Abstract
Purpose
To quantify the influence of ALL lesions on static and dynamic laxity in ACL-deficient knee.
Methods
The study was performed in 10 fresh-frozen knees. The joints were analysed in the following conditions: intact, ACL resection and ACL + ALL resection. Testing parameters were defined as: anterior displacement at 30° and 90° of flexion (AP30, AP90) applying a manual-maximum load; internal rotation at 30° and 90° of flexion (INT30, INT90) applying a 5 N m torque and internal rotation and acceleration during manual pivot-shift (PS) test. Kinematics was acquired by a navigation system; a testing rig and a torquemeter were used to control the limb position and the applied torque. Paired Student’s t test was conducted to assess statistical difference, and significance was set at P < 0.05.
Results
The ALL resection determined a significant increase in terms of internal rotation (INT30 P = 0.02, INT90 P = 0.03), while AP30 (P n.s) and AP90 (P n.s) were not affected. ALL resection produced a significant increase in terms of acceleration during PS test (P < 0.01), but no significant change in PS internal rotation was observed.
Conclusion
The ALL plays a significant role in controlling static internal rotation and acceleration during PS test. On the other hand, ALL resection did not produce any significant change in terms of anterior displacement. A trend was seen for the internal rotation during the pivot-shift test to increase after ALL resection was higher when compared to the intact and isolated ACL lesion states; however, the differences were not significant. The results highlight the clinical relevance of this structure that should be assessed before an ACL reconstruction in order to avoid residual laxity.
Similar content being viewed by others
Introduction
According to the current literature, the importance of the secondary restraint of the knee as a key factor in the ACL reconstruction failure has been emphasized [12, 17, 19]. The function of the majority of the stabilizing soft tissues of the knee joint has been widely investigated. However, the anatomy and function of the anterolateral structures of the knee have been poorly understood. In the 1879, Ségond [25] first described a “pearly, resistant, fibrous band” associated with the avulsion fracture now named as the “Ségond fracture”. Other previous studies have used different terminology to allude to this structure of the knee: “Anterior oblique band”, “Capsulo-osseous layer of iliotibial tract”, “Lateral capsular ligament” and “Mid-third lateral capsular ligament” [5, 10, 13, 15, 24].
Due to the complex relationships among the structures of the anterolateral aspect of the knee, there are few discrepancies in the anatomical description of this structure in the anterolateral aspect of the knee now termed anterolateral ligament (ALL). Claes et al. [3] described a ligamentous structure connecting the femur with the tibia with connections to the lateral meniscus. They identified the femoral attachment over the epicondyle slightly anterior to the attachment of the lateral collateral ligament (LCL). Dodds et al. [6] identified an extracapsular structure without any connection with the lateral meniscus and with a femoral attachment described as being proximal and posterior to the epicondyle. However, it has been clearly defined that the ALL is a distinct ligamentous structure with an incidence ranging from 83 % [6] to 100 % [24].
Given the recent improvements in understanding the anatomy and incidence of the ALL, the kinematic role of this ligament and its clinical relevance have yet to be fully determined. It has been suggested that the ALL acts as secondary restrain to control rotational laxity [6, 13, 27, 28]. Further, it has been hypothesized to be associated with the “Segond fracture” that is considered to be pathognomonic for ACL injury. However, in the current literature, there is a paucity of biomechanical data focused on the effect of an ALL tear in an ACL-deficient knee.
Therefore, the aim of this study is to investigate in vitro the effect of an ALL tear on the static and dynamic laxity parameters of an ACL-deficient knee. Moreover, in order to perform an evaluation reproducible in vivo, a navigation system was used to assess the laxity parameters.
The hypothesis was that a lesion of the ALL in ACL-deficient knee would produce significant alterations in the kinematic of the knee joint. In particular, it has been hypothesized an increase in both dynamic and static laxity levels with particular attention to the rotational contribution.
