Abstract
In Europe, the introduction of monovalent meningococcal serogroup C (MenC) conjugate vaccines has resulted in a significant decline in MenC invasive disease. However, given the potential for strain evolution and increasing travel to areas of high endemicity, protection against additional serogroups is needed. In this study, the immunogenicity, measured by a serum bactericidal activity assay using rabbit complement (rSBA), and the safety of a quadrivalent meningococcal serogroups A, C, W-135 and Y tetanus toxoid conjugate vaccine (MenACWY-TT) were compared to that of a licensed monovalent MenC conjugate vaccine (MenC-CRM197) in children 2–10 years of age. Children were randomised (3:1) to receive a single dose of either MenACWY-TT or MenC-CRM197. Non-inferiority of the immunogenicity of MenACWY-TT versus MenC-CRM197 in terms of rSBA-MenC vaccine response was demonstrated. Exploratory analyses suggested that rSBA-MenC geometric mean titres adjusted for pre-vaccination titres were lower in children vaccinated with MenACWY-TT compared to MenC-CRM197. Nevertheless, at 1 month post-vaccination, ≥99.3 % of the children who received MenACWY-TT had rSBA titres ≥1:128 for each of the four vaccine serogroups, which is the more conservative correlate of protection. The reactogenicity and safety profile of MenACWY-TT was clinically acceptable and no serious adverse events considered related to vaccination were reported throughout the study. Conclusion: When administered to European school-age children, MenACWY-TT has a clinically acceptable safety profile and, when compared with MenC-CRM197, the potential to broaden protection against meningococcal disease caused by serogroups A, W-135 and Y while maintaining protection against MenC. This study has been registered at www.clinicaltrials.gov NCT00674583.
Similar content being viewed by others
Introduction
Neisseria meningitidis is an important cause of invasive bacterial infections, such as meningitis and sepsis, which are major public health concerns throughout the world [18, 24, 41]. Although the incidence of meningococcal disease is highest in infants, children are also at risk, particularly if they travel to areas of high endemicity. The mean annual incidence of invasive meningococcal disease was 0.71 per 100,000 inhabitants in Germany between 2002 and 2010 and varied between 0.9 and 1.5 cases per 100,000 inhabitants in France during the past 10 years [26, 39]. Globally, six serogroups (MenA, MenB, MenC, MenW-135, MenY and MenX) are responsible for most cases of meningococcal disease [23, 24, 41, 49, 50]. In Europe, MenB and MenC are the most prevalent serogroups, although diseases caused by MenA, MenW-135 and MenY have also been reported in some European countries [2, 6, 22, 51, 52, 54, 55]. In Germany, the incidence of invasive meningococcal disease caused by MenB and MenC decreased between 2002 and 2010 from 0.63 to 0.32 cases and from 0.26 to 0.10 cases per 100,000 inhabitants younger than 25 years of age, respectively [26]. In France, invasive meningococcal disease cases were also mainly due to MenB and MenC during the past decade (65 and 27 %, respectively) [39].
Prevention of meningococcal disease by vaccination is the best control strategy, and the development of broadly effective vaccines is a public health priority [23, 49]. To overcome the limitations of meningococcal plain polysaccharide vaccines, which are poorly immunogenic in young children, do not induce immune memory, do not reduce mucosal carriage and do not confer herd immunity, meningococcal capsular polysaccharides were covalently bound to carrier proteins in conjugate vaccines [19, 23, 25, 34, 38]. Monovalent MenC conjugate vaccines are licensed for use in children from 2 months of age in Europe [10, 13, 33, 35, 43, 53], children older than 1 year of age in Australia [45], and children between 2 months and 5 years of age, adolescents, and adults in Canada [5, 31]. Routine MenC vaccination was introduced in the national childhood vaccination schedule for children 12–24 months of age in Germany in 2006 and in France in 2010 [15, 26]. Of note, the introduction of monovalent MenC conjugate vaccines into routine vaccination schedules in Europe since 2006 has led to a ten-fold drop in the incidence of MenC disease [17]. In the current study, children 2–10 years of age were vaccinated in 2008, and an exclusion criterion required that no previous meningococcal conjugate vaccine had been administered; therefore, this study did not interfere with either national vaccination programme.
Given the potential strain evolution and increasing global travel to areas of high endemicity, vaccines offering broader protection are needed. A quadrivalent MenA, MenC, MenW-135 and MenY conjugate vaccine using diphtheria toxoid as carrier protein (Menactra™, Sanofi Pasteur) has been licensed in the USA for use in individuals between 11 and 55 years of age since 2005, in children between 2 and 10 years of age in 2007, and in toddlers between 9 and 23 months of age in 2011 [30, 40, 56]. Another quadrivalent meningococcal conjugate vaccine using a mutant diphtheria toxoid as carrier protein (MenACWY-CRM197; Menveo™, Novartis) has been authorised since 2010–2011 for active immunisation of individuals from 2 years of age in the European Union and Australia and between 2 and 55 years of age in Canada and the USA [7, 27, 57]. Beside these quadrivalent vaccines, a monovalent MenA conjugate vaccine (MenA-TT, MenAfriVac™, Serum Institute of India) has been specifically developed for Africa. MenA accounts for about 80–85 % of the cases in the ‘Meningitis Belt’, a region covering 25 countries in sub-Saharan Africa [48]. Finally, a combination Haemophilus influenzae type b–Neisseria meningitidis serogroups C and Y conjugate vaccine (Hib-MenCY-TT, MenHibrix™, GlaxoSmithKline Vaccines) was licensed for use in US infants [11].
