Abstract
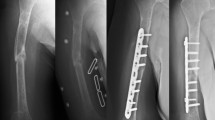
The intention of the current article is to review the epidemiology with related socioeconomic costs, pathophysiology, and treatment options for diaphyseal long bone delayed unions and nonunions. Diaphyseal nonunions in the tibia and in the femur are estimated to occur 4.6–8% after modern intramedullary nailing of closed fractures with an even much higher risk in open fractures. There is a high socioeconomic burden for long bone nonunions mainly driven by indirect costs, such as productivity losses due to long treatment duration. The classic classification of Weber and Cech of the 1970s is based on the underlying biological aspect of the nonunion differentiating between “vital” (hypertrophic) and “avital” (hypo−/atrophic) nonunions, and can still be considered to represent the basis for basic evaluation of nonunions. The “diamond concept” units biomechanical and biological aspects and provides the pre-requisites for successful bone healing in nonunions. For humeral diaphyseal shaft nonunions, excellent results for augmentation plating were reported. In atrophic humeral shaft nonunions, compression plating with stimulation of bone healing by bone grafting or BMPs seem to be the best option. For femoral and tibial diaphyseal shaft fractures, dynamization of the nail is an atraumatic, effective, and cheap surgical possibility to achieve bony consolidation, particularly in delayed nonunions before 24 weeks after initial surgery. In established hypertrophic nonunions in the tibia and femur, biomechanical stability should be addressed by augmentation plating or exchange nailing. Hypotrophic or atrophic nonunions require additional biological stimulation of bone healing for augmentation plating.




Similar content being viewed by others
References
Weber BG, Cech O (1973) Pseudarthrosen. Pathophysiologie Biomechanik Therapie Ergebnisse. Huber, Bern
Frolke JP, Patka P (2007) Definition and classification of fracture non-unions. Injury 38(Suppl 2):S19–S22
Einhorn TA (1995) Enhancement of fracture-healing. J Bone Joint Surg Am 77:940–956
Mills LA, Aitken SA, Simpson AHR (2017) The risk of non-union per fracture: current myths and revised figures from a population of over 4 million adults. Acta Orthop 88:434-439. https://doi.org/10.1080/17453674.2017.1321351
Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R, Simpson H, Alt V (2014) Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury 45(Suppl 2):S3–S7. https://doi.org/10.1016/j.injury.2014.04.002
Mills LA, Simpson AH (2013) The relative incidence of fracture non-union in the Scottish population (5.17 million): a 5-year epidemiological study. BMJ Open. https://doi.org/10.1136/bmjopen-2012-002276
Nandra R, Grover L, Porter K (2015) Fracture non-union epidemiology and treatment. Trauma 18:3–11. https://doi.org/10.1177/1460408615591625
Peters RM, Claessen FM, Doornberg JN, Kolovich GP, Diercks RL, van den Bekerom MP (2015) Union rate after operative treatment of humeral shaft nonunion--a systematic review. Injury 46:2314–2324. https://doi.org/10.1016/j.injury.2015.09.041
Giannoudis P, MacDonald D, Matthews S, Smith R, Furlong A, De Boer P (2000) Nonunion of the femoral diaphysis. Bone Joint J 82:655–658
Canadian Orthopaedic Trauma S (2003) Nonunion following intramedullary nailing of the femur with and without reaming. Results of a multicenter randomized clinical trial. J Bone Joint Surg Am Vol 85-A:2093–2096
Investigators SPERINPTF (2008) Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. J Bone Joint Surg Am 90:2567
Vallier HA, Cureton BA, Patterson BM (2011) Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma 25:736–741. https://doi.org/10.1097/BOT.0b013e318213f709