Materials and methods
Ten (5 matched pairs) fresh-frozen cadaveric specimens were used in the study (mean age 79 ± 5 years old). Only joints without evidence of prior knee injury, surgery, arthritis or anatomical abnormality were included in the present work. Cadaveric specimens were stored at −20 °C and thawed at least 36 h before use.
Skin and subcutaneous fat were removed 15 cm from the joint line on tibia as well as on femur. The ligamentous and the tendinous structures were left intact. The iliotibial band was incised along its fibres in order to identify the ALL. After separating the fibres of the iliotibial tract, a manual internal torque was applied and tense fibres were identified. Those fibres were running obliquely over the lateral collateral ligament (LCL) until their fanlike insertion on the tibia proximally and posterior to the Gerdy’s tubercle. Those fibres were isolated from the capsule and were indentified as the ALL (Fig. 1). A medial parapatellar arthrotomy was performed to assess the status of knee joint to access the ACL.
After the preparation of the limb, a 3-mm bicortical pin was inserted into the diaphyseal area of both femur and tibia. Then, a tracker-holding device was attached to the pins in order to set-up the navigation system (Polaris, NDI, Waterloo, Ontario, Canada) embedded with a custom-made software (MATLAB, The MathWorks Inc., Natick, Massachusetts, USA). An anatomical femoral and tibial coordinate system was defined for each joint using a tracked probe to select palpable anatomical landmarks. In particular, the femoral system of reference needs the acquisition of the medial and lateral epicondyles and the definition through a pivoting motion of hip joint centre. For the tibial anatomical reference system are required the medial and lateral malleolus and the most medial as well as the most lateral point of the tibial plateau. The foot was fastened to a testing rig in order to maintain the correct limb position during the kinematic testing.
Biomechanical testing
A single surgeon, experienced with navigation system, performed the ligament sectioning and the entire kinematics evaluation. The specimens were tested in the following conditions: (1) intact knee, (2) resection of the ACL (ACL) and (3) resection of the ALL (ACL + ALL).
All the testing conditions were subjected to a manual-maximum anterior tibial load at 30° and 90° of knee flexion, and 5 N m internal rotation torque was applied at 30° and 90° of flexion. The selected flexion angles were based on the commonly performed clinical test (i.e. Lachman and Drawer test) as well as on the available scientific manuscripts [2, 7, 8, 29]. Anterior–posterior test at 30° and 90° of knee joint flexion (AP30, AP90), internal rotation test at 30° and 90° of flexion (INT30, INT90) and pivot-shift (PS) test were performed. In order to quantify static laxity level, the tibial displacement has been evaluated, with respect to femoral system of reference, in anterior–posterior direction during AP30 and AP90. Moreover, the internal rotation of the tibial system of reference versus the femoral one during INT30 and INT90 test was assessed.
Pivot-shift test was executed following the procedure reported by Galway and MacIntosh [9] and Jakob [14]. The laxity parameters evaluated during PS test were the acceleration displacement of the lateral tibial compartment as well as the internal rotation. Lateral compartment has been reported being the one mainly affected by the PS phenomenon [1]. The motion in the described anatomical coordinate systems was evaluated according to the Grood and Suntay algorithm [11]. Between the testing of each knee state, the joint was maintained damp applying saline. All the kinematics data were elaborated offline with a MATLAB (The MathWorks Inc, Natick, Massachusetts, USA) interface specifically developed. The 3D root-mean-square (RMS) volumetric accuracy of the navigation system in the localization of a single passive marker declared by manufacturer is equal to 0.35 mm [32]. According to this, all the results were rounded to the first decimal digit. Reliability of the performed tests has been determined in a previous in vivo study where the joints were tested at manual-maximum force. For AP30/AP90, it has been found an intra-tester repeatability of about 1 mm, while for rotational test, it was 1° [30]. Also, the repeatability of the pivot-shift test manually performed has been deeply analysed in a previous in vivo navigated study [20] underling encouraging value. To control the 5 N m torque load applied for the execution of rotational test, an analogical torquemeter (Stryker Howmedica Dall Miles Instruments, Limbach-Oberfrohna, Germany; full scale 20 N m/180 lb-In) arranged to the testing rig was used.
