Abstract
Purpose
The aim of this network meta-analysis (NMA) was to compare the complication rates of discectomy/microdiscectomy, percutaneous laser disc decompression (PLDD), percutaneous endoscopic lumbar discectomy (PELD), microendoscopic discectomy (MED), and tubular discectomy for symptomatic lumbar disc herniation (LDH).
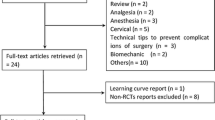
Methods
We searched three online databases for randomized controlled trials (RCTs). Overall complication rates, complication rates per general and modified Clavien–Dindo classification schemes, and reoperation rates were considered as primary outcomes. Odds ratio with 95% confidence intervals for direct comparisons and 95% credible intervals for NMA results were reported. Surface under cumulative ranking curve (SUCRA) was used to estimate ranks for each discectomy technique based on the complication rates.
Results
In total, 18 RCTs with 2273 patients were included in this study. Our results showed that there was no significant difference in any of the pairwise comparisons. PELD (SUCRA: 0.856) ranked the lowest for overall complication rates. Discectomy/microdiscectomy (SUCRA: 0.599) and PELD (SUCRA: 0.939) ranked the lowest for intraoperative and post-operative complication rates, respectively. Concerning modified Clavien–Dindo classification scheme, PELD (SUCRA: 0.803), MED (SUCRA: 0.730), and PLDD (SUCRA: 0.605) ranked the lowest for the occurrence of type I, II, and III complications, respectively. Tubular discectomy (SUCRA: 0.699) ranked the lowest for reoperation rates.
Conclusions
The results of this NMA suggest that discectomy/microdiscectomy and PELD are the safest procedures for LDH with minimal intraoperative and post-operative complications, respectively. PELD, MED, and PLDD are the safest procedures for LDH in terms of minimal rates for complications necessitating conservative, pharmacological, and surgical treatment, respectively.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.





Similar content being viewed by others
References
Benzakour T, Igoumenou V, Mavrogenis AF, Benzakour A (2018) Current concepts for lumbar disc herniation. Int Orthop 43:841–851. https://doi.org/10.1007/s00264-018-4247-6
Postacchini F (1999) Management of herniation of the lumbar disc. J Bone Jt Surg Br 81:567–576
Taylor VM, Deyo RA, Cherkin DC, Kreuter W (1994) Low back pain hospitalization. Recent United States trends and regional variations. Spine 19:1207–1212 (discussion 1213)
Maroon JC (2002) Current concepts in minimally invasive discectomy. Neurosurgery 51:S137–S145. https://doi.org/10.1227/01.NEU.0000031066.08137.64
Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P 2nd, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WL Jr, Toton JF, North American Spine S (2014) An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 14:180–191. https://doi.org/10.1016/j.spinee.2013.08.003
Kim CH, Chung CK, Jahng TA, Yang HJ, Son YJ (2012) Surgical outcome of percutaneous endoscopic interlaminar lumbar diskectomy for recurrent disk herniation after open diskectomy. J Spinal Disord Tech 25:E125–E133. https://doi.org/10.1097/BSD.0b013e31825bd111
Ruetten S, Komp M, Merk H, Godolias G (2009) Recurrent lumbar disc herniation after conventional discectomy: a prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech 22:122–129. https://doi.org/10.1097/BSD.0b013e318175ddb4
DePalma MJ, Ketchum JM, Saullo TR, Laplante BL (2012) Is the history of a surgical discectomy related to the source of chronic low back pain? Pain Physician 15:E53–E58
Yasargil MG (1977) Microsurgical operations for herniated lumbar disc. Adv Neurosurg 4:81–82
Caspar W (1977) A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. Adv Neurosurg 4:74–80
Rasouli MR, Rahimi-Movaghar V, Shokraneh F, Moradi-Lakeh M, Chou R (2014) Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev 9:CD010328. https://doi.org/10.1002/14651858.CD010328.pub2
Deen HG, Fenton DS, Lamer TJ (2003) Minimally invasive procedures for disorders of the lumbar spine. Mayo Clin Proc 78:1249–1256
Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, Nakashima S, Ito Z, Ishiguro N (2006) Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech 19:344–347
Foley KT, Smith MM, Rampersaud YR (1999) Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 7:e5
Clark AJ, Safaee MM, Khan NR, Brown MT, Foley KT (2017) Tubular microdiscectomy: techniques, complication avoidance, and review of the literature. Neurosurg Focus 43:E7. https://doi.org/10.3171/2017.5.FOCUS17202
Foley MKT (1997) Microendoscopic discectomy. Tech Neurosurg 3:301–307
Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K (2001) Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine 26:652–657
Shriver MF, Xie JJ, Tye EY, Rosenbaum BP, Kshettry VR, Benzel EC, Mroz TE (2015) Lumbar microdiscectomy complication rates: a systematic review and meta-analysis. Neurosurg Focus 39:E6. https://doi.org/10.3171/2015.7.FOCUS15281