Sanders R, Jersinovich I, Anglen J, DiPasquale T, Herscovici D Jr (1994) The treatment of open tibial shaft fractures using an interlocked intramedullary nail without reaming. J Orthop Trauma 8:504–510
Court-Brown CM (2004) Reamed intramedullary tibial nailing: an overview and analysis of 1106 cases. J Orthop Trauma 18:96–101
Antonova E, Le TK, Burge R, Mershon J (2013) Tibia shaft fractures: costly burden of nonunions. BMC Musculoskelet Disord 14:42
Khunda A, Al-Maiyah M, Eardley W, Montgomery R (2016) The management of tibial fracture non-union using the Taylor spatial frame. J Orthop 13:360–363
Cooper A (1842) A treatise on dislocations and fractures of the joints. Churchill, London
Bajada S, Marshall MJ, Wright KT, Richardson JB, Johnson WE (2009) Decreased osteogenesis, increased cell senescence and elevated Dickkopf-1 secretion in human fracture non union stromal cells. Bone 45:726–735. https://doi.org/10.1016/j.bone.2009.06.015
Iwakura T, Miwa M, Sakai Y, Niikura T, Lee SY, Oe K, Hasegawa T, Kuroda R, Fujioka H, Doita M (2009) Human hypertrophic nonunion tissue contains mesenchymal progenitor cells with multilineage capacity in vitro. J Orthop Res 27:208–215
Panteli M, Pountos I, Jones E, Giannoudis PV (2015) Biological and molecular profile of fracture non-union tissue: current insights. J Cell Mol Med 19:685–713
Reed A, Joyner C, Brownlow H, Simpson A (2002) Human atrophic fracture non-unions are not avascular. J Orthop Res 20:593–599
Hofmann A, Ritz U, Hessmann M, Schmid C, Tresch A, Rompe J, Meurer A, Rommens P (2008) Cell viability, osteoblast differentiation, and gene expression are altered in human osteoblasts from hypertrophic fracture non-unions. Bone 42:894–906
McDonald MM, Morse A, Mikulec K, Peacock L, Baldock PA, Kostenuik PJ, Little DG (2013) Matrix metalloproteinase–driven endochondral fracture union proceeds independently of osteoclast activity. J Bone Miner Res 28:1550–1560
Fajardo M, Liu C-J, Ilalov K, Egol KA (2010) Matrix metalloproteinases that associate with and cleave bone morphogenetic protein-2 in vitro are elevated in hypertrophic fracture nonunion tissue. J Orthop Trauma 24:557–563
Zeckey C, Hildebrand F, Glaubitz LM, Jürgens S, Ludwig T, Andruszkow H, Hüfner T, Krettek C, Stuhrmann M (2011) Are polymorphisms of molecules involved in bone healing correlated to aseptic femoral and tibial shaft non-unions? J Orthop Res 29:1724–1731
Xiong D-H, Liu X-G, Guo Y-F, Tan L-J, Wang L, Sha B-Y, Tang Z-H, Pan F, Yang T-L, Chen X-D (2009) Genome-wide association and follow-up replication studies identified ADAMTS18 and TGFBR3 as bone mass candidate genes in different ethnic groups. Am J Hum Genet 84:388–398
Claes L, Augat P, Suger G, Wilke HJ (1997) Influence of size and stability of the osteotomy gap on the success of fracture healing. J Orthop Res 15:577–584
Claes L, Grass R, Schmickal T, Kisse B, Eggers C, Gerngross H, Mutschler W, Arand M, Wintermeyer T, Wentzensen A (2002) Monitoring and healing analysis of 100 tibial shaft fractures. Langenbeck's Arch Surg 387:146–152
Gaebler C, Berger U, Schandelmaier P, Greitbauer M, Schauwecker HH, Applegate B, Zych G, Vecsei V (2001) Rates and odds ratios for complications in closed and open tibial fractures treated with unreamed, small diameter tibial nails: a multicenter analysis of 467 cases. J Orthop Trauma 15:415–423
Drosos G, Bishay M, Karnezis I, Alegakis A (2006) Factors affecting fracture healing after intramedullary nailing of the tibial diaphysis for closed and grade I open fractures. Bone Joint J 88:227–231
Schemitsch EH, Bhandari M, Guyatt G, Sanders DW, Swiontkowski M, Tornetta P, Walter SD, Zdero R, Goslings JC, Teague D, Jeray K, McKee MD, Study to Prospectively Evaluate Reamed Intramedullary Nails in Patients with Tibial Fractures I (2012) Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am 94:1786-1793. https://doi.org/10.2106/JBJS.J.01418
Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, Della Rocca GJ, Mehta S, McKinley T, Wang Z, Steen RG (2016) Epidemiology of fracture nonunion in 18 human bones. JAMA Surg 151:e162775. https://doi.org/10.1001/jamasurg.2016.2775
Giannoudis PV, Einhorn TA, Marsh D (2007) Fracture healing: the diamond concept. Injury 38:S3–S6
Klemm K, Schellmann W (1972) Dynamische und statische Verriegelung des Marknagels. Monatsschr Unfallheilkd 75:303
Egger EL, Gottsauner-Wolf F, Palmer J, Aro HT, Chao E (1993) Effects of axial dynamization on bone healing. J Trauma 34:185–192
Claes L, Wilke H, Augat P, Rübenacker S, Margevicius K (1995) Effect of dynamization on gap healing of diaphyseal fractures under external fixation. Clin Biomech 10:227–234
Kempf I, Grosse A, Beck G (1985) Closed locked intramedullary nailing. Its application to comminuted fractures of the femur. J Bone Joint Surg Am Vol 67:709–720
Foxworthy M, Pringle R (1995) Dynamization timing and its effect on bone healing when using the Orthofix dynamic axial Fixator. Injury 26:117–119
Glatt V, Evans CH, Tetsworth K (2016) A concert between biology and biomechanics: the influence of the mechanical environment on bone healing. Front Physiol 7:678. https://doi.org/10.3389/fphys.2016.00678
Pihlajamäki HK, Salminen ST, Böstman OM (2002) The treatment of nonunions following intramedullary nailing of femoral shaft fractures. J Orthop Trauma 16:394–402
Wu CC (1997) The effect of dynamization on slowing the healing of femur shaft fractures after interlocking nailing. J Trauma 43:263–267
Papakostidis C, Psyllakis I, Vardakas D, Grestas A, Giannoudis PV (2011) Femoral-shaft fractures and nonunions treated with intramedullary nails: the role of dynamisation. Injury 42:1353–1361
Vaughn J, Gotha H, Cohen E, Fantry AJ, Feller RJ, Van Meter J, Hayda R, Born CT (2016) Nail Dynamization for delayed union and nonunion in femur and tibia fractures. Orthopedics 39:e1117–e1123. https://doi.org/10.3928/01477447-20160819-01
Claes L, Blakytny R, Göckelmann M, Schoen M, Ignatius A, Willie B (2009) Early dynamization by reduced fixation stiffness does not improve fracture healing in a rat femoral osteotomy model. J Orthop Res 27:22–27
Claes L, Blakytny R, Besse J, Bausewein C, Ignatius A, Willie B (2011) Late dynamization by reduced fixation stiffness enhances fracture healing in a rat femoral osteotomy model. J Orthop Trauma 25:169–174
Huang KC, Tong KM, Lin YM, Loh el W, Hsu CE (2012) Evaluation of methods and timing in nail dynamisation for treating delayed healing femoral shaft fractures. Injury 43:1747-1752. https://doi.org/10.1016/j.injury.2012.06.024
Litrenta J, Tornetta P 3rd, Vallier H, Firoozabadi R, Leighton R, Egol K, Kruppa C, Jones CB, Collinge C, Bhandari M, Schemitsch E, Sanders D, Mullis B (2015) Dynamizations and exchanges: success rates and indications. J Orthop Trauma 29:569–573. https://doi.org/10.1097/BOT.0000000000000311
Ghiasi MS, Chen J, Vaziri A, Rodriguez EK, Nazarian A (2017) Bone fracture healing in mechanobiological modeling: a review of principles and methods. Bone reports 6:87–100. https://doi.org/10.1016/j.bonr.2017.03.002
Brinker MR, O'connor DP (2007) Exchange nailing of ununited fractures. The Journal of Bone & Joint Surgery 89:177–188
Wenisch S, Trinkaus K, Hild A, Hose D, Herde K, Heiss C, Kilian O, Alt V, Schnettler R (2005) Human reaming debris: a source of multipotent stem cells. Bone 36:74–83
Hoffmann S, Gerber C, von Oldenburg G, Kessler M, Stephan D, Augat P (2015) Effect of angular stability and other locking parameters on the mechanical performance of intramedullary nails. Biomed Tech (Berl) 60:157–164. https://doi.org/10.1515/bmt-2014-0100
Hierholzer C, Friederichs J, Glowalla C, Woltmann A, Buhren V, von Ruden C (2016) Reamed intramedullary exchange nailing in the operative treatment of aseptic tibial shaft nonunion. Int Orthop. https://doi.org/10.1007/s00264-016-3317-x
