Abstract
Background
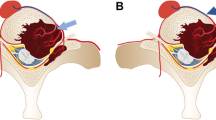
Radical surgery of renal cell carcinoma spinal metastases carries a high risk due to potentially life-threatening extreme blood loss. Radical preoperative embolization of renal cell carcinoma metastases alone is not necessarily a guarantee of extreme blood loss not occurring during operation.
Methods
A retrospective analysis of 15 patients following radical surgery for a spinal metastases of a renal cell carcinoma was performed. Eight patients were embolized preoperatively and 7 were not. We analysed features influencing peroperative blood loss: size and extent of tumour, complexity of surgical approaches and radicality of embolization.
Results
The embolized and non embolized groups were not comparable before treatment. They differed markedly in size of tumour as well as the complexity of approach. In the embolized group the size of the tumour was, on average, twice as large as that in non embolized patients and more complex approaches were used twice as frequently. Despite findings suggesting that embolization was effective, blood loss was greater in the embolized group of 8 patients (4750 ml), compared to the non-embolized group of 7 patients (1786 ml).
Conclusion
Metastasis size, extent of tumour, technical complexity of surgery and the completeness of preoperative embolization had an important effect on the amount of peroperative blood loss. The evaluation of the benefits of preoperative embolization only on the basis of blood loss is not an adequate method.

Similar content being viewed by others
References
Berkefeld J, Scale D, Kirchner J, Heinrich T, Kollath J (1999) Hypervascular spinal tumors: influence of the embolization technique on preoperative hemorrhage. AJNR 20:757–763
Bowers TA, Murray JA, Charnsangavej C, Soo CS, Chuang VP, Wallace S (1982) Bone metastase from renal carcinoma: the pre-operative use of transcatheter arterial occlusion. J Bone Point Surg (Am) 64:749–754
Breslau J, Eskridge JM (1995) Preoperative embolization of spinal tumors. J Vasc Interv Radiol 6(6):871–875
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ (1969) The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Part 1. Paraplegia 7:179–192
Gellad FE, Sadato N, Numaguchi Y, Levine AM (1990) Vascular metastatic lesions of the spine: preoperative embolization. Radiology 176:683–686
Guzman R, Dubach-Schwizer S, Heini P, Lovblad KO, Kalbermatten D, Schroth G, Remonda L (2005) Preoperative transarterial embolization of vertebral metastases. Eur Spine J 14:263–268
Hess T, Kramann B, Schmidt E, Rupp S (1997) Use of preoperative vascular embolization in spinal metastases resection. Arch Orthop Trauma Surg 116:279–282
Chatziioannou AN, Johnson ME, Pneumaticoc SG, Lawrence DD, Carrasco CH (2000) Preoperative embolization of bone metastase from renal cell carcinoma. Europ Radiol 10:593–596
Manke Ch, Bretschneide T, Lenhart M, Strotzer M, Neumann C, Gmeinwieser J, Feurbach S (2001) Spinal metastases from renal cell carcinoma: effect of preoperative particle embolization on intraoperative blood loss. AJNR (Am) J Neuroradiol 22:997–1003
Olerud C, Jonsson H, Lofberg AM, Lorelius LE, Sjostrom L (1993) Embolization of spinal metastases reduces peroperative blood loss. 21 patients operated on for renal cell carcinoma. Acta Orthop Scand 64(1):9–12
Prabhu VC, Bilsky MH, Jambhekar K, Panageas KS, Boland PJ, Lis E, Heier L, Nelson K (2002) Results of preoperative embolization for metastatic spinal neoplasms. J Neurosurg (Spine 2) 98:156–164
Řehák S, Málek V, Náhlovský J, Odrážka K, Ryška P, Kaltofen K, Česák T, Melichar B, Kanta M (2004) Chirurgická léčba metastatického onemocnění páteře. Acta Spondylologica 3:15–23
Smith TP, Gray L, Weinstein JN, Richardson WJ, Payne CS (1995) Preoperative transarterial embolization of spinal column neoplasms. J Vasc Interv Radiol 6(6):863–869
Sun S, Lang EV (1998) Bone metastase from renal cell carcinoma: preoperative embolization. JVIR 9:263–269
Sundaresan N, Scher H, DiGiacinto GV, Yagoda A, Whitmore W, Choi IS (1986) Surgical treatment of spinal cord compression in kidney cancer. J Clin Oncol 4:1851–1856
Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T (2001) Surgical strategy for spinal metastases. Spine 26(3):298–306
Tokuhashi Y, Matsuzaki H, Toriyama S, Kawano H, Ohsaka S (1990) Scoring system for the preoperative evaluation of metastatic spine tumor prognosis. Spine 15(11):1110–1113
Ungermann L, Krajina A, Lojík M, Urban K, Málek V, Chovance V, Raupach J, Mašková J (2005) Embolizace nádorů kostí – retrospektivní analýza 8 letých zkušeností. Čes Radiol 59(1):27–31
Acknowledgment
This study was supported by a grant of the Ministry of Health, Czech republic (grant No: IGA MZCR NR 7953–3/2004).
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Rehak et al. retrospectively analyzed 15 cases of spinal renal cell carcinoma metastases, operated on during a 9 year period. One major problem of this kind of secondary tumour manifestation close to the spinal cord is its hypervascularization, which risks extensive, sometimes life-threatening, bleeding and/or post-operative neurological deterioration. Therefore, pre-operative embolization is favoured by many surgeons prior to attempting complete tumour removal or even before decompressive surgery. The available scientific literature on pre-surgical embolization does suggest lower operative complication rates and better patient outcomes after pre-surgical embolization. Unfortunately, past reports are based on small case series and have not led to any widely accepted recommendations about when or when not to embolize RCC etastases. The strength of this paper from Rehak et al. is that it begins to develop reflections on the process of decision making concerning pre-operative tumour embolization, its effectiveness and limits, and the risk of blood loss despite embolization of metastases. Even with embolization, surgery with the aim of complete removal of a hypervascuralized spinal tumour remains a risky procedure, as the 1 mortality from 8 embolized patients in the authors’ series showed. The authors did not find any statistically significant predictors of whether or not to embolize, except the estimated risk of intraoperative blood loss according to the surgeon’s personal opinion. Thus, 2 of 7 cases without embolization had to be stopped before complete tumour removal because of extreme blood loss. So what we can learn from this study is that surgeons should seriously consider pre-operative embolization, at least when there are hypervascularized spinal metastasis exceeding the bony structures of the affected vertebra with infiltrating paravertebral tumour extension, and when the surgical aim is complete resection via a combined dorso-ventral approach. But it still remains unclear whether there is any benefit from embolization for smaller tumours (which can be removed via a posterior approach alone). Rehak et al. have made a valuable contribution by reporting their cases and initiating renewing discussion on the surgical treatment of RCC metastases. Now studies with larger sample sizes or metaanlyses of past studies are needed to determine more clearly the benefits and risks of performing pre-operative embolization or not.
Olaf Suess
Department of Neurosurgery, Charité,
Berlin, Germany
Rights and permissions
About this article
Cite this article
Řehák, S., Krajina, A., Ungermann, L. et al. The role of embolization in radical surgery of renal cell carcinoma spinal metastases. Acta Neurochir (Wien) 150, 1177–1181 (2008). https://doi.org/10.1007/s00701-008-0031-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-008-0031-5