Abstract
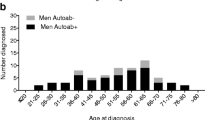
Patients with primary Sjogren’s syndrome (pSS) may go undiagnosed or be misclassified due to the insidious nature and wide spectrum of the disease. The available several classification criteria emphasize glandular findings. We aimed to analyze the efficiency of various classification criteria sets in patients diagnosed on the clinical basis by expert opinion and to compare those pSS patients who fulfilled these criteria with those who did not. This is a multicenter study in which 834 patients from 22 university-based rheumatology clinics are included. Diagnosis of pSS was made on the clinical basis by the expert opinion. In this study, we only interviewed patients once and collected available data from the medical records. The European criteria, American-European Consensus Group (AECG) and American College of Rheumatology (ACR) Sjogren’s criteria were applied. Majority of the patients were women (F/M was 20/1). The median duration from the first pSS-related symptom to diagnosis was significantly shorter in men (2.5 ± 2.3 vs 4.3 ± 5.9 years) (p = 0 < 0.016). When the European, AECG and ACR Sjogren’s criteria were applied, 666 patients (79.9%) satisfied at least one of them. In total, 539 patients (64.4%) satisfied the European, 439 (52.6%) satisfied the AECG, and 359 (43%) satisfied the ACR criteria. Among the entire group, 250 patients (29.9%) satisfied all and 168 (20.1%) met none of the criteria. The rates of extraglandular organ involvements were not different between patients who met at least one of the criteria sets and those who met none. There is an urgent need for the modification of the pSS criteria sets to prevent exclusion of patients with extraglandular involvements as the dominant clinical features.

Similar content being viewed by others
References
Patel R, Shahane A (2014) The epidemiology of Sjögren’s syndrome. Clin Epidemiol 6:247–255
Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH (2002) Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. European Study Group on Classification Criteria for Sjögren’s Syndrome. Ann Rheum Dis 61(6):554–558
Shiboski SC, Shiboski CH, Criswell L, Baer A, Challacombe S, Lanfranchi H, Schiødt M, Umehara H, Vivino F, Zhao Y, Dong Y, Greenspan D, Heidenreich AM, Helin P, Kirkham B, Kitagawa K, Larkin G, Li M, Lietman T, Lindegaard J, McNamara N, Sack K, Shirlaw P, Sugai S, Vollenweider C, Whitcher J, Wu A, Zhang S, Zhang W, Greenspan J, Daniels T; Sjögren’s International Collaborative Clinical Alliance (SICCA) Research Groups (2012) American College of Rheumatology classification criteria for Sjögren’s syndrome: a data-driven, expert consensus approach in the Sjögren’s International Collaborative Clinical Alliance cohort. Arthritis Care Res (Hoboken) 64(4):475–487
Alamanos Y, Tsifetaki N, Voulgari PV, Venetsanopoulou AI, Siozos C, Drosos AA (2006) Epidemiology of primary Sjögren’s syndrome in north-west Greece, 1982–2003. Rheumatology (Oxford) 45(2):187–191
vanBijsterveld OP (1969) Diagnostic tests in the Sicca syndrome. Arch Ophthalmol 82(1):10–14
Rasmussen A, Ice JA, Li H, Grundahl K, Kelly JA, Radfar L, Stone DU, Hefner KS, Anaya JM, Rohrer M, Gopalakrishnan R, Houston GD, Lewis DM, Chodosh J, Harley JB, Hughes P, Maier-Moore JS, Montgomery CG, Rhodus NL, Farris AD, Segal BM, Jonsson R, Lessard CJ, Scofield RH, Sivils KL (2014) Comparison of the American-European Consensus Group Sjogren’s syndrome classification criteria to newly proposed American College of Rheumatology criteria in a large, carefully characterised sicca cohort. Ann Rheum Dis 73(1):31–38. doi:10.1136/annrheumdis-2013-203845
Vitali C, Bombardieri S, Moutsopoulos HM, Coll J, Gerli R, Hatron PY et al (1996) Assessment of the European classification criteria for Sjogren’s syndrome in a series of clinically defined cases: results of a prospective multicentre study. The European Study Group on Diagnostic Criteria for Sjogren’s syndrome. Ann Rheum Dis 55:116–121
Cornec D, Saraux A, Cochener B, Pers JO, Jousse-Joulin S, Renaudineau Y, Marhadour T (2014) Devauchelle-PensecVLevel of agreement between 2002 American-European Consensus Group and 2012 American College of Rheumatology classification criteria for Sjögren’s syndrome and reasons for discrepancies. Arthritis Res Ther 16(2):R74
Vitali C, Bootsma H, Bowman SJ, Dorner T, Gottenberg JE, Mariette X, Ramos-Casals M, Ravaud P, Seror R, Theander E, Tzioufas AG (2013) Classification criteria for Sjogren’s syndrome: we actually need to definitively resolve the long debate on the issue. Ann Rheum Dis 72(4):476–478
Brun JG, Madland TM, Gjesdal CB, Bertelsen LT (2002) Sjögren’s syndrome in an out-patient clinic: classification of patients according to the preliminary European criteria and the proposed modified European criteria. Rheumatology (Oxford) 41(3):301–304