All the biomechanical tests have been performed at Laboratoire d’Anatomie, Universitè Françoise-Rabelais. IRB approval was not required.
Statistical analysis
Based on an alpha level of 0.05, ten specimens were found to be sufficient to detect a significant difference among the tested conditions with 80 % of power.
Normality of the acquired data has been evaluated by Kolmogorov–Smirnov test. Paired Student’s t tests were used to analyse differences in laxity between intact, ACL-deficient and ACL + ALL-deficient states after each performed test (anterior–posterior displacement, internal rotation and pivot-shift test). All statistical analysis was performed using MATLAB (The MathWorks Inc., Natick, Massachusetts, USA). For all comparisons, significance was set at P = 0.05.
Results
Kolmogorov–Smirnov test confirmed the normal distribution of the data for all the acquired data.
Anterior–posterior displacement at 30° and 90° of knee flexion (AP30, AP90)
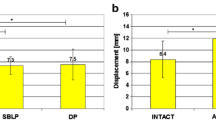
While tested under manual-maximum load, the ACL-deficient condition had significantly higher (P < 0.01) anterior–posterior displacement at 30° of knee flexion compared to the intact state. When even the ALL was resected and the two states ACL-deficient knee and ACL + ALL-deficient knee were compared, no further significant increase in laxity was found (n.s).
Analogously, at 90° of knee flexion, both the ACL− and ACL + ALL-deficient knee state had significantly increased average anterior–posterior translation when compared with the intact condition (P = 0.03 and P < 0.01, respectively). There were no significant differences (n.s) between ACL− and ACL + ALL-deficient knee state (Fig. 2a, b).
Mean (SD) values of anterior tibial translation (mm) at 30° (a) and 90° (b) of flexion for INTACT, ACL deficient and ACL + ALL-deficient joints status. Tests have been manually performed at the manual-maximum force. Statistically significant (P < 0.05) differences have been underlined by asterisks sign
Considering the absolute value of anterior–posterior displacement, the highest mean value was still found at 30° of flexion after ACL + ALL resection. Anyway, difference between absolute value of AP30 and AP90 for the ACL + ALL-deficient knee condition was not statistically significant (n.s).
Internal rotation at 30° and 90° of knee flexion (IE30, IE90)
The ACL + ALL state had significantly (P = 0.02) more internal–external rotation when compared with the isolated ACL-sectioned state under a 5 N m internal rotation torque. Analogously, at 90° of flexion, the ACL + ALL-deficient knee condition displayed significant increase in internal rotation when compared to the ACL-deficient state (P = 0.03). No other significant differences were found for other comparisons with the cutting conditions (Fig. 3a, b).
Mean (SD) values of tibial internal rotation (°) at 30° (a) and 90° (b) of flexion for INTACT, ACL deficient and ACL + ALL-deficient knees status. Tests have been manually performed applying a 5 N m torque load controlled by a analogical torquemeter (Stryker Howmedica Dall Miles Instruments, Limbach-Oberfrohna, Germany). Statistically significant (P < 0.05) differences have been underlined by asterisks sign
Considering the absolute value of internal rotation, the highest mean value was obtained at 90° of flexion after ACL + ALL resection. INT90 for the ACL + ALL-deficient knee condition was significantly higher than INT30 for the same state (P = 0.04).