In addition, a quadrivalent MenA, MenC, MenW-135 and MenY tetanus toxoid (TT) conjugate vaccine (MenACWY-TT; Nimenrix™, GlaxoSmithKline Vaccines) has been developed and recently approved by the European Medicines Agency for the active immunisation of individuals older than 12 months of age [16]. Non-inferiority of MenACWY-TT compared to a licensed quadrivalent plain polysaccharide vaccine was shown in a previous study conducted in children 2–10 years of age [37]. Since monovalent MenC conjugate vaccines are also licensed in school-age children, this study was designed to assess immunological non-inferiority of MenACWY-TT versus a commonly used monovalent MenC conjugate vaccine (MenC-CRM197; Menjugate™, Novartis). In addition, the immunogenicity to MenA, MenW-135 and MenY, and the safety profile of MenACWY-TT were assessed.
Materials and methods
Study design
This study was a phase III, open, randomised, controlled trial conducted in 20 centres in Germany and 11 centres in France between May 2008 and January 2009. The study was conducted in accordance with the guidelines for Good Clinical Practice, all applicable regulatory requirements and the Declaration of Helsinki. The protocol and associated documents were reviewed and approved by local ethics committees. Written informed consent was obtained from the parents/guardians of children prior to the performance of any study specific procedures. In Germany, informed assents were obtained from the children who were able to understand and sign the informed assent form according to the investigators’ discretion. In France, parents/legally authorized representatives signed the informed consent form, with provision of study information to the subject. Informed consent/assent procedures were aligned with country standards and were approved by the relevant ethics committee.
Healthy children were enrolled in two age strata: 2–5 years and 6–10 years of age. Within each age stratum, children were randomised into two parallel groups to receive a single dose of either MenACWY-TT (ACWY-TT group) or MenC-CRM197 (MenC-CRM group). Blood samples were collected from all children at pre-vaccination (month 0) and at 1 month post-vaccination (month 1). This active vaccination phase was followed by an extended safety follow-up phase up to 6 months post-vaccination (month 6).
Treatment allocation at the investigator site was performed using a central, web-based randomisation system. The randomisation algorithm (block size of four) included a minimisation procedure to ensure balanced allocation between groups at individual centres and in the two age strata. The study was open in design because the vials containing the study vaccines differed in appearance. This study has been registered at www.clinicaltrials.gov NCT00674583. A summary of the protocol is available at http://www.gsk-clinicalstudyregister.com (GSK study ID 111414).
Study objectives
The primary objective was to demonstrate the non-inferiority of MenACWY-TT versus MenC-CRM197 in terms of vaccine response to MenC measured with a serum bactericidal activity assay using rabbit complement (rSBA) in children 2–10 years of age. Non-inferiority was shown if the lower limit (LL) of the two-sided standardised asymptotic 95 % confidence interval (CI) for the group difference (ACWY-TT group minus MenC-CRM group) in the percentages of children with rSBA-MenC vaccine response at month 1 was greater than or equal to −10 %.
The secondary objectives included the evaluation of the immunogenicity of MenACWY-TT to MenA, MenW-135 and MenY at month 1; the comparison of the immunogenicity of MenACWY-TT and MenC-CRM in terms of percentages of children with rSBA-MenC titres above pre-defined thresholds and rSBA-MenC geometric mean titres (GMTs); and the evaluation of the reactogenicity and safety profiles of both vaccines throughout the study.
Study participants
Participants were healthy boys or girls between 2 and 10 years of age at the time of vaccination, who had completed routine childhood vaccination to the best of their parents/guardians knowledge.
Children who were immunosuppressed from any cause, had a history of meningococcal disease, had previously received a meningococcal conjugate vaccine at any time, had had previous vaccination with a meningococcal polysaccharide vaccine (for participants younger than 6 years of age) or within the last 5 years (for participants 6 years of age and older), or had previously received immunoglobulins or blood products within 3 months preceding the study were excluded from the trial.
Vaccines
One 0.5-mL dose of MenACWY-TT contained 5 μg of each meningococcal serogroup polysaccharide (MenA, MenC, MenW-135 and MenY) conjugated to TT (approximately 44 μg in total). The lyophilised vaccine was reconstituted with saline. The licensed MenC-CRM197 vaccine (Menjugate™, Novartis) comprised 10 μg of MenC polysaccharide conjugated to CRM197 (12.5 to 25 μg) adsorbed onto aluminium hydroxide (0.3–0.4 mg). The vaccines were administered intramuscularly into the non-dominant deltoid or thigh as age appropriate.
Immunogenicity assessment
Immunogenicity to all four meningococcal polysaccharides was assessed with an rSBA assay [1, 36], which was performed as previously described [4]. The cut-off of the assay was a dilution titre of 1:8, which is considered a surrogate marker of protection for rSBA-MenC [9] and has been extended to the other serogroups [12]. In addition, antibody titres were also measured using a threshold of 1:128, which is the more conservative correlate of protection [8]. An rSBA vaccine response was defined as an rSBA titre of at least 1:32 in initially seronegative children (i.e. rSBA titre <1:8) and as a four-fold increase in titre from pre- to post-vaccination in initially seropositive children (i.e. rSBA titre ≥1:8). All immunological assays were performed at GlaxoSmithKline’ laboratories (Rixensart, Belgium).
