, non-Hodgkin’s lymphoma, cervical cancer and anal cancer (in both men and women) also occur much more frequently in HIV-positive than in HIV-negative individuals [22, 23]. HIV-infected patients are also more susceptible to severe liver injury and progression of cirrhosis, especially in the setting of co-infection with viral hepatitis and alcohol use [24].
In this study, septic shock at ICU admission was also observed more frequently among HIV-infected patients, probably due to the fact that the main reason for admission was bacterial infections, which contrasts with what happened before the advent of highly active ART when opportunistic infections were the most frequent cause for ICU admission [25]. In the present study, only 12 (19 %) patients were admitted with a condition directly related to HIV infection (six P. jirovecii pneumonia, one CMV pneumonia, one miliary tuberculosis, two cryptococcal meningitis and two ART severe adverse events), a rate which is even lower than the figure of 34 % reported in one recent study [26]. The association between sepsis and a higher rate of mortality in the critically ill HIV-AIDS population has been shown in previous studies [27, 28]. It has been estimated that sepsis is a major determinant of 28-day and 6-month mortality in HIV-infected patients admitted to the ICU (adjusted HR 3.13 and 3.35, respectively) [28]. However, our data show that to be admitted due to an infection was an independent predictor of ICU mortality for all patients and, therefore, not just limited to the HIV-infected population. It has also been reported that pneumonia is the most common infection that needs admission to the ICU (52–55.6 %), which is in accordance to the 52 % pneumonia rate observed in our cohort. In the present study, 9 % of HIV-infected patients had P. jirovecii pneumonia (Table 2), a prevalence which is in the lower range of that reported in previous studies (3–25 %) [5, 6, 26]. However, mortality among these patients remains very high, as it was corroborated in our study, since three out of six patients (50 %) required mechanical ventilation and died . Similarly to previous studies, approximately 23 % of patients were admitted for reasons not related to an infection [5, 26].
There are relatively few data concerning the predisposition of HIV-infected patients to acquire RPRMs and infections during admission to a medical ICU. It is of note that we did not find that HIV-infected patients were significantly more colonised with this type of microorganism on admission. An increased rate of RPRMs would have been expected, since this population had been more frequently exposed to antibiotics within the previous month and had more infections during the last year. In addition, although patients with HIV infection stayed for longer in the ICU and were more frequently and/or exposed for longer to steroids, orotracheal intubation and other invasive devices, as well as to several antibiotics, the rate of acquisition of RPRMs was not significantly higher. The only ICU-acquired infection that was more prevalent among HIV-infected patients was catheter-related bacteraemia. The explanation for these findings is unclear; however, it might be attributed to the prophylactic effect of increased exposure to antibiotics such as trimethoprim–sulfamethoxazole or antipseudomonal agents. The prophylactic activity of antibiotics, in particular quinolones, against the acquisition of ampC-producing enteric Gram-negative bacilli and P. aeruginosa had been previously described [29, 30]. On the other hand, the higher incidence of catheter-related bacteraemia may be due to the fact that these patients had more often several central venous catheters (probably associated to the higher rate of septic shock at admission), received more frequently parenteral nutrition and their stay in the unit was longer. Other studies have shown that the central venous catheter is a major cause of bacteraemia in this population [31, 32]. An increased rate of methicillin-susceptible S. aureus colonisation on admission was also observed in the present study [8, 9], but no infections due to these microorganisms were diagnosed in HIV-infected patients. Our finding of a significant association between the ICU acquisition of P. aeruginosa and a lower CD4 cell count may be consistent with previous studies documenting that a low CD4 cell count (usually below 50/μL) was an independent risk factor for infection due to P. aeruginosa in this population [33, 34].
In regards to prognosis, the overall and ICU mortality were similar in both groups. This similarity occurred despite the fact that HIV-infected patients had a higher prevalence of factors associated with ICU mortality, such as longer intubation, infection diagnosis on admission and higher APACHE II scores. The explanation for this finding may lay on a greater exposure to protective factors such as antipseudomonal antibiotics or third-generation cephalosporins, which suggest that the eventual untoward impact of sepsis on survival can be lessened by the corresponding use of appropriate antimicrobial therapy. We did not find that the acquisition of RPRMs or infections during ICU stay were independent predictors of ICU mortality. The extent to which ICU-acquired infections in general or those due to resistant microorganisms in particular increase mortality beyond what would be expected on the basis of severity of illness is still a matter of controversy. Studies that did not find an independent association of ICU-acquired infections (including those due to RPRMs) with mortality are not exceptional in the critical care literature [35–37]. In addition, there is evidence that, when appropriate multistate or causal inference models are applied, the attributable mortality of ICU-acquired infections such as VAP may be lower than previously estimated (in the range of 4–8 %) [38, 39]. In any case, timely and appropriate antibiotic therapy is likely to be a modifying factor that may render the attributable mortality of ICU-acquired infections almost negligible [40]. The independent association of some antibiotic exposures with mortality deserves comment. When the administration of a given drug is associated with death, it may be quite difficult to establish whether this was due to a deleterious effect of the drug or just the result of preferentially administering that therapy to sicker patients. We think that the independent association of anti-Aspergillus antifungals with death belongs to the latter category. However, the observation that linezolid was associated with ICU mortality raises concern. In a clinical trial on patients with catheter-related bacteraemia, linezolid was associated with increased mortality in the subset of patients with no pathogens at baseline [41]. In a recent case–control study of critically ill patients, a non-significant trend toward increased mortality in those with renal insufficiency receiving linezolid was noted [42]. Further studies, therefore, are necessary to provide a definite answer to this relevant question.