Abadie B, Leas D, Cannada L, Malm P, Morwood M, Howes C, Zura R, Healy K, Avery M, Schlatterer D (2016) Does screw configuration or fibular Osteotomy decrease healing time in exchange Tibial nailing? J Orthop Trauma 30:622–626
Shroeder JE, Mosheiff R, Khoury A, Liebergall M, Weil YA (2009) The outcome of closed, intramedullary exchange nailing with reamed insertion in the treatment of femoral shaft nonunions. J Orthop Trauma 23:653–657
Hak DJ, Lee SS, Goulet JA (2000) Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma 14:178–182
Tsang ST, Mills LA, Frantzias J, Baren JP, Keating JF, Simpson AH (2016) Exchange nailing for nonunion of diaphyseal fractures of the tibia: our results and an analysis of the risk factors for failure. Bone Joint J 98-B:534–541. https://doi.org/10.1302/0301-620X.98B4.34870
Lin J, Chiang H, Hou S-M (2003) Open exchange locked nailing in humeral nonunions after intramedullary nailing. Clin Orthop Relat Res 411:260–268
McKee MD, Miranda MA, Riemer BL, Blasier RB, Redmond BJ, Sims SH, Waddell JP, Jupiter JB (1996) Management of humeral nonunion after the failure of locking intramedullary nails. J Orthop Trauma 10:492–499
Flinkkilä T, Ristiniemi J, Hämäläinen M (2001) Nonunion after intramedullary nailing of humeral shaft fractures. J Trauma Acute Care Surg 50:540–544
Sen MK, Miclau T (2007) Autologous iliac crest bone graft: should it still be the gold standard for treating nonunions? Injury 38(Suppl 1):S75–S80. https://doi.org/10.1016/j.injury.2007.02.012
Megas P (2005) Classification of non-union. Injury 36(Suppl 4):S30–S37. https://doi.org/10.1016/j.injury.2005.10.008
Dekker TJ, White P, Adams SB (2016) Efficacy of a cellular bone allograft for foot and ankle arthrodesis and revision nonunion procedures. Foot Ankle Int 1071100716674977
Dawson J, Kiner D, Warren Gardner I, Swafford R, Nowotarski PJ (2014) The reamer–irrigator–aspirator as a device for harvesting bone graft compared with iliac crest bone graft: union rates and complications. J Orthop Trauma 28:584–590
Khan SN, Cammisa FP Jr, Sandhu HS, Diwan AD, Girardi FP, Lane JM (2005) The biology of bone grafting. J Am Acad Orthopaed Surg 13:77–86
Griffin KS, Davis KM, McKinley TO, Anglen JO, Chu T-MG, Boerckel JD, Kacena MA (2015) Evolution of bone grafting: bone grafts and tissue engineering strategies for vascularized bone regeneration. Clin Rev Bone Mineral Metab 13:232–244
Cox G, Jones E, McGonagle D, Giannoudis PV (2011) Reamer-irrigator-aspirator indications and clinical results: a systematic review. Int Orthop 35:951–956
Calori G, Colombo M, Mazza E, Mazzola S, Malagoli E, Mineo G (2014) Incidence of donor site morbidity following harvesting from iliac crest or RIA graft. Injury 45:S116–S120
Emara KM, Diab RA, Emara AK (2015) Recent biological trends in management of fracture non-union. World J Orthoped 6:623
Tomford WW (2000) Bone allografts: past, present and future. Cell Tissue Bank 1:105–109
Roberts TT, Rosenbaum AJ (2012) Bone grafts, bone substitutes and orthobiologics: the bridge between basic science and clinical advancements in fracture healing. Organ 8:114–124
Sutherland A, Raafat A, Yates P, Hutchison J (1997) Infection associated with the use of allograft bone from the north east Scotland bone Bank. J Hosp Infect 35:215–222
Liu J, Chao L, Su L, Wang J, Wang C (2002) Experience with a bone bank operation and allograft bone infection in recipients at a medical centre in southern Taiwan. J Hosp Infect 50:293–297
Wozney JM, Rosen V, Celeste AJ, Mitsock LM, Whitters MJ, Kriz RW, Hewick RM, Wang EA (1988) Novel regulators of bone formation: molecular clones and activities. Science 242:1528–1535
Urist MR (1965) Bone: formation by autoinduction. Science 150:893–899
