Abstract
Objectives
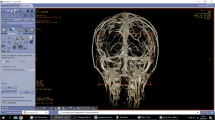
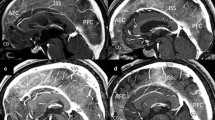
Surgery for parasagittal and falcine meningiomas requires meticulous preservation of the cortical veins that surround the tumour; thus, knowledge of the relevant venous anatomy would be extremely helpful during surgery.
Methods
This study utilises virtual reality technology to determine the number, size and disposition of the veins in relation to the tumour in 8 patients with parasagittal and falcine meningiomas. The same data were also collected from the scans of 8 normal subjects and compared with the data from the meningioma patients.
Results
Our results show that the average number of veins is comparable in the tumour and control groups, and that the number of veins on either side does not differ significantly for both groups. On measurement, the size of the veins is approximately the same on either side of the superior sagittal sinus for both the control and the tumour groups. It was also observed that regardless of size, most of the parasagittal and falcine meningiomas demonstrated no significant anatomical distortion effects on the adjacent venous structures, with the exception of one parasagittal meningioma with invasion of the superior sagittal sinus and concomitant engulfment of the draining veins.
Conclusion
Data from a larger population would have to be collected in order to determine the effect of the growth of these tumours on the surrounding venous anatomy. With virtual reality technology, the parasagittal veins are clearly discerned, and knowing their location and relationship to the tumour would contribute towards safe and effective surgery.


Similar content being viewed by others
References
Andrews BT, Dujovny M, Mirchandani HG, Ausman JI (1989) Microsurgical anatomy of the venous drainage into the superior sagittal sinus. Neurosurgery 24:514–520
Bozzao A, Finocchi V, Romano A, Ferrante M, Fasoli F, Trillo G et al (2005) Role of contrast-enhanced MR venography in the preoperative evaluation of parasagittal meningiomas. Eur Radiol 15(9):1790–1796. doi:10.1007/s00330-005-2788-8
Burtscher J, Kremser C, Seiwald M, Obwegeser A, Wagner M, Aichner F et al (1998) Three-dimensional computer assisted magnetic resonance imaging for neurosurgical planning in parasagittal and parafalcine central region tumors. Comput Aided Surg 3(1):27–32
Chua GG, Serra L, Kockro RA, Hern N, Nowinski WL, Chan C (1998) Volume-based tumor neurosurgery planning in the Virtual Workbench. Virtual Reality Annual International Symposium, 1998. Proceedings IEEE: 167–173
Gleason PL, Kikinis R, Altobelli D, Wells W, Alexander E, Black PM et al (1994) Video registration virtual reality for nonlinkage stereotactic surgery. Stereotact Funct Neurosurg 63:139–143. doi:10.1159/000100305
Hancq S, Baleriaux D, Brotchi J (2003) Surgical treatment of parasagittal meningiomas. Semin Neurosurg 14:203–210. doi:10.1055/s-2004-828923
Kockro RA, Serra L, Yeo TT, Chan C, Sitoh YY, Chua GG et al (2000) Planning and simulation of neurosurgery in a virtual reality environment. Neurosurgery 46(1):118–137. doi:10.1097/00006123-200001000-00024
Oka K, Rhoton AL, Barry M, Rodriguez R (1985) Microsurgical anatomy of the superficial veins of the cerebrum. Neurosurgery 17(5):711–748. doi:10.1097/00006123-198511000-00003
Oka K, Go Y, Kimura H, Tomonaga M (1994) Obstruction of the superior sagittal sinus caused by parasagittal meningiomas: the role of collateral venous pathways. J Neurosurg 81(4):520–524
Rhoton AL (1989) Microsurgical anatomy of the venous drainage into the superior sagittal sinus. Neurosurgery 24:514–520 commentary
Rosahl SK, Gharabaghi A, Shahidi UH, Samii M (2006) Virtual reality augmentation in skull base surgery. Skull Base 16(2):59–66. doi:10.1055/s-2006-931620
Sekhar LN, Chanda A, Morita A (2002) The preservation and reconstruction of cerebral veins and sinuses. J Clin Neurosci 9(4):391–399. doi:10.1054/jocn.2001.1008
Sindou M, Auque J, Jouanneau E (2005) Neurosurgery and the intracranial venous system. Acta Neurochir Suppl (Wien) 94:167–175. doi:10.1007/3-211-27911-3_27