Kraemer R, Wild A, Haak H, Herdmann J, Krauspe R, Kraemer J (2003) Classification and management of early complications in open lumbar microdiscectomy. Eur Spine J 12:239–246. https://doi.org/10.1007/s00586-002-0466-y
Kim M, Lee S, Kim HS, Park S, Shim SY, Lim DJ (2018) A comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for lumbar disc herniation in the Korean: a meta-analysis. Biomed Res Int 2018:9073460. https://doi.org/10.1155/2018/9073460
Shi R, Wang F, Hong X, Wang YT, Bao JP, Liu L, Wang XH, Xie ZY, Wu XT (2018) Comparison of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy for the treatment of lumbar disc herniation: a meta-analysis. Int Orthop 43:923–937. https://doi.org/10.1007/s00264-018-4253-8
Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A (2016) Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: A meta-analysis. Int J Surg 31:86–92. https://doi.org/10.1016/j.ijsu.2016.05.061
Cong L, Zhu Y, Tu G (2016) A meta-analysis of endoscopic discectomy versus open discectomy for symptomatic lumbar disk herniation. Eur Spine J 25:134–143. https://doi.org/10.1007/s00586-015-3776-6
Wang XS, Sun RF, Ji Q, Zhao B, Niu XM, Wang R, Peng L, Tian XD (2014) A meta-analysis of interlaminar minimally invasive discectomy compared to conventional microdiscectomy for lumbar disk herniation. Clin Neurol Neurosurg 127:149–157. https://doi.org/10.1016/j.clineuro.2014.10.001
He J, Xiao S, Wu Z, Yuan Z (2016) Microendoscopic discectomy versus open discectomy for lumbar disc herniation: a meta-analysis. Eur Spine J 25:1373–1381. https://doi.org/10.1007/s00586-016-4523-3
Akinduro OO, Kerezoudis P, Alvi MA, Yoon JW, Eluchie J, Murad MH, Wang Z, Chen SG, Bydon M (2017) Open versus minimally invasive surgery for extraforaminal lumbar disk herniation: a systematic review and meta-analysis. World Neurosurg 108:924–938. https://doi.org/10.1016/j.wneu.2017.08.025
Qin R, Liu B, Hao J, Zhou P, Yao Y, Zhang F, Chen X (2018) Percutaneous endoscopic lumbar discectomy versus posterior open lumbar microdiscectomy for the treatment of symptomatic lumbar disc herniation: a systemic review and meta-analysis. World Neurosurg 120:352–362. https://doi.org/10.1016/j.wneu.2018.08.236
Chang X, Chen B, Li HY, Han XB, Zhou Y, Li CQ (2014) The safety and efficacy of minimally invasive discectomy: a meta-analysis of prospective randomised controlled trials. Int Orthop 38:1225–1234. https://doi.org/10.1007/s00264-014-2331-0
Li X, Chang H, Meng X (2018) Tubular microscopes discectomy versus conventional microdiscectomy for treating lumbar disk herniation: systematic review and meta-analysis. Medicine 97:e9807. https://doi.org/10.1097/MD.0000000000009807
Mu X, Wei J, Li P (2015) What were the advantages of microendoscopic discectomy for lumbar disc herniation comparing with open discectomy: a meta-analysis? Int J Clin Exp Med 8:17498–17506
Lebude B, Yadla S, Albert T, Anderson DG, Harrop JS, Hilibrand A, Maltenfort M, Sharan A, Vaccaro AR, Ratliff JK (2010) Defining “complications” in spine surgery: neurosurgery and orthopedic spine surgeons' survey. J Spinal Disord Tech 23:493–500. https://doi.org/10.1097/BSD.0b013e3181c11f89
Reis RC, de Oliveira MF, Rotta JM, Botelho RV (2015) Risk of complications in spine surgery: a prospective study. Open Orthop J 9:20–25. https://doi.org/10.2174/1874325001509010020
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Ibanez FAL, Hem S, Ajler P, Vecchi E, Ciraolo C, Baccanelli M, Tramontano R, Knezevich F, Carrizo A (2011) A new classification of complications in neurosurgery. World Neurosurg 75:709–715. https://doi.org/10.1016/j.wneu.2010.11.010 (discussion 604–711)
Leucht S, Chaimani A, Cipriani AS, Davis JM, Furukawa TA, Salanti G (2016) Network meta-analyses should be the highest level of evidence in treatment guidelines. Eur Arch Psychiatry Clin Neurosci 266:477–480. https://doi.org/10.1007/s00406-016-0715-4
Rouse B, Chaimani A, Li T (2017) Network meta-analysis: an introduction for clinicians. Intern Emerg Med 12:103–111. https://doi.org/10.1007/s11739-016-1583-7
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, van Tulder MW (2015) 2015 Updated method guideline for systematic reviews in the Cochrane back and neck group. Spine 40:1660–1673. https://doi.org/10.1097/brs.0000000000001061
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions, version 510. The Cochrane Collaboration, London
Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS ONE 8:e76654. https://doi.org/10.1371/journal.pone.0076654
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406. https://doi.org/10.1016/j.jclinepi.2010.07.015
Puhan MA, Schunemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, Kessels AG, Guyatt GH, Glow GW (2014) A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 349:g5630. https://doi.org/10.1136/bmj.g5630
Ding ZM, Tao YQ (2017) Clinical outcomes of percutaneous transforaminal endoscopic discectomy versus fenestration discectomy in patients with lumbar disc herniation. J Int Transl Med 5:29–33. https://doi.org/10.11910/2227-6394.2017.05.01.06