Garrison KR, Shemilt I, Donell S, Ryder JJ, Mugford M, Harvey I, Song F, Alt V (2010) Bone morphogenetic protein (BMP) for fracture healing in adults. Cochrane Database Syst Rev 16:CD006950. https://doi.org/10.1002/14651858.CD006950.pub2
Miska M, Findeisen S, Tanner M, Biglari B, Studier-Fischer S, Grützner P, Schmidmaier G, Moghaddam A (2016) Treatment of nonunions in fractures of the humeral shaft according to the diamond concept. Bone Joint J 98:81–87
Singh R, Bleibleh S, Kanakaris NK, Giannoudis PV (2016) Upper limb non-unions treated with BMP-7: efficacy and clinical results. Injury 47:S33–S39
Pneumaticos SG, Panteli M, Triantafyllopoulos GK, Papakostidis C, Giannoudis PV (2014) Management and outcome of diaphyseal aseptic non-unions of the lower limb: a systematic review. The surgeon 12:166–175
Alt V, Meyer C, Litzlbauer HD, Schnettler R (2007) Treatment of a double nonunion of the femur by rhBMP-2. J Orthop Trauma 21:734–737
Schell H, Duda G, Peters A, Tsitsilonis S, Johnson K, Schmidt-Bleek K (2017) The haematoma and its role in bone healing. J Experiment Orthopaed 4:5
Seebach C, Henrich D, Tewksbury R, Wilhelm K, Marzi I (2007) Number and proliferative capacity of human mesenchymal stem cells are modulated positively in multiple trauma patients and negatively in atrophic nonunions. Calcif Tissue Int 80:294–300
Mathieu M, Rigutto S, Ingels A, Spruyt D, Stricwant N, Kharroubi I, Albarani V, Jayankura M, Rasschaert J, Bastianelli E (2013) Decreased pool of mesenchymal stem cells is associated with altered chemokines serum levels in atrophic nonunion fractures. Bone 53:391–398
Goujon E (1869) Recherches expérimentales sur les propriétés du tissu osseux. JL Anat 6:399–412
Friedenstein AJ, Petrakova KV, Kurolesova AI, Frolova GP (1968) HETEROTOPIC transplants of bone marrow. Transplantation 6:230–247
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Paley D, Young MC, Wiley AM, Fornasier VL, Jackson RW (1986) Percutaneous bone marrow grafting of fractures and bony defects an experimental study in rabbits. Clin Orthop Relat Res 208:300
Connolly JF, Guse R, Tiedeman J, Dehne R (1991) Autologous marrow injection as a substitute for operative grafting of tibial nonunions. Clin Orthop Relat Res 266:259–270
Bruder SP, Kurth AA, Shea M, Hayes WC, Jaiswal N, Kadiyala S (1998) Bone regeneration by implantation of purified, culture-expanded human mesenchymal stem cells. J Orthop Res 16:155–162
Homma Y, Zimmermann G, Hernigou P (2013) Cellular therapies for the treatment of non-union: the past, present and future. Injury 44:S46–S49
Bajada S, Harrison P, Ashton B, Cassar-Pullicino V, Ashammakhi N, Richardson J (2007) Successful treatment of refractory tibial nonunion using calcium sulphate and bone marrow stromal cell implantation. Bone Joint J 89:1382–1386
Hernigou P, Poignard A, Beaujean F, Rouard H (2005) Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am vol 87:1430–1437. https://doi.org/10.2106/JBJS.D.02215
Quarto R, Mastrogiacomo M, Cancedda R, Kutepov SM, Mukhachev V, Lavroukov A, Kon E, Marcacci M (2001) Repair of large bone defects with the use of autologous bone marrow stromal cells. N Engl J Med 344:385–386
Wittig O, Romano E, Gonzalez C, Diaz-Solano D, Marquez ME, Tovar P, Aoun R, Cardier JE (2016) A method of treatment for nonunion after fractures using mesenchymal stromal cells loaded on collagen microspheres and incorporated into platelet-rich plasma clots. Int Orthop 40:1033–1038. https://doi.org/10.1007/s00264-016-3130-6
Kazmers NH, Fragomen AT, Rozbruch SR (2016) Prevention of pin site infection in external fixation: a review of the literature. Strategies Trauma Limb Reconstr 11:75–85
Kadhim M, Holmes L Jr, Gesheff MG, Conway JD (2017) Treatment options for nonunion with segmental bone defects: systematic review and quantitative evidence synthesis. J Orthop Trauma 31:111–119. https://doi.org/10.1097/BOT.0000000000000700