In HIV-infected patients, we noted a non-significant trend towards the association of a lower CD4 cell count with an increased mortality and length of ICU stay. These observations are consistent with the results of previous studies showing an association of low CD4 cell counts with increased mortality, although the finding that, in the critical care setting, it is an independent predictor of mortality remains elusive [43–45].
While early initiation of ART has shown to improve survival in patients with AIDS-related opportunistic infections [7], it remains questionable as to whether ART should be started during ICU stay due to issues of toxicity, bioavailability and drug interactions [3].
The present study has some common drawbacks of observational studies performed in a single institution with a limited number of participants, such as a low power to detect significant differences, difficulties in establishing causal relationships and the limitations when trying to apply results to other epidemiological scenarios. However, its strength resides on the frequent and thorough sampling method, allowing an accurate detection of the acquisition of RPRMs during ICU stay.
In conclusion, critically ill HIV-infected patients admitted to our ICU did not show a higher rate of RPRMs acquisition. The only most frequently acquired infection was catheter-related bacteraemia and mortality was similar in HIV-infected and non-infected patients.
References
Akgün KM, Pisani M, Crothers K (2011) The changing epidemiology of HIV-infected patients in the intensive care unit. J Intensive Care Med 26:151–164
Castro Rebollo P, Nicolás JM, Gatell JM (2007) HIV in the intensive care unit. In: Rello J, Kollef MH, Díaz E, Rodríguez A (eds) Infectious diseases in critical care, 2nd edn. Springer-Verlag, Berlin Heidelberg New York, pp 51–62
Huang L, Quartin A, Jones D et al (2006) Intensive care of patients with HIV infection. N Engl J Med 355:173–181
Crothers K, Huang L, Goulet JL et al (2011) HIV infection and risk for incident pulmonary diseases in the combination antiretroviral therapy era. Am J Respir Crit Care Med 183:388–395
Chiang H-H, Hung C-C, Lee C-M et al (2011) Admissions to intensive care unit of HIV-infected patients in the era of highly active antiretroviral therapy: etiology and prognostic factors. Crit Care 15:R202
Casalino E, Wolff M, Ravaud P et al (2004) Impact of HAART advent on admission patterns and survival in HIV-infected patients admitted to an intensive care unit. AIDS 18:1429–1433
Zolopa A, Andersen J, Powderly W et al (2009) Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PLoS One 4:e5575
Nguyen MH, Kauffman CA, Goodman RP et al (1999) Nasal carriage of and infection with Staphylococcus aureus in HIV-infected patients. Ann Intern Med 130:221–225
Padoveze MC, de Jesus Pedro R, Blum-Menezes D et al (2008) Staphylococcus aureus nasal colonization in HIV outpatients: persistent or transient? Am J Infect Control 36:187–191
American Thoracic Society; Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Clinical and Laboratory Standards Institute (CLSI) (2009) Performance standards for antimicrobial susceptibility testing; Nineteenth informational supplement. CLSI document M100–S19. CLSI, Wayne
Martínez JA, Nicolás JM, Marco F et al (2006) Comparison of antimicrobial cycling and mixing strategies in two medical intensive care units. Crit Care Med 34:329–336
Knaus WA, Draper EA, Wagner DP et al (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Department of Health and Human Services, Panel on Antiretroviral Guidelines for Adults and Adolescents, Office of AIDS Research Advisory Council. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents, 2007. Available online at: http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf
Levy MM, Fink MP, Marshall JC et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Mermel LA, Allon M, Bouza E et al (2009) Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 49:1–45
Ruiz M, Torres A, Ewig S et al (2000) Noninvasive versus invasive microbial investigation in ventilator-associated pneumonia: evaluation of outcome. Am J Respir Crit Care Med 162:119–125
Thomas CF Jr, Limper AH (2004) Pneumocystis pneumonia. N Engl J Med 350:2487–2498
Garner JS, Jarvis WR, Emori TG et al (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–140
Centers for Disease Control and Prevention (CDC) (2007) HIV/AIDS surveillance report, 2005. Vol. 17. Rev ed. CDC, Atlanta, pp 16-1
Mbulaiteye SM, Biggar RJ, Goedert JJ et al (2003) Immune deficiency and risk for malignancy among persons with AIDS. J Acquir Immune Defic Syndr 32:527–533
Petroll AE, Hare CB, Pinkerton SD (2008) The essentials of HIV: a review for nurses. J Infus Nurs 31:228–235