Pivot-shift test: acceleration and internal rotation
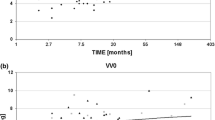
The cutting of the ACL showed no significant differences in acceleration compared with the intact state. The ACL + ALL-deficient knee condition had significantly more acceleration (P < 0.01) than the intact state during pivot-shift state. Considering the internal rotation during pivot-shift test, no significant differences have been found when comparing the intact, ACL-deficient and ACL + ALL-deficient knee (Fig. 4a, b).
Discussion
The most important finding of the current study was that ALL has a specific biomechanical role as it significantly restrains static internal rotation in an ACL-deficient knee. On the other hand, ALL resection did not produce any significant change in terms of anterior displacement. Further, an ALL tear produced a significant increase in terms of acceleration during PS test. A trend was seen for the internal rotation during the pivot-shift test to increase after ALL resection as this laxity parameter is increased of almost 10° (Fig. 4b). This increase was higher than the one produced during the static internal rotation, but it was not significant.
In the 70s, Hughston et al. [13], in a dissection biomechanical study of the lateral compartment of the knee, identified the ‘‘midthird capsular ligament’’ as key restrain against the occurrence of anterolateral rotatory instability. In a recent paper [6], the ALL was described as an isometric structure from 0° to 60° of knee flexion. They observed an increase in the ligament length with an internal tibial rotation from 30° to 90° of flexion. Claes et al. [3] observed this structure to be tensioned by coupled flexion and internal rotation; however, they did not quantify the kinematic function of the ALL.
In an in vitro set-up similar to the current study, Monaco et al. [21] performed a cutting study of the two bundles of the ACL and the anterolateral aspect of the knee. The resection of the anterolateral aspect of the knee produced a significant increase in the internal rotation at 30° of flexion. These authors noticed that the anterior tibial displacement was significantly increased by the anterolateral resection. In the current paper, this laxity parameter was not affected by the ALL status. A reason for this difference might be in the cutting procedure as they did not isolate the ALL from the capsule, but they performed a wide resection 2 cm long through all the structures of the third layer of the anterolateral aspect of the knee [13]. Further, they reported high correlation among the anterolateral resection and the pivot-shift phenomenon, which was clinically evaluated. In the current paper, a significant difference was observed concerning the acceleration during the pivot shift, which as been demonstrated to be a parameter that correlate with clinical grade of pivot shift [18]. Interestingly, the isolated lesion of the ACL did not significantly affect the acceleration; this finding might suggest that when a significant pivot shift is noted in clinical practice, a possible unrecognized lesion to the anterolateral aspect of the knee might occur.
Recently, Spencer et al. [26] assessed the biomechanical function of the ALL from lesion to reconstruction. In their cutting study, the ALL resulted to be effective in controlling internal rotation in the setting of a combined complete ACL tear during the early phase of simulated pivot shift. In the current paper, the influence of the ALL on the internal rotation during pivot shift was not significant; however, a trend was seen for this laxity parameter to increase after ALL resection. The authors believe that this lack of significance might be due to the size of the series and due to the complexity of the pivot-shift phenomenon which is affected from anatomical features and other stabilizing structures [22]. Consistently to the current paper, they observed that sectioning the ALL did not produced any significant increase in terms of anterior translation compared to an isolated ACL tear. In another biomechanical study [23], the ACL, the ALL and the lateral collateral ligament (LCL) were randomly sectioned achieving similar findings. Concerning anterior translation, they reported significant changes produced by the ACL but not by the ALL. During internal rotation, both ligaments resulted to be significant restrains. Interestingly, they noticed that the ALL contribution increased with the knee flexion, while the ACL contribution followed an opposite trend. In the current paper, absolute value of internal rotation with both ligaments resected was higher at deeper angle of flexion. However, these findings are difficult to compare as avoiding randomization precludes the possibility to evaluate the function of each ligament at different angles of flexion. On the other hand, a recent paper reported the superficial and deep layers of the iliotibial tract to be the primary restraint to tibial internal rotation between 30° and 90° of flexion and 30°–45° during a simulated pivot shift, while the ALL was just a minor restraint [16]. These results were criticized by an international group of experts [4] postulating that deep layer of the iliotibial tract and the ALL of the knee are basically the same structure but isolated with different procedures. The authors of the current paper agree with this last point of view as no distinct structure other than the ALL was identified during the dissection between the capsule and the iliotibial tract.