Harshwal RK, Sankhala SS, Jalan D (2014) Management of nonunion of lower-extremity long bones using mono-lateral external fixator–report of 37 cases. Injury 45:560–567
Brinker MR, O'Connor DP (2003) Ilizarov compression over a nail for aseptic femoral nonunions that have failed exchange nailing: a report of five cases. J Orthop Trauma 17:668–676
El-Rosasy MA (2012) Nonunited humerus shaft fractures treated by external fixator augmented by intramedullary rod. Indian J Orthopaed 46:58
Ilizarov G, Lediaev V (1969) Replacement of defects of long tubular bones by means of one of their fragments. Vestnik khirurgii imeni II Grekova 102:77
Ilizarov GA (1989) The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthopaed Relat Res 239:263–285
Green SA (1994) Skeletal defects a comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res 301:111–117
Oh CW, Apivatthakakul T, Oh JK, Kim JW, Lee HJ, Kyung HS, Baek SG, Jung GH (2013) Bone transport with an external fixator and a locking plate for segmental tibial defects. The bone & joint journal 95-B:1667–1672. https://doi.org/10.1302/0301-620X.95B12.31507
Kadhim M, Holmes L Jr, Gesheff MG, Conway JD (2017) Treatment options for nonunion with segmental bone defects: systematic review and quantitative evidence synthesis. J Orthop Trauma 31:111–119
Ueng SW, Chao E-K, Lee S-S, Shih C-H (1997) Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma Acute Care Surg 43:640–644
Wang Z, Liu C, Liu C, Zhou Q, Liu J (2014) Effectiveness of exchange nailing and augmentation plating for femoral shaft nonunion after nailing. Int Orthop 38:2343–2347
Park J, Kim SG, Yoon HK, Yang KH (2010) The treatment of nonisthmal femoral shaft nonunions with im nail exchange versus augmentation plating. J Orthop Trauma 24:89–94
Birjandinejad A, Ebrahimzadeh MH, Ahmadzadeh-Chabock H (2009) Augmentation plate fixation for the treatment of femoral and tibial nonunion after intramedullary nailing. Orthopedics 32:409. https://doi.org/10.3928/01477447-20090511-12
Ateschrang A, Albrecht D, Stockle U, Weise K, Stuby F, Zieker D (2013) High success rate for augmentation compression plating leaving the nail in situ for aseptic diaphyseal tibial nonunions. J Orthop Trauma 27:145–149. https://doi.org/10.1097/BOT.0b013e31825d01b2
Gessmann J, Königshausen M, Coulibaly MO, Schildhauer TA, Seybold D (2016) Anterior augmentation plating of aseptic humeral shaft nonunions after intramedullary nailing. Arch Orthop Trauma Surg 136:631–638
Hierholzer C, Sama D, Toro JB, Peterson M, Helfet DL (2006) Plate fixation of ununited humeral shaft fractures: effect of type of bone graft on healing. J Bone Joint Surg Am 88:1442–1447. https://doi.org/10.2106/JBJS.E.00332
Huang K-C, Tong K-M, Lin Y-M, Loh E-W, Hsu C-E (2012) Evaluation of methods and timing in nail dynamisation for treating delayed healing femoral shaft fractures. Injury 43:1747–1752
Lin CJ, Chiang CC, Wu PK, Chen CF, Huang CK, Su AW, Chen WM, Liu CL, Chen TH (2012) Effectiveness of plate augmentation for femoral shaft nonunion after nailing. J Chin Med Association 75:396–401. https://doi.org/10.1016/j.jcma.2012.06.008
Choi Y, Kim K (2005) Plate augmentation leaving the nail in situ and bone grafting for non-union of femoral shaft fractures. Int Orthop 29:287–290
Feldman DS, Shin SS, Madan S, Koval KJ (2003) Correction of tibial malunion and nonunion with six-axis analysis deformity correction using the Taylor spatial frame. J Orthop Trauma 17:549–554
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rupp, M., Biehl, C., Budak, M. et al. Diaphyseal long bone nonunions — types, aetiology, economics, and treatment recommendations. International Orthopaedics (SICOT) 42, 247–258 (2018). https://doi.org/10.1007/s00264-017-3734-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3734-5