Safety and reactogenicity assessment
The occurrence of solicited local symptoms at the injection site (pain, redness and swelling in both age strata) and of solicited general symptoms (drowsiness, fever [oral temperature ≥37.5 °C], irritability and loss of appetite in the 2–5 years age stratum, and fatigue, fever, gastro-intestinal symptoms and headache in the 6–10 years age stratum) was recorded up to 4 days after vaccination by the parents or guardians on a written diary card. Unsolicited adverse events (AEs) were recorded on the diary cards for a period of 31 days after vaccination. These events were then transcribed by the investigator into an electronic case report form.
The intensity of each symptom was graded on a three-level scale. In the 2–5 years age stratum, redness and swelling were of grade 3 intensity if their diameter was >30 mm, pain if the child cried when the limb was moved or if the limb was spontaneously painful and loss of appetite if the child did not eat at all. In the 6–10 years age stratum, redness and swelling were of grade 3 intensity if their diameter was >50 mm. In both age strata, grade 3 fever was defined as oral temperature >39.5 °C. All other symptoms of grade 3 intensity were defined as symptoms preventing normal activity.
Serious adverse events (SAEs), AEs of specific interest (new onset of chronic illnesses, rashes and AEs resulting in emergency room visits) were reported during 6 months post-vaccination. All solicited local (injection site) reactions were considered causally related to vaccination. The relationship to vaccination of all other symptoms was assessed by the investigator.
Statistical analyses
With a target sample size of 400 children (300 children in the ACWY-TT group and 100 children in the MenC-CRM group), the power to meet the primary objective of this study was at least 85.6 %.
The total vaccinated cohort, on which the primary safety analyses were performed, included all vaccinated children. The primary analysis of immunogenicity was performed on the according to protocol (ATP) cohort for immunogenicity, which included all the children meeting the eligibility criteria, complying with the protocol-defined procedures, with no elimination criteria during the study, and for whom data concerning immunogenicity endpoints were available for at least one study vaccine antigen. While immunogenicity and unsolicited symptoms were evaluated on the entire study population, the safety evaluation for solicited symptoms was performed separately on the 2–5 years and 6–10 years age strata because the nature of the solicited general symptoms and the severity grading of the solicited local symptoms differed.
Percentages of children with antibody titres above the proposed cut-offs, vaccine response rates, and GMTs for the four serogroups were calculated in each treatment group with 95 % CIs. The GMTs were calculated by taking the anti-log of the mean of the log10 titre transformations. Antibody titres below the cut-off of the assay were given an arbitrary value of half the cut-off for the purpose of GMT calculation. The distribution of titres was also evaluated using reverse cumulative curves for each meningococcal serogroup.
Exploratory analyses compared immune responses to the four serogroups between the ACWY-TT and the MenC-CRM groups. The two groups were considered statistically significantly different if the standardised asymptotic 95 % CI for the difference in rates (percentages of children with titres above proposed cut-offs or with vaccine response) between the two vaccine groups did not contain the value ‘0’ or if the 95 % CI for the GMT ratio between the two groups did not contain the value ‘1’. The GMT ratios were computed by an analysis of covariance model on the log10 transformation of the titres using the pre-vaccination log10 transformation of the titres, the age strata and the vaccine group as covariates. No adjustment for multiplicity of secondary endpoints was made, and significant results from the exploratory analyses should be interpreted with caution.
The percentages of children reporting each solicited local and general (any and grade 3) symptom were tabulated per age strata with exact 95 % CIs. The percentages of children reporting unsolicited AEs (any and grade 3) were tabulated overall with exact 95 % CIs. SAEs, AEs of specific interest and withdrawals due to AEs were described in detail.
The statistical analyses were performed using the SAS® software version 9.1 (SAS Institute Inc., Cary, NC, USA) and StatXact 7.0.
Results
Study participants
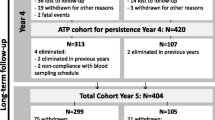
A total of 414 children were enrolled and vaccinated in this study (311 in the ACWY-TT group and 103 in the MenC-CRM group) (Fig. 1). All the children completed the active vaccination phase of the study, and 413 of them completed the extended safety follow-up phase. The ATP cohort for immunogenicity included 296 children in the ACWY-TT group and 99 children in the MenC-CRM group. The two treatments groups were comparable in terms of demographic characteristics (Table 1).
Immunogenicity
The pre-defined criterion assessing the primary immunogenicity objective of non-inferiority was reached; MenACWY-TT was shown to be non-inferior to MenC-CRM197 as the LL of the two-sided standardised asymptotic 95 % CI for the group difference (ACWY-TT group minus MenC-CRM group) in the percentage of children with rSBA-MenC vaccine response was −5.25 % (Table 2). Vaccine response rates for rSBA-MenC were 94.8 and 95.7 % in the ACWY-TT and the MenC-CRM groups, respectively.
At month 1, 99.3 % of the children who received MenACWY-TT had rSBA-MenC titres ≥1:128 compared with 100 % of the children who received MenC-CRM197 (Table 3). The rSBA-MenC GMTs increased 123-fold from pre- to post-vaccination in the ACWY-TT group versus 273-fold in the MenC-CRM group (Tables 3, also illustrated in Fig. 2). Exploratory analyses did not detect any statistically significant difference between the two groups in terms of percentages of children with rSBA-MenC titres ≥1:8 and ≥1:128 but suggested that rSBA-MenC GMTs adjusted for pre-vaccination measurements and age-strata were statistically significantly lower in the ACWY-TT group than in the MenC-CRM group.