The authors noted some limitations. First, the cohort size was limited, and the age of the cadavers was not similar to a normal ACL injury population. Second, the cutting sequence was not randomized; however, varying the order of ligament sectioning would not have been consistent with the aim to investigate the effect of an ALL tear on an ACL-deficient knee. Third, the kinematic evaluation was performed by means of a navigation system in place of a robot testing system. The robot is capable of higher kinematic measurement [31]; however, the navigation system allowed for an experimental set-up is closer to the in vivo one. Therefore, the authors believe that the result of the current paper can be more directly applied to the everyday clinical practice.
Conclusion
In conclusion, this study shows that ALL plays a significant role in controlling static internal rotation and pivot shift in the setting of an ACL-deficient knee. These findings highlight the importance of ALL as secondary restraint of the knee. The authors recommend evaluation of the anterolateral aspect of the knee when facing an ACL reconstruction in everyday clinical practice in the attempt to prevent residual rotational laxity.
References
Bedi A, Musahl V, Lane C, Citak M, Warren RF, Pearle AD (2010) Lateral compartment translation predicts the grade of pivot shift: a cadaveric and clinical analysis. Knee Surg Sports Traumatol Arthrosc 18(9):1269–1276
Bonanzinga T, Signorelli C, Lopomo N, Grassi A, Neri MP, Filardo G, Zaffagnini S, Marcacci M (2015) Biomechanical effect of posterolateral corner sectioning after ACL injury and reconstruction. Knee Surg Sports Traumatol Arthrosc 23(10):2918–2924
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223(4):321–328
Daggett M, Claes S, Helito CP, Imbert P, Monaco E, Lutz C, Sonnery-Cottet B (2016) The Role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee: letter to the editor. Am J Sports Med 44(4):NP14–NP15
Dietz GW, Wilcox DM, Montgomery JB (1986) Segond tibial condyle fracture: lateral capsular ligament avulsion. Radiology 159(2):467–469
Dodds AL, Gupte CM, Neyret P, Williams AM, Amis AA (2011) Extra-articular techniques in anterior cruciate ligament reconstruction: a literature review. J Bone Joint Surg Br 93(11):1440–1448
Driscoll MD, Isabell GP, Conditt MA, Ismaily SK, Jupiter DC, Noble PC, Lowe WR (2012) Comparison of 2 femoral tunnel locations in anatomic single-bundle anterior cruciate ligament reconstruction: a biomechanical study. Arthroscopy 28(10):1481–1489
Gadikota HR, Seon JK, Kozanek M, Oh LS, Gill TJ, Montgomery KD, Li G (2009) Biomechanical comparison of single-tunnel-double-bundle and single-bundle anterior cruciate ligament reconstructions. Am J Sports Med 37(5):962–969
Galway HR, MacIntosh DL (1980) The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 147:45–50
Goldman AB, Pavlov H, Rubenstein D (1988) The segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. AJR Am J Roentgenol 151(6):1163–1167
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105(2):136–144
Hara K, Niga S, Ikeda H, Cho S, Muneta T (2008) Isolated anterior cruciate ligament reconstruction in patients with chronic anterior cruciate ligament insufficiency combined with grade II valgus laxity. Am J Sports Med 36(2):333–339
Hughston JC, Andrews JR, Cross MJ, Moschi A (1976) Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am 58(2):173–179
Jakob RP, Stäubli HU, Deland JT (1987) Grading the pivot shift. Objective tests with implications for treatment. J Bone Joint Surg Br 69(2):294–299
Johnson LL (1979) Lateral capsualr ligament complex: anatomical and surgical considerations. Am J Sports Med 7(3):156–160
Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, Amis AA (2016) The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med 44(2):345–354
Kopf S, Kauert R, Halfpaap J, Jung T, Becker R (2012) A new quantitative method for pivot shift grading. Knee Surg Sports Traumatol Arthrosc 20(4):718–723
Labbe DR, de Guise JA, Mezghani N, Godbout V, Grimard G, Baillargeon D, Lavigne P, Fernandes J, Ranger P, Hagemeister N (2010) Feature selection using a principal component analysis of the kinematics of the pivot shift phenomenon. J Biomech 43(12):3080–3084
Lopomo N, Signorelli C, Bonanzinga T, Marcheggiani Muccioli GM, Visani A, Zaffagnini S (2012) Quantitative assessment of pivot-shift using inertial sensors. Knee Surg Sports Traumatol Arthrosc 20(4):713–717
Lopomo N, Zaffagnini S, Bignozzi S, Visani A, Marcacci M (2010) Pivot-shift test: analysis and quantification of knee laxity parameters using a navigation system. J Orthop Res 28(2):164–169
Monaco E, Ferretti A, Labianca L, Maestri B, Speranza A, Kelly MJ, D’Arrigo C (2012) Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc 20(5):870–877
Musahl V, Ayeni OR, Citak M, Irrgang JJ, Pearle AD, Wickiewicz TL (2010) The influence of bony morphology on the magnitude of the pivot shift. Knee Surg Sports Traumatol Arthrosc 18(9):1232–1238
Parsons EM, Gee AO, Spiekerman C, Cavanagh PR (2015) The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 43(3):669–674
Pomajzl R, Maerz T, Shams C, Guettler J, Bicos J (2015) A review of the anterolateral ligament of the knee: current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy 31(3):583–591
Segond P (1879) Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Prog Med 7:297–341
Spencer L, Burkhart TA, Tran MN, Rezansoff AJ, Deo S, Caterine S, Getgood AM (2015) Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med 43(9):2189–2197
Vieira EL, Vieira EA, da Silva RT, dos Santos Berlfein PA, Abdalla RJ, Cohen M (2007) An anatomic study of the iliotibial tract. Arthroscopy 23(3):269–274
Vincent JP, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F, Al-Saati MF, Lustig S, Demey G, Servien E, Neyret P (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20(1):147–152
Wang JH, Kato Y, Ingham SJM, Maeyama A, Linde-Rosen M, Smolinski P, Fu FH (2012) Measurement of the end-to-end distances between the femoral and tibial insertion sites of the anterior cruciate ligament during knee flexion and with rotational torque. Arthroscopy 28(10):1524–1532
Zaffagnini S, Bignozzi S, Martelli S, Imakiire N, Lopomo N, Marcacci M (2006) New intraoperative protocol for kinematic evaluation of ACL reconstruction: preliminary results. Knee Surg Sports Traumatol Arthrosc 14(9):811–816
Zantop T, Schumacher T, Diermann N, Schanz S, Raschke MJ, Petersen W (2007) Anterolateral rotational knee instability: role of posterolateral structures. Winner of the AGA-DonJoy Award 2006. Arch Orthop Trauma Surg 127(9):743–752
http://www.ndigital.com/medical/polarisfamily-techspecs.php. Date Disp. August 5th 2015
Acknowledgments
This work was supported by Italian Ministry of Health, Progetto RF Ministero Salute [grant number 2010-2312173].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work was supported by Italian Ministry of Health, Progetto RF Ministero Salute [grant number 2010-2312173].
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Bonanzinga, T., Signorelli, C., Grassi, A. et al. Kinematics of ACL and anterolateral ligament. Part I: Combined lesion. Knee Surg Sports Traumatol Arthrosc 25, 1055–1061 (2017). https://doi.org/10.1007/s00167-016-4259-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4259-y