Franke J, Greiner-Perth R, Boehm H, Mahlfeld K, Grasshoff H, Allam Y, Awiszus F (2009) Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J 18:992–1000. https://doi.org/10.1007/s00586-009-0964-2
Righesso O, Falavigna A, Avanzi O (2007) Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 61:545–549. https://doi.org/10.1227/01.NEU.0000280008.72190.15
Abrishamkar S, Kouchakzadeh M, Mirhosseini A, Tabesh H, Rezvani M, Moayednia A, Ganjeifar B, Mahabadi A, Yousefi E, Kooshki AM (2015) Comparison of open surgical discectomy versus plasma-laser nucleoplasty in patients with single lumbar disc herniation. J Res Med Sci 20:1133–1137. https://doi.org/10.4103/1735-1995.172979
Pan L, Zhang P, Yin Q (2014) Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: a randomised controlled trial. Int J Surg 12:534–537. https://doi.org/10.1016/j.ijsu.2014.02.015
Pan Z, Ha Y, Yi S, Cao K (2016) Efficacy of transforaminal endoscopic spine system (TESSYS) technique in treating lumbar disc herniation. Med Sci Monitor 22:530–539. https://doi.org/10.12659/msm.894870
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine 33:931–939
Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, Minoia L (2010) Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J 19:443–450. https://doi.org/10.1007/s00586-010-1290-4
Huang TJ, Hsu RW, Li YY, Cheng CC (2005) Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res 23:406–411
Garg B, Nagraja UB, Jayaswal A (2011) Microendoscopic versus open discectomy for lumbar disc herniation: A prospective randomised study. J Orthop Surg 19:30–34
Hussein M (2016) Minimal incision, multifidus-sparing microendoscopic diskectomy versus conventional microdiskectomy for highly migrated intracanal lumbar disk herniations. J Am Acad Orthop Surg 24:805–813. https://doi.org/10.5435/JAAOS-D-15-00588
Mayer HM, Brock M (1993) Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg 78:216–225
Brouwer PA, Brand R, van den Akker-van Marle ME, Jacobs WC, Schenk B, van den Berg-Huijsmans AA, Koes BW, Arts MA, van Buchem MA, Peul WC (2017) Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: Two-year results of a randomised controlled trial. Interv Neuroradiol 23:313–324. https://doi.org/10.1177/1591019917699981
Hermantin FU, Peters T, Quartararo L, Kambin P (1999) A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic m. J Bone Joint Surg Am 81:958–965
Hussein M, Abdeldayem A, Mattar MM (2014) Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J 23:1992–1999. https://doi.org/10.1007/s00586-014-3296-9
Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V (2008) Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery 62:174–181. https://doi.org/10.1227/01.NEU.0000296996.00030.3F
Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Tan WF, Peul WC (2011) Tubular diskectomy vs conventional microdiskectomy for the treatment of lumbar disk herniation: 2-year results of a double-blind randomized controlled trial. Neurosurgery 69:135–144. https://doi.org/10.1227/NEU.0b013e318214a98c (discussion 144)
Chen Z, Zhang L, Dong J, Xie P, Liu B, Wang Q, Chen R, Feng F, Yang B, Shu T, Li S, Yang Y, He L, Pang M, Rong L (2018) Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J Neurosurg Spine 28:300–310. https://doi.org/10.3171/2017.7.SPINE161434
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine 33:931–939. https://doi.org/10.1097/BRS.0b013e31816c8af7
Brouwer PA, Brand R, van den Akker-van Marle ME, Jacobs WCH, Schenk B, van den Berg-Huijsmans AA, Koes BW, Arts MA, van Buchem MA, Peul WC (2017) Percutaneous laser disc decompression versus conventional microdiscectomy for patients with sciatica: Two-year results of a randomised controlled trial. Interventional Neuroradiology 23:313–324. https://doi.org/10.1177/1591019917699981
Hermantin FU, Peters T, Quartararo L, Kambin P (1999) A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am 81:958–965
Feng F, Xu Q, Yan F, Xie Y, Deng Z, Hu C, Zhu X, Cai L (2017) Comparison of 7 surgical interventions for lumbar disc herniation: a network meta-analysis. Pain Physician 20:E863–E871
Acknowledgements
The authors would like to thank Joyce Cornelius (outreach librarian, UNSW) for her help with developing the database search strategy.
Funding
This work was supported by a Research Training Program scholarship and a University Postgraduate Award from the Australian Government and UNSW to XLC. A Clinical Travelling Fellowship from the International Society for the Study of the Lumbar Spine (ISSLS) in 2018 further supported this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, X., Chamoli, U., Lapkin, S. et al. Complication rates of different discectomy techniques for the treatment of lumbar disc herniation: a network meta-analysis. Eur Spine J 28, 2588–2601 (2019). https://doi.org/10.1007/s00586-019-06142-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06142-7