Tigliev GS, Oliushin VE, Gurchin AF, Fadeeva TN, Chernov MF (1999) The collateral venous blood flow and the surgical procedure in parasagittal meningiomas. Vestn Khir Im I I Grek 158(1):9–12 abstract
Wei YH, Liang L, Yan FZ (2004) Resection of recurrent parasagittal meningiomas with complete obstructed superior sagittal sinus. Proceedings of the 3rd International Mt. Bandai Symposium for Neuroscience and the 4th Pan-Pacific Neurosurgery Congress 1259:53–57
Acknowledgements
The authors would like to thank Ms. Tay Lee Lian for her assistance in constructing 3-D virtual reality images from the MRI and MRV scans, and Ms. Lee Kah Keow for her help in the statistical analysis.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The virtual reality study of the superficial cortical veins, in particular the bridging veins, is an important preoperative study in the treatment of parasagittal and/or falcine meningiomas.
The problem with the surgery of meningiomas at these locations is real and surgeons are aware of it. With lack of experience, younger neurosurgeons might get into trouble while operating on parasagittal—mainly parietal—meningiomas conflicting with the important cortical veins. It is mandatory to preserve all these veins, even at the expense of incomplete resection of the meningioma. Of course, over the years, one gets more experienced in how to deal with these veins and how to approach the lesion(s). However, in some meningiomas it is impossible to remove the tumour completely without lesioning the bridging veins when the tumour is located at the inflow of the veins into the superior sagittal sinus. In such cases it is—in order to preserve the venous drainage—necessary to leave a coat of meningioma around the vein(s) in order to preserve the inflow from the vein(s) into the superior sagittal sinus and to preserve the drainage from the corresponding region of the brain.
Approaches have to be tailored according to the venogram in patients with parasagittal and/or falcine meningiomas. The microsurgical approach along the falx should be designed anteriorly and/or posteriorly to the tumour, or in some cases, where on the contralateral side there are better conditions (fewer or no veins), the approach may be from the opposite side, in order to devascularise it, and then to reduce it in size or to remove it completely. Only when the volume of the meningioma is gross-totally resected, and pressure against the bridging veins reduced, is the dissection of the rest of the tumour from the veins much easier and less dangerous.
Coupling the images of the veins with the MRI does give the surgeon the opportunity to study the relationship between the tumourous and other structures before surgical intervention, and this no doubt can help in conducting real surgery with more information on the critical structures. However, the most important fact is that under no circumstances should the vein(s) be interrupted. The reasons for this are: the reconstruction or surgical by-passing of the veins is still very questionable regarding the final outcome, and on the other hand, the abrupt interruption of the drainage from a territory is very dangerous in all cases where collaterals have not existed. It is for this reason that, when the tumour cannot be resected completely and when and if the veins remain compromised, the collaterals will develop over a longer period of time, and only when these collaterals are functioning is the surgeon's task less difficult and risky regarding the gross-total or complete removal of the tumour. In our practice, it is possible to recollect such cases where we were not radical with resection of the lesion for the above-mentioned reason(s), and surgery was repeated after a period of years; in some cases even twice. Nowadays, there is also the possibility of treating such a meningioma rest with the Gamma knife.
Vinko V. Dolenc
Ljubljana, Slovenia
Rights and permissions
About this article
Cite this article
Khu, K.J., Ng, I. & Ng, W.H. The relationship between parasagittal and falcine meningiomas and the superficial cortical veins: a virtual reality study. Acta Neurochir 151, 1459–1464 (2009). https://doi.org/10.1007/s00701-009-0379-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0379-1