Reverse cumulative curves for the ACWY-TT and MenC-CRM groups for rSBA-MenA (a), rSBA-MenC (b), rSBA-MenW-135 (c) and rSBA-MenY (d) (ATP cohort for immunogenicity). ACWY-TT group of children who received one dose of MenACWY-TT at month 0, MenCCRM group of children who received one dose of MenC-CRM197 at month 0. PRE pre-vaccination at month 0, PI(M1) post-vaccination at month 1
In the ACWY-TT group, vaccine response rates, percentages of children with rSBA titres ≥1:8 and percentages of children with rSBA titres ≥1:128 for each of the serogroups were at least 94.7, 99.7 and 99.3 %, respectively (Tables 2 and 3). rSBA GMTs for the four serogroups increased between 54-fold (rSBA-MenY) and 198-fold (rSBA-MenA) from pre- to post-vaccination in the children who received MenACWY-TT (Table 2, also illustrated in Fig. 2).
Safety
In the 2–5 years age stratum, redness was the most common solicited local symptom and was reported in 57/162 children (35.2 %) in the ACWY-TT group and 21/53 children (39.6 %) in the MenC-CRM group during the 4-day post-vaccination follow-up period (Fig. 3a). Redness was also the most frequently reported grade 3 solicited local symptom and was reported in 11/162 children (6.8 %) and 8/53 children (15.1 %) in the ACWY-TT and the MenC-CRM groups, respectively. In the 6–10 years age stratum, pain was the most frequently reported solicited local symptom, which was reported in 65/148 children (43.9 %) in the ACWY-TT group and 27/50 children (54.0 %) in the MenC-CRM group (Fig. 3b). Redness was the most common grade 3 solicited symptom and was reported in 9/148 children (6.1 %) and 5/50 children (10.0 %) in the ACWY-TT and the MenC-CRM groups, respectively.
Percentage of children in the 2–5 years age stratum (a) and in the 6–10 years age stratum (b) experiencing solicited local and general symptoms within the 4-day post-vaccination period (total vaccinated cohort). ACWY-TT group of children who received one dose of MenACWY-TT at month 0, MenC-CRM group of children who received one dose of MenC-CRM197 at month 0. Error bars represent 95 % confidence intervals
In the 2–5 years age stratum, the most common solicited general symptoms reported during the 4-day post-vaccination follow-up period were irritability in the ACWY-TT group (25/162 children [15.4 %]) and irritability and drowsiness in the MenC-CRM group (each in 6/53 children [11.3 %]) (Fig. 3a). In the 6–10 years age stratum, fatigue was the most frequently reported solicited general symptom in both groups and was reported in 33/148 children (22.3 %) and 11/50 children (22.0 %) in the ACWY-TT and the MenC-CRM groups, respectively (Fig. 3b). Headache was the second most frequently reported solicited general symptom in the ACWY-TT group (30/148 children [20.3 %]), while it was only reported in 4/50 children (8.0 %) in the MenC-CRM group. Grade 3 general symptoms were uncommonly reported in both treatments groups (between 0 and 2.7 % of the children across both age strata) (Fig. 3a, b). No children in either group had fever with grade 3 intensity (oral temperature >39.5 °C).
For the two age strata combined, unsolicited AEs were reported during the 31-day post-vaccination period in 55/311 children (17.7 %) and 20/103 children (19.4 %) in the ACWY-TT and the MenC-CRM groups, respectively. The most frequently reported unsolicited symptoms were fever in the ACWY-TT group (8/311 children [2.6 %]) and cough in the MenC-CRM group (3/103 children [2.9 %]). None of the children reported grade 3 unsolicited symptoms considered by the investigator to have a causal relationship to vaccination.
Throughout the entire study, two children reported each one new onset of chronic illness: one child in the ACWY-TT group reported chronic otitis media and one child in the MenC-CRM group reported allergy to arthropod bites. Rashes were reported in 8/311 children (2.6 %) in the ACWY-TT group and 1/103 child (1.0 %) in the MenC-CRM group and included dermatitis, eczema, rashes and skin exfoliation. One child in the ACWY-TT group reported urticaria 67 days post-vaccination, which resolved without sequelae and was not considered related to vaccination. AEs resulting in emergency room visit were reported in 11/311 (3.5 %) children in the ACWY-TT group and 1/103 child (1.0 %) in the MenC-CRM group.
Throughout the study, SAEs were observed in 6/311 children (1.9 %) who received MenACWY-TT: 4/163 children (2.5 %) in the 2–5 age stratum (convulsion, gastroesophageal reflux disease and nasopharyngitis, accidental poisoning and head injury) and 2/148 children (1.4 %) in the 6–10 age stratum (abdominal injury and appendicitis). One child (1.0 %) who received MenC-CRM197 (2–5 age stratum) reported one SAE (gastroenteritis). No SAEs were considered related to vaccination.
Discussion
In the Netherlands and Canada (Quebec), vaccination with a single dose of a monovalent conjugate vaccine against MenC given in the second year of life has resulted in a decrease of the incidence of diseases caused by this serogroup [14, 29, 54]. However, protection against the other major meningococcal serogroups is also needed, especially for travellers to areas of high endemicity. Currently, two quadrivalent meningococcal conjugate vaccines have been licensed in Europe: the MenACWY-CRM197 vaccine for immunisation of children 2 years of age and older and the MenACWY-TT vaccine that extends protection to include toddlers in the second year of life, an age group at high risk for meningococcal disease. The present study was primarily designed to demonstrate the non-inferiority of MenACWY-TT versus MenC-CRM197 in terms of immune response to MenC in children 2–10 years of age. In addition, the immunogenicity to MenA, MenW-135 and MenY, and the safety profile of MenACWY-TT were assessed.