Puoti M, Spinetti A, Ghezzi A et al (2000) Mortality for liver disease in patients with HIV infection: a cohort study. J Acquir Immune Defic Syndr 24:211–217
Schein RM, Fischl MA, Pitchenik AE et al (1986) ICU survival of patients with the acquired immunodeficiency syndrome. Crit Care Med 14:1026–1027
Adlakha A, Pavlou M, Walker DA et al (2011) Survival of HIV-infected patients admitted to the intensive care unit in the era of highly active antiretroviral therapy. Int J STD AIDS 22:498–504
Coquet I, Pavie J, Palmer P et al (2010) Survival trends in critically ill HIV-infected patients in the highly active antiretroviral therapy era. Crit Care 14:R107
Japiassú AM, Amâncio RT, Mesquita EC et al (2010) Sepsis is a major determinant of outcome in critically ill HIV/AIDS patients. Crit Care 14:R152
Schwaber MJ, Cosgrove SE, Gold HS et al (2004) Fluoroquinolones protective against cephalosporin resistance in gram-negative nosocomial pathogens. Emerg Infect Dis 10:94–99
Martínez JA, Delgado E, Martí S et al (2009) Influence of antipseudomonal agents on Pseudomonas aeruginosa colonization and acquisition of resistance in critically ill medical patients. Intensive Care Med 35:439–447
Petrosillo N, Viale P, Nicastri E et al (2002) Nosocomial bloodstream infections among human immunodeficiency virus-infected patients: incidence and risk factors. Clin Infect Dis 34:677–685
Ortega M, Almela M, Soriano A et al (2008) Bloodstream infections among human immunodeficiency virus-infected adult patients: epidemiology and risk factors for mortality. Eur J Clin Microbiol Infect Dis 27:969–976
Meynard JL, Barbut F, Guiguet M et al (1999) Pseudomonas aeruginosa infection in human immunodeficiency virus infected patients. J Infect 38:176–181
Vidal F, Mensa J, Martínez JA et al (1999) Pseudomonas aeruginosa bacteremia in patients infected with human immunodeficiency virus type 1. Eur J Clin Microbiol Infect Dis 18:473–477
Soufir L, Timsit JF, Mahe C et al (1999) Attributable morbidity and mortality of catheter-related septicemia in critically ill patients: a matched, risk-adjusted, cohort study. Infect Control Hosp Epidemiol 20:396–401
Peres-Bota D, Rodriguez H, Dimopoulos G et al (2003) Are infections due to resistant pathogens associated with a worse outcome in critically ill patients? J Infect 47:307–316
Shorr AF (2009) Review of studies of the impact on Gram-negative bacterial resistance on outcomes in the intensive care unit. Crit Care Med 37:1463–1469
Timsit JF, Zahar JR, Chevret S (2011) Attributable mortality of ventilator-associated pneumonia. Curr Opin Crit Care 17:464–471
Bekaert M, Timsit JF, Vansteelandt S et al (2011) Attributable mortality of ventilator-associated pneumonia: a reappraisal using causal analysis. Am J Respir Crit Care Med 184:1133–1139
Agrafiotis M, Siempos II, Ntaidou TK et al (2011) Attributable mortality of ventilator-associated pneumonia: a meta-analysis. Int J Tuberc Lung Dis 15:1154–1163
Wilcox MH, Tack KJ, Bouza E et al (2009) Complicated skin and skin-structure infections and catheter-related bloodstream infections: noninferiority of linezolid in a phase 3 study. Clin Infect Dis 48:203–212
Sterzik H, Soriano A, Mohamad AM et al (2011) Is linezolid a risk factor for Gram-negative bacillus infections in intensive care unit patients? A comparative study with vancomycin. Scand J Infect Dis 43:765–770
Dickson SJ, Batson S, Copas AJ et al (2007) Survival of HIV-infected patients in the intensive care unit in the era of highly active antiretroviral therapy. Thorax 62:964–968
Alves C, Nicolás JM, Miró JM et al (2001) Reappraisal of the aetiology and prognostic factors of severe acute respiratory failure in HIV patients. Eur Respir J 17:87–93
Khouli H, Afrasiabi A, Shibli M et al (2005) Outcome of critically ill human immunodeficiency virus-infected patients in the era of highly active antiretroviral therapy. J Intensive Care Med 20:327–333
Acknowledgments
This work was supported by a grant from the “Fondo de Investigaciones Sanitarias, Subdirección General de Evaluación y Fomento de la Investigación, Ministerio de Ciencia e Innovación, Gobierno de España” (PI050167).
Nazaret Cobos-Trigueros is the recipient of a Río Hortega grant (CM12/00155) from the Instituto de Salud Carlos III.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
N. Cobos-Trigueros and M. Rinaudo contributed equally to this article.
Rights and permissions
About this article
Cite this article
Cobos-Trigueros, N., Rinaudo, M., Solé, M. et al. Acquisition of resistant microorganisms and infections in HIV-infected patients admitted to the ICU. Eur J Clin Microbiol Infect Dis 33, 611–620 (2014). https://doi.org/10.1007/s10096-013-1995-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-013-1995-5