Vitali C, Bombardieri S, Moutsopoulos HM, Balestrieri G, BencivelliW, Bernstein RM et al (1993) Preliminary criteria for the classification of Sjögren’s syndrome. Results of a prospective concerted action supported by the European Community. Arthritis Rheum 36(3):340–347
Malladi AS, Sack KE, Shiboski SC, Shiboski CH, Baer AN, Banushree R, Dong Y, Helin P, Kirkham BW, Li M, Sugai S, Umehara H, Vivino FB, Vollenweider CF, Zhang W, Zhao Y, Greenspan JS, Daniels TE, Criswell LA (2012) Primary Sjögren’s syndrome as a systemic disease: a study of participants enrolled in an international Sjögren’s syndrome registry. Arthritis Care Res (Hoboken) 64(6):911–918
Hsu CW, Su YJ, Chang WN, Tsai NW, Chiu WC, Cheng BC, Su CM, Huang CR, Chang YT, Lu CH (2014) The association between serological biomarkers and primary Sjogren’s syndrome associated with peripheral polyneuropathy. Biomed Res Int 2014:902492
Ryu YS, Park SH, Lee J, Kwok SK, Ju JH, Kim HY, Jeon CH (2013) Follow-up of primary Sjogren’s syndrome patients presenting positive anti-cyclic citrullinated peptides antibody. Rheumatol Int )(Issue 6):1443
Manuel Ramos-Casals, Pilar Brito-Zerón, Raphaèle Seror, Hendrika Bootsma, Simon J. Bowman, Thomas Dörner, Jacques-Eric Gottenberg, Xavier Mariette, ElkeTheander, Stefano Bombardieri, ,Salvatore De Vita, Thomas Mandl, Wan-Fai Ng, AikeKruize, AthanasiosTzioufas and Claudio Vitali on behalf of the EULAR Sjögren Characterization of systemic disease in primary Sjögren’s syndrome: EULAR-SS Task Force recommendations for articular, cutaneous, pulmonary and renal involvements (2015) Rheumatology (Oxford) 54(12):2230–2238
Palm O, Garen T, Berge Enger T, Jensen JL, Lund MB, Aaløkken TM, Gran JT (2013) Clinical pulmonary involvement in primary Sjogren’s syndrome: prevalence, quality of life and mortality–a retrospective study based on registry data. Rheumatology (Oxford) 52(1):173–179
Brito-Zerón P, Retamozo S, Akasbi M, Gandía M, Perez-De-Lis M, Soto-Cardenas MJ, Diaz-Lagares C, Kostov B, Bove A, Bosch X, Perez-Alvarez R, Siso A (2014) Ramos-Casals M. Annular erythema in primary Sjogren’s syndrome: description of 43 non-Asian cases. Lupus 23(2):166–175
Teppo H, Revonta M (2007) A follow-up study of minimally invasive lip biopsy in the diagnosis of Sjögren’s syndrome. Clin Rheumatol 26(7):1099–1103
Plesivcnik Novljan M, Rozman B, Hocevar A, Grmek M, Kveder T, Tomsic M (2004) Incidence of primary Sjogren’s syndrome in Slovenia. Ann Rheum Dis 63:874–876
Karabulut G, Kitapcioglu G, Inal V, Kalfa M, Yargucu F, Keser G, Emmungil H, Gokmen NM, Kocanaogullari H, Aksu K (2011) Cigarette smoking in primary Sjögren’s syndrome: positive association only with ANA positivity. Mod Rheumatol 21(6):602–607
Goules AV, Tzioufas AG, Moutsopoulos HM (2014) Classification criteria of Sjögren’s syndrome. J Autoimmun. 48–49: 42–45
Shiboski CH, Siboski SC, Seror R, Criswell LA, Labetoulle M, Lietman A, Rasmussen A, Scofield H, Vitali C, Bowman SJ, Mariette X, the International Sjögren’s Syndrome Criteria Working Group (2017) 2016 American College of Rheumatology/European Leagues Against Rheumatism classification criteria for primary Sjögren’s syndrome: a consensus and data driven methodology involving three international patient cohorts. Ann Rheum Dis 76:9–16
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kabasakal, Yasemin, M.D., Kitapcıoğlu, Gül, Karabulut, Gonca, M.D., Tezcan, Mehmet E., M.D., Balkarlı, Ayşe, M.D., Aksoy, Adem, M.D., Yavuz, Şule, M.D., Yılmaz, Sema, M.D., Kaşifoğlu, Timuçin, M.D., Kalyoncu, Umut, M.D., Dalkılıç, Ediz, M.D., Tufan, Abdurrahman, M.D., Mercan, Rıdvan, M.D., Yıldız, Fatih, M.D., Şentürk, Taşkın, M.D., Önen, Fatoş, M.D., Bes, Cemal, M.D., Erken, Eren, M.D., Tunç, Ercan, M.D., Kamalı, Sevil, M.D., Tarhan, Emine, M.D., Yazıcı, Ayten, M.D., Düzgün, Nurşen, M.D., Bıçakçıgil, Müge, M.D., Yılmaz, Sedat, M.D., Özmen, Mustafa, M.D., Öcal, Lale, M.D., Alibaz-Öner, Fatma, M.D., Solmaz, Dilek, M.D., Çobankara, Veli, M.D., Nalbant, Selim, M.D., Kasapoğlu Günal, Esen, M.D., Kaskari, Derya, M.D., Göker, Berna, M.D., declare that they have no conflict of interest related to this manuscript to disclose.
Financial support
This study was funded by the Rheumatology Society of Turkey (TRD) (award recipient is Yasemin Kabasakal, M.D.).
Rights and permissions
About this article
Cite this article
Kabasakal, Y., Kitapçıoğlu, G., Karabulut, G. et al. Criteria sets for primary Sjogren’s syndrome are not adequate for those presenting with extraglandular organ involvements as their dominant clinical features. Rheumatol Int 37, 675–684 (2017). https://doi.org/10.1007/s00296-017-3691-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3691-8