Abstract
Purpose
To prospectively report the perimetric defects during a 6-month follow-up (FU) in patients with initially active ocular toxoplasmosis (OT).
Methods
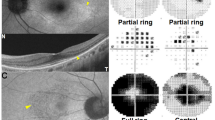
Twenty-four patients were studied, including 11 eyes with chorioretinal toxoplasmosis proven with a positive aqueous humor sample and 13 eyes with a biologically unproven, chorioretinal lesion. Automated 24-2 SITA-Standard visual fields were performed at baseline, at the first, and sixth months of FU. A composite clinical severity score was calculated from visual acuity (VA), severity of vitreitis, chorioretinal lesion size, location of the lesion in zone 1, the presence of an initial macular or papillary edema, and long-term scarring. This provided a relative cutoff level of severity. Nine eyes out of the 24 eyes were considered severe (3 unproven and 6 proven OT).
Results
Initial and final visual field parameters (mean deviation [MD] and pattern standard deviation [PSD]) were significantly correlated (r = 0.873; p < 0.001, and r = 0.890; p < 0.001, respectively). During FU, only foveal threshold [FT] was correlated with VA at baseline (r = 0.48; p = 0.01) and at the 6-month FU visit (r = 0.547; p = 0.004). The MD initial predictive value of clinical severity was 0.739 according to the ROC curve. At baseline, severe and nonsevere OT exhibited no significant difference in term of MD (p = 0.06) and PSD (p = 0.1). During the FU, taking into account all the data, MD, PSD, visual function index [VFI], and FT were associated with the severity of toxoplasmosis (p = 0.018, 0.05, 0.016, and 0.02, respectively): the unproven group had a faster recovery of MD during FU (p = 0.05).
Conclusion
Visual field parameters better reflected the chorioretinal destruction related to the toxoplasmosis lesion and the functional repercussions than VA alone. Interestingly, MD at presentation could be a discriminating factor of severity in active OT, and each visual field parameter follow-up could be a support to manage patients with active OT, especially in the severe group.





Similar content being viewed by others
References
Montoya J, Liesenfeld O (2004) Toxoplasmosis. Lancet 363(9425):1965–1976
Furtado JM, Winthrop KL, Butler NJ et al (2013) Ocular toxoplasmosis I: parasitology, epidemiology and public health: ocular toxoplasmosis. Clin Exp Ophthalmol 41(1):82–94
Holland GN (2003) Ocular toxoplasmosis: a global reassessment. Am J Ophthalmol 136(6):973–988
Holland GN (2004) Ocular toxoplasmosis: a global reassessment. Am J Ophthalmol 137(1):1–17
Pleyer U, Schlüter D, Mänz M (2014) Ocular toxoplasmosis: recent aspects of pathophysiology and clinical implications. Ophthalmic Res 52(3):116–123
Weiss LM, Dubey JP (2009) Toxoplasmosis: a history of clinical observations. Int J Parasitol 39(8):895–901
Wilder HC (1952) Toxoplasma chorioretinitis in adults. Arch Ophthalmol 48(2):127–136
Dodds EM, Holland GN, Stanford MR et al (2008) Intraocular inflammation associated with ocular toxoplasmosis: relationships at initial examination. Am J Ophthalmol 146(6):856–865.e2
Martin WG, Brown GC, Parrish RK et al (1980) Ocular toxoplasmosis and visual field defects. Am J Ophthalmol 90(1):25–29
Schlaegel TF, Weber JC (1984) The macula in ocular toxoplasmosis. Arch Ophthalmol 102(5):697–698
Stanford MR (2005) The visual field in toxoplasmic retinochoroiditis. Br J Ophthalmol 89(7):812–814
Scherrer J, Iliev ME, Halberstadt M et al (2007) Visual function in human ocular toxoplasmosis. Br J Ophthalmol 91(2):233–236