The primary objective of the study was met, and the immunogenicity of a single dose of MenACWY-TT was shown to be non-inferior to that of MenC-CRM197 in terms of rSBA-MenC vaccine response. However, exploratory analyses suggested that lower rSBA-MenC GMTs were measured after vaccination with MenACWY-TT compared with MenC-CRM197. A similar finding was noted in a previous study conducted in infants showing that rSBA-MenC GMTs induced by the licensed MenACWY-CRM197 vaccine were lower than those induced by MenC-CRM197 [46]. These findings could be related to the differences in MenC capsular polysaccharide doses in MenACWY-TT or MenACWY-CRM197 (5 μg) as opposed to MenC-CRM197 (10 μg). Furthermore, the additional serogroups included in the quadrivalent vaccines compared to the monovalent vaccine may result in lower overall titres for MenC. Finally, it should be noted that, in contrast with MenACWY-TT and MenACWY-CRM197, MenC-CRM197 contains an aluminium adjuvant.
Results of our study are in contrast with those of other trials in which MenACWY-TT was compared to another monovalent MenC-CRM197 vaccine (Meningitec™; Pfizer, formerly Wyeth) [32, 58]. In these trials, MenACWY-TT was shown to induce higher rSBA-MenC GMTs than the monovalent MenC-CRM197 vaccine in toddlers. This difference is consistent with results of other studies showing that the immune response induced by MenC-CRM197 (Menjugate™) was higher than that induced by the other monovalent MenC-CRM197 vaccine (Meningitec™) [44, 47].
The lower rSBA-MenC GMTs induced by MenACWY-TT compared to MenC-CRM197 in the present study are of unknown clinical significance, since >99 % of children had rSBA-MenC titres ≥1:128 at 1 month post-vaccination, suggesting that MenACWY-TT induced seroprotective antibody titres against MenC in the vast majority of the vaccine recipients. However, the lower rSBA-MenC GMTs may have an impact on antibody persistence and this is being explored in an ongoing extension study (NCT01266993). The persistence of antibodies in the serum is particularly important for preventing diseases that have a short incubation period, such as meningococcal diseases, for which the memory B-cell responses are not sufficiently rapid to prevent bacterial dissemination [3, 42]. The lower rSBA-MenC GMTs must be considered in light of the additional robust responses to MenA, MenW-135 and MenY induced by MenACWY-TT, which indicate broader serogroup coverage than that induced by the monovalent MenC conjugate vaccine.
Currently, there is no international consensus on whether rabbit (rSBA) or human (hSBA) complement source should be considered as standard for bactericidal activity measurements [21, 28, 59]. Although the original correlate of protection was defined in terms of hSBA titres [20], it was previously suggested that hSBA assays may have reduced sensitivity and that while hSBA titres ≥1:4 are predictive of protection, hSBA titres <1:4 may not necessarily predict susceptibility [8, 21, 28]. Therefore, a functional assay using rabbit complement was used to evaluate the immunogenicity of the meningococcal vaccines in the present study. Moreover, three monovalent MenC vaccines were licensed in Europe based on rSBA-MenC responses, and during post-licensure surveillance, rSBA titres of 1:8 were confirmed as the antibody threshold that best correlated to vaccine effectiveness [1].
The safety profile of MenACWY-TT observed in our study was in line with that observed in a previous study conducted in young children in Europe [32]. However, solicited local symptoms seemed to be more frequently reported here than in another previous study conducted in children 2–10 years of age in the Philippines, India, Lebanon and Saudi Arabia [37]. The differences between the safety profiles may reflect differences between the populations in which the vaccine was studied, both in terms of biological reactogenicity to the vaccine and cultural differences in AE reporting.
The present study was limited by its open design, which had the potential to bias the safety reporting by the investigators and parents/guardians. However, since it is most likely that bias would be in favour of the control monovalent vaccine versus the quadrivalent vaccine, the results of the safety comparison remain relevant. The study was also potentially limited by the lack of MenC-TT or quadrivalent meningococcal conjugate vaccines as control and the numerous exploratory statistical comparisons without multiplicity adjustment, which should be interpreted with caution.
The results of the present study suggest that MenACWY-TT has a clinically acceptable safety profile and the potential to offer protection against meningococcal disease to European children 2–10 years of age, since the vaccine was shown to provide protection against additional serogroups while maintaining protection against serogroup C.
Menactra is a trademark of Sanofi Pasteur.
Menveo and Menjugate are trademarks of Novartis Vaccines and Diagnostics, Inc.
Meningitec is a trademark of Pfizer, formerly Wyeth.
Nimenrix is a trademark of the GlaxoSmithKline Group of companies.