Delair E, Latkany P, Noble AG et al (2011) Clinical manifestations of ocular toxoplasmosis. Ocul Immunol Inflamm 19(2):91–102
Commodaro AG, Belfort RN, Rizzo LV et al (2009) Ocular toxoplasmosis: an update and review of the literature. Mem Inst Oswaldo Cruz 104(2):345–350
Garweg JG, de Groot-Mijnes JDF, Montoya JG (2011) Diagnostic approach to ocular toxoplasmosis. Ocul Immunol Inflamm 19(4):255–261
Goldmann H, Witmer R (1954) Antikörper im Kammerwasser. Ophthalmologica 127(4–5):323–330
Fekkar A, Bodaghi B, Touafek F et al (2008) Comparison of immunoblotting, calculation of the Goldmann-Witmer coefficient, and real-time PCR using aqueous humor samples for diagnosis of ocular toxoplasmosis. J Clin Microbiol 46(6):1965–1967
Villard O, Filisetti D, Roch-Deries F et al (2003) Comparison of enzyme-linked immunosorbent assay, immunoblotting, and PCR for diagnosis of Toxoplasmic chorioretinitis. J Clin Microbiol 41(8):3537–3541
Fardeau C, Romand S, Rao NA et al (2002) Diagnosis of toxoplasmic retinochoroiditis with atypical clinical features. Am J Ophthalmol 134(2):196–203
Cunningham ET (2011) Proportionate topographic areas of retinal zones 1, 2, and 3 for use in describing infectious retinitis. Arch Ophthalmol 129(11):1507
European Glaucoma Society (ed) (2014) Terminology and guidelines for glaucoma, 4th edn. PubliComm, Savona, p 195
Standardization of Uveitis Nomenclature for Reporting Clinical Data (2005) Results of the first international workshop. Am J Ophthalmol 140(3):509–516
Ouyang Y, Pleyer U, Shao Q et al (2014) Evaluation of cystoid change phenotypes in ocular toxoplasmosis using optical coherence tomography. PLoS One 9(2):e86626
Diniz B, Regatieri AR et al (2011) Evaluation of spectral domain and time domain optical coherence tomography findings in toxoplasmic retinochoroiditis. Clin Ophthalmol:645–647
Monnet D (2009) Optical coherence tomography in ocular toxoplasmosis. Int J Med Sci:137–138
Smith JR, Cunningham ET (2002) Atypical presentations of ocular toxoplasmosis. Curr Opin Ophthalmol 13(6):387–392
Song A, Scott IU, Davis JL et al (2002) Atypical anterior optic neuropathy caused by toxoplasmosis. Am J Ophthalmol 133(1):162–164
Mets MB, Holfels E, Boyer KM et al (1997) Eye manifestations of congenital toxoplasmosis. Am J Ophthalmol 123(1):1–16
Maenz M, Schlüter D, Liesenfeld O et al (2014) Ocular toxoplasmosis past, present and new aspects of an old disease. Prog Retin Eye Res 39:77–106
Riemslag FCC, Brinkman CJJ, Lunel HFEV et al (1992) Analysis of the electroretinogram in toxoplasma retinochorioiditis. Doc Ophthalmol 82(1–2):57–63
Acknowledgments
Association for Research and Teaching in Ophthalmology (ARFO, Grenoble, France), DRCI (Grenoble University Hospital).
Other participating investigators:
Guillemot C., MD, Department of Ophthalmology, University Hospital, Saint Etienne, France.
Fricker-Hidalgo H., MD, Department of Parasitology, University Hospital, Grenoble, France.
Brenier-Pinchart M.P., MD, Department of Parasitology, University Hospital, Grenoble, France.
Lesoin A., MD, Department of Ophthalmology, University Hospital, Grenoble, France and Grenoble Alpes University, Grenoble, F-38041, France.
Funding
This study was funded by grant number IRB 2009-A00877-50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Blot, J., Aptel, F., Chumpitazi, B.F.F. et al. Monitoring of visual field over 6 months after active ocular toxoplasmosis. Graefes Arch Clin Exp Ophthalmol 257, 1481–1488 (2019). https://doi.org/10.1007/s00417-019-04313-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04313-2