References
Andrews N, Borrow R, Miller E (2003) Validation of serological correlate of protection for meningococcal C conjugate vaccine by using efficacy estimates from postlicensure surveillance in England. Clin Diagn Lab Immunol 10:780–786
Antignac A, Ducos-Galand M, Guiyoule A, Pirès R, Alonso J-M, Taha M-K (2003) Neisseria meningitidis strains isolated from invasive infections in France (1999–2002): phenotypes and antibiotic susceptibility patterns. Clin Infect Dis 37:912–920
Auckland C, Gray S, Borrow R, Andrews N, Goldblatt D, Ramsay M, Miller E (2006) Clinical and immunological risk factors for meningococcal C conjugate vaccine failure in the United Kingdom. J Infect Dis 194:1745–1752
Bermal N, Huang L-M, Dubey AP, Jain H, Bavdekar A, Lin T-Y, Bianco V, Baine Y, Miller JM (2011) Safety and immunogenicity of a tetravalent meningococcal serogroups A, C, W-135 and Y conjugate vaccine in adolescents and adults. Hum Vaccin 7:239–247
Bettinger JA, Scheifele DW, Le Saux N, Halperin SA, Vaudry W, Tsang R (2009) The impact of childhood meningococcal serogroup C conjugate vaccine programs in Canada. Pediatr Infect Dis J 28:220–224
Bidmos FA, Neal KR, Oldfield NJ, Turner DP, Ala’aldeen DA, Bayliss CD (2011) Persistence, replacement, and rapid clonal expansion of meningococcal carriage isolates in a 2008 university student cohort. J Clin Microbiol 49:506–512
Black S, Klein NP, Shah J, Bedell L, Karsten A, Dull PM (2010) Immunogenicity and tolerability of a quadrivalent meningococcal glycoconjugate vaccine in children 2–10 years of age. Vaccine 28:657–663
Borrow R, Andrews N, Goldblatt D, Miller E (2001) Serological basis for use of meningococcal serogroup C conjugate vaccines in the United Kingdom: reevaluation of correlates of protection. Infect Immun 69:1568–1573
Borrow R, Balmer P, Miller E (2005) Meningococcal surrogates of protection-serum bactericidal antibody activity. Vaccine 23:2222–2227
Borrow R, Miller E (2006) Long-term protection in children with meningococcal C conjugate vaccination: lessons learned. Expert Rev Vaccines 5:851–857
Bryant KA, Marshall GS, Marchant CD, Pavia-Ruiz N, Nolan T, Rinderknecht S, Blatter M, Aris E, Lestrate P, Boutriau D, Friedland LR, Miller JM (2011) Immunogenicity and safety of H influenzae type b–N meningitidis C/Y conjugate vaccine in infants. Pediatrics 127:e1375–e1385
Centers for Disease Control and Prevention (2006) Inadvertent misadministration of meningococcal conjugate vaccine-United States, June–August 2005. MMWR Morb Mortal Wkly Rep 55:1016–1017
de Voer RM, Mollema L, Schepp RM, de Greeff SC, van Gageldonk PG, de Melker HE, Sanders EA, Berbers GA, van der Klis FR (2010) Immunity against Neisseria meningitidis serogroup C in the Dutch population before and after introduction of the meningococcal C conjugate vaccine. PLoS One 5:e12144
De Wals P, Deceuninck G, Lefebvre B, Boulianne N, De Serres G (2011) Effectiveness of serogroup C meningococcal conjugate vaccine: a 7-year follow-up in Quebec, Canada. Pediatr Infect Dis J 30:566–569
European Centre for Disease Prevention and Control (2012). Summary chart, vaccination schedule for France. http://ecdc.europa.eu/en/activities/surveillance/euvac/schedules/Pages/france.aspx. Accessed 21 Nov 2012
European Medicines Agency (2012).Assessment report Nimenrix. Procedure N0. EMAE/H/C/002226. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002226/WC500127664.pdf. Accessed 20 July 2012)
European Union Invasive Bacterial Infections Surveillance (EU-IBIS) Network (2007) Invasive Neisseria meningitis in Europe 2006. Health Protection Agency, London 2006. http://www.hpa-bioinformatics.org.uk/euibis/documents/2006_meningo.pdf. Accessed 02 Apr 2012
Findlow J, Balmer P, Yero D, Niebla O, Pajón R, Borrow R (2007) Neisseria vaccines 2007. Expert Rev Vaccines 6:485–489
Gold R, Lepow ML, Goldschneider I, Draper TF, Gotshlich EC (1979) Kinetics of antibody production to group A and group C meningococcal polysaccharide vaccines administered during the first six years of life: prospects for routine immunization of infants and children. J Infect Dis 140:690–697
Goldschneider I, Gotschlich EC, Artenstein MS (1969) Human immunity to the meningococcus. J Exp Med 129:1307–1326
Granoff DM (2009) Relative importance of complement-mediated bactericidal and opsonic activity for protection against meningococcal disease. Vaccine 27:B117–B125
Gray SJ, Trotter CL, Ramsay ME, Guiver M, Fox AJ, Borrow R, Mallard RH, Kaczmarski EB (2006) Epidemiology of meningococcal disease in England and Wales 1993/94 to 2003/04: contribution and experiences of meningococcal reference unit. J Med Microbiol 55:887–896
Harrison LH (2006) Prospects for vaccine prevention of meningococcal infection. Clin Microbiol Rev 19:142–164
Harrison LH, Trotter CL, Ramsay ME (2009) Global epidemiology of meningococcal disease. Vaccine 27:B51–B63
Hassan-King MK, Wall RA, Greenwood BM (1988) Meningococcal carriage, meningococcal disease and vaccination. J Infect 16:55–59
Hellenbrand W, Elias J, Wichmann O, Dehnert M, Frosch M, Vogel U (2012) Epidemiology of invasive meningococcal disease in Germany, 2002–2010, and impact of vaccination with meningococcal C conjugate vaccine. J Infect. doi:10.1016/j.jinf.2012.09.008
Jackson LA, Baxter R, Reisinger K, Karsten A, Shah J, Bedell L, Dull PM (2009) Phase III comparison of an investigational quadrivalent meningococcal conjugate vaccine with the licensed meningococcal ACWY conjugate vaccine in adolescents. Clin Infect Dis 49:e1–e10
Jodar L, Cartwright K, Feavers IM (2000) Standardisation and validation of serological assays for the evaluation of immune responses to Neisseria meningitidis serogroup A and C vaccines. Biologicals 28:193–197
Kaaijk P, van der Ende A, Berbers G, van den Dobbelsteen GP, Rots NY (2012) Is a single dose of meningococcal serogroups C conjugate vaccine sufficient for protection? Experience from the Netherlands. BMC Infect Dis 12:35. doi:10.1186/1471-2334-12-35
Keyserling H, Papa T, Koranyi K, Ryall R, Bassily E, Bybel MJ, Sullivan K, Gilmet G, Reinhardt A (2005) Safety, immunogenicity, and immune memory of a novel meningococcal (groups A, C, Y, and W-135) polysaccharide diphtheria toxoid conjugate vaccine (MCV-4) in healthy adolescents. Arch Pediatr Adolesc Med 159:907–913
Kinlin LM, Jamieson F, Brown EM, Brown S, Rawte P, Dolman S, Drews SJ, Fisman DN (2009) Rapid identification of herd effects with the introduction of serogroup C meningococcal conjugate vaccine in Ontario, Canada, 2000–2006. Vaccine 27:1735–1740
Knuf M, Kieninger-Baum D, Habermehl P, Muttonen P, Maurer H, Vink P, Poolman J, Boutriau D (2010) A dose-range study assessing immunogenicity and safety of one dose of a new candidate meningococcal serogroups A, C, W-135, Y tetanus toxoid conjugate (MenACWY-TT) vaccine administered in the second year of life and in young children. Vaccine 28:744–753
Larrauri A, Cano R, Garcia M, Mateo S (2005) Impact and effectiveness of meningococcal C conjugate vaccine following its introduction in Spain. Vaccine 23:4097–4100
MacDonald NE, Halperin SA, Law BJ, Forrest B, Danzig LE, Granoff DM (1998) Induction of immunologic memory by conjugated vs plain meningococcal C polysaccharide vaccine in toddlers: a randomized controlled trial. JAMA 280:1685–1689
Maiden MC, Ibarz-Pavon AB, Urwin R, Gray SJ, Andrews NJ, Clarke SC, Walker AM, Evans MR, Kroll JS, Neal KR et al (2008) Impact of meningococcal serogroup C conjugate vaccines on carriage and herd immunity. J Infect Dis 197:737–743
Maslanka SE, Gheesling LL, Libutti DE, Donaldson KB, Harakeh HS, Dykes JK, Arhin FF, Devi SJ, Frasch CE, Huang JC et al (1997) Standardization and a multilaboratory comparison of Neisseria meningitidis serogroup A and C serum bactericidal assays. Clin Diagn Lab Immunol 4:156–167
Memish ZA, Dbaibo G, Montellano M, Verghese VP, Jain H, Dubey AP, Bianco V, Van der Wielen M, Gatchalian S, Miller JM (2011) Immunogenicity of a single dose of tetravalent meningococcal serogroups A, C, W-135, and Y conjugate vaccine administered to 2- to 10-year-olds is noninferior to a licensed-ACWY polysaccharide vaccine with an acceptable safety profile. Pediatr Infect Dis J 30:e56–e62
Morley SL, Pollard AJ (2001) Vaccine prevention of meningococcal disease, coming soon? Vaccine 20:666–687
Parent du Châtelet I, Barboza P, Taha MK (2012) W135 invasive meningococcal infections imported from Sub-Saharan Africa to France, January to April 2012. Eur Surveill 17(21) pii=20181
Pichichero M, Casey J, Blatter M, Rothstein E, Ryall R, Bybel M, Gilemt G, Papa T (2005) Comparative trial of the safety and immunogenicity of quadrivalent (A, C, Y, W-135) meningococcal polysaccharide-diphtheria conjugate vaccine versus quadrivalent polysaccharide vaccine in two- to ten-year-old children. Pediatr Infect Dis J 24:57–62
Pollard AJ (2004) Global epidemiology of meningococcal disease and vaccine efficacy. Pediatr Infect Dis J 23:S274–S279
Pollard AJ, Perrett KP, Beverley PC (2009) Maintaining protection against invasive bacteria with protein–polysaccharide conjugate vaccines. Nat Rev Immunol 9:213–220
Ramsay ME, Andrews N, Kaczmarski EB, Miller E (2001) Efficacy of meningococcal serogroup C conjugate vaccine in teenagers and toddlers in England. Lancet 357:195–196
Richmond P, Borrow R, Goldblatt D, Findlow J, Martin S, Morris R, Cartwright K, Miller E (2001) Ability of 3 different meningococcal C conjugate vaccines to induce immunologic memory after a single dose in UK toddlers. J Infect Dis 183:160–163
Slinko VG, Sweeny A (2007) Reduction of invasive meningococcal disease in Queensland: a success for immunisation. Commun Dis Intell 31:227–232
Snape MD, Perrett KP, Ford KJ, John TM, Pace D, Yu LM, Langley JM, McNeil S, Dull PM, Ceddia F et al (2008) Immunogenicity of a tetravalent meningococcal glycoconjugate vaccine in infants: a randomized controlled trial. JAMA 299:173–184
Southern J, Borrow R, Andrews N, Morris R, Waight P, Hudson M, Balmer P, Findlow H, Findlow J, Miller E (2009) Immunogenicity of a reduced schedule of meningococcal group C conjugate vaccine given concomitantly with the Prevenar and Pediacel vaccines in healthy infants in the United Kingdom. Clin Diagn Lab Immunol 16:194–199
Sow SO, Okoko BJ, Diallo A, Viviani S, Borrow R, Carlone G, Tapia M, Akinsola AK, Arduin P, Findlow H et al (2011) Immunogenicity and safety of a meningococcal A conjugate vaccine in Africans. N Engl J Med 364:2293–2304
Stephens DS (2007) Conquering the meningococcus. FEMS Microbiol Rev 31:3–14
Tan LK, Carlone GM, Borrow R (2010) Advances in the development of vaccines against Neisseria meningitidis. N Engl J Med 362:1511–1520
The European Meningococcal Disease Society (EMGM). 11th EMGM Meeting, May 18–20, 2011, Ljubljana, Slovenia. Poster abstracts: Emergence of serogroup Y: P035-040
Thulin HS, Toros B, Fredlund H, Olcen P, Molling P (2011) Genetic characterisation of the emerging invasive Neisseria meningitidis serogroup Y in Sweden, 2000 to 2010. Euro Surveill 16
Trotter CL, Andrews NJ, Kaczmarski EB, Miller E, Ramsay ME (2004) Effectiveness of meningococcal serogroup C conjugate vaccine 4 years after introduction. Lancet 364:365–367
Trotter CL, Chandra M, Cano R, Larrauri A, Ramsay ME, Brehony C, Jolley KA, Maiden MC, Heuberger S, Frosch M (2007) A surveillance network for meningococcal disease in Europe. FEMS Microbiol Rev 31:27–36
Tsolia MN, Theodoridou M, Tzanakaki G, Vlachou V, Mostrou G, Stripeli F, Kalabalikis P, Pangalis A, Kafetzis D, Kremastinou J, Konstantopoulos A (2006) Invasive meningococcal disease in children in Greece: comparison of serogroup A disease with disease caused by other serogroups. Eur J Clin Microbiol Infect Dis 25:449–456
US Food and Drug Administration (2011) Approval letter—Menactra. http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm252511.htm. Accessed 30 Mar 2012
US Food and Drug Administration (2011) Menveo; Full prescribing information. http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm201342.htm.Accessed 19 July 2012
Vesikari T, Karvonen A, Bianco V, Van der Wielen M, Miller J (2011) Tetravalent meningococcal serogroups A, C, W-135 and Y conjugate vaccine is well tolerated and immunogenic when co-administered with measles-mumps-rubella-varicella vaccine during the second year of life. Vaccine 29:4274–4284
World Health Organization (2006) Recommendations to assure the quality, safety and efficacy of group A meningococcal conjugate vaccines. Geneva, Switzerland: WHO Press; Report No: WHO/BS/06.2041
Acknowledgments
The authors are indebted to the study participants and their parents, clinicians, nurses and laboratory technicians at the study site as well as to clinical investigators for their contribution to this study. In particular, we thank Drs. Campagne, Helm, Hoernlein, Mai and Vocks-Hauck. We are also grateful to all the teams of GlaxoSmithKline Vaccines for their contribution to this study, including N. Clyti and W. Kroeniger for their assistance in coordination of the study, M. Franco for his input into study reports preparation, D. Boutriau for input into study design, F. Celzo and A. Stukkens for input into protocol development, and K Maleux and P Lestrate for conducting laboratory assays. The authors also thank Juliette Gray and Virginie Durbecq (XPE Pharma & Science, Belgium c/o GlaxoSmithKline Vaccines) for publication management and Claire Verbelen (XPE Pharma & Science, Belgium) for medical writing services.
Conflicts of interest
Dr. M. Knuf received compensations for presentations and participation in Advisory Boards with regard to MenACWY vaccines from GlaxoSmithKline group of companies and Novartis. Dr. M. Knuf received compensations for consultancy from GlaxoSmithKline group of companies, Novartis, Pfizer, Baxter and SPMSD. Dr. M. Knuf received compensations for lectures from GlaxoSmithKline group of companies, Novartis and SPMSD. Dr. M. Knuf received support for meetings, travel or accommodation expenses from GlaxoSmithKline group of companies, Baxter and Novartis. Dr. M. Knuf received compensations for writing and review activities from Novartis. Dr. D. Kieninger-Baum received support for meetings, travel or accommodation expenses from GlaxoSmithKline group of companies, Pfizer-Wyeth and Novartis. Dr. D. Kieninger-Baum received compensations for lectures from GlaxoSmithKline group of companies and Pfizer-Wyeth. Dr. D. Kieninger-Baum’s institute received reimbursement for study performance from GlaxoSmithKline group of companies, Pfizer-Wyeth, Novartis and Sanofi Pasteur. Dr. O. Romain received compensation for lectures and presentations from GlaxoSmithKline group of companies. Y. Baine, V. Bianco and Dr. J. Miller are employees of GlaxoSmithKline group of companies. Y. Baine and Dr. J. Miller declare stock ownership in GlaxoSmithKline group of companies. Dr. H. Pankow-Culot, Dr. U. Walther, Dr P.H. Tran, Dr K. Klaus and Dr. T. Fischbach have no conflict of interest to disclose.
Source of funding
GlaxoSmithKline Biologicals SA was the funding source and was involved in all stages of the study conduct and analysis. GlaxoSmithKline Biologicals SA also took responsibility for all costs associated with the development and publishing of the present manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Knuf, M., Romain, O., Kindler, K. et al. Immunogenicity and safety of the quadrivalent meningococcal serogroups A, C, W-135 and Y tetanus toxoid conjugate vaccine (MenACWY-TT) in 2–10-year-old children: results of an open, randomised, controlled study. Eur J Pediatr 172, 601–612 (2013). https://doi.org/10.1007/s00431-012-1924-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-012-1924-0