Abstract
Objective
To develop a risk stratification scheme for deliberate self-extubation in intensive care patients.
Design
A nested case-control study.
Setting
Four surgical ICUs, one medical ICU, one coronary care unit, and one emergency department of a tertiary care center.
Measurement
In a 3-month period, the number of ventilation periods, ventilation days, and unplanned extubations were recorded. Potential determinants of unplanned extubation were assessed with a translated (English to Dutch) and modified version of the “Unplanned Extubation Data Collection Tool.”
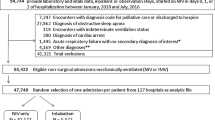
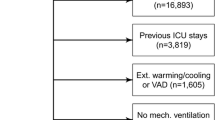
Patients
Clinical and demographic characteristics and circumstances of the 26 unplanned extubations were compared with those of 48 randomly selected control patients who did not experience unplanned extubation.
Results
The incidence of unplanned extubation was 4.2%, corresponding to 0.68 unplanned extubations per 100 ventilation days. The incidence was substantially lower at surgical ICUs (2.6%) compared with that at medical ICU/CCUs (9.5%). Multiple logistic regression analysis revealed that patients with a low sedation level (Bloomsbury Sedation Score) and a higher degree of consciousness (Glasgow Coma Scale) were at higher risk for deliberate self-extubation. The explained variance of this model including these factors was 67.3%.
Conclusion
Based on the risk factors identified, a risk assessment tool was developed. Systematic administration of the Bloomsbury Sedation Score and the Glasgow Coma Scale, and the use of the stratification scheme, allows identification of patients at risk. Appropriate reduction of sedative drugs during weaning, a timely extubation, and increased surveillance in patients identified to be at risk are possible interventions to diminish the number of unplanned extubations.

Similar content being viewed by others
References
Epstein SK, Nevins ML, Chung J (2000) Effect of unplanned extubation on outcome of mechanical ventilation. Am J Respir Crit Care Med 161:1912–1916
Chevron V, Menard JF, Richard JC, Girault C, Leroy J, Bonmarchand G (1998) Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med 26:1049–1053
Betbese AJ, Perez M, Bak E, Rialp G, Mancebo J (1998) A prospective study of unplanned endotracheal extubation in intensive care unit patients. Crit Care Med 26:1180–1186
Tindol GA Jr, Benedetto RJ Di, Kosciuk L (1994) Unplanned extubations. Chest 105:1804–1807
Ellstrom K, Brenner M, Williams J (1991) Incidence and factors related to unplanned extubations in the MICU (Abstract). Heart Lung 20:23A
Atkins PM, Mion LC, Mendelson W, Palmer RM, Slomka J, Franko T (1997) Characteristics and outcomes of patients who self-extubate from ventilatory support: a case-control study. Chest 112:1317–1223
Coppolo DP, May JJ (1990) Self-extubations. A 12-month experience. Chest 98:165–169
Vassal T, Anh NG, Gabillet JM, Guidet B, Staikowsky F, Offenstadt G (1993) Prospective evaluation of self-extubations in a medical intensive care unit. Intensive Care Med 19:340–342
Tung A, Tadimeti L, Caruana-Montaldo B, Atkins PM, Mion LC, Palmer RM Slomka J, Mendelson W (2001) The relationship of sedation to deliberate self-extubation. J Clin Anesth 13:24–29
Taggart JA, Lind MA (1994) Evaluating unplanned endotracheal extubations. Dimens Crit Care Nurs 13:114–121
Pesiri AJ (1994) Two-year study of the prevention of unintentional extubation. Crit Care Nurs Q 17:35–39
Chiang AA, Lee KC, Lee JC, Wei CH (1996) Effectiveness of a continuous quality improvement program aiming to reduce unplanned extubation: a prospective study. Intensive Care Med 22:1269–1271
Maguire GP, DeLorenzo LJ, Moggio RA (1994) Unplanned extubation in the intensive care unit: a quality-of-care concern. Crit Care Nurs Q 17:40–47
Little LA, Koenig JC Jr, Newth CJ (1990) Factors affecting accidental extubations in neonatal and pediatric intensive care patients. Crit Care Med 18:163–165
Boulain T (1998) Unplanned extubations in the adult intensive care unit: a prospective multicenter study. Association des Reanimateurs du Centre-Ouest. Am J Respir Crit Care Med 157:1131–1137
Christie JM, Dethlefsen M, Cane RD (1996) Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth 8:289–293
Devlin JW, Fraser GL, Kanji S, Riker RR (2001) Sedation assessment in critically ill adults. Ann Pharmacother 35:1624–1632
Carrasco G (2000) Instruments for monitoring intensive care unit sedation. Crit Care 4:217–225
De Jonghe B, Cook D, Appere-De-Vecchi C, Guyatt G, Meade M, Outin H (2000) Using and understanding sedation scoring systems: a systematic review. Intensive Care Med 26:275–285
Ramsay MA, Savege TM, Simpson BR, Goodwin R (1974) Controlled sedation with alphaxalone-alphadolone. Br Med J 2:656–659
Armstrong RF, Bullen C, Cohen SL, Singer M, Webb AR (1992) Critical care algorithm: sedation, analgesia and paralysis. Clin Intensive Care 3:284–287
Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W, Kollef MH (1999) Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med 27:2609–2615
Brattebo G, Hofoss D, Flaatten H, Muri AK, Gjerde S, Plsek PE (2002) Effect of a scoring system and protocol for sedation on duration of patients’ need for ventilator support in a surgical intensive care unit. Br Med J 324:1386–1389
Esteban A, Frutos F, Tobin MJ, Alia I, Solsona JF, Valverdu I, Fernandez R, Cal MA de la, Benito S, Tomas R (1995) A comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. N Engl J Med 332:345–350
Ely EW, Baker AM, Dunagan DP, Burke HL, Smith AC, Kelly PT, Johnson MM, Browder RW, Bowton DL, Haponik EF (1996) Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med 335:1864–1869
Acknowledgements
The authors gratefully thank P. Lauwers, H. Bobbaers, F. Van de Werf, and H. Delooz of the University Hospitals of Leuven (Belgium) for their participation in this study. S. Fieuws is acknowledged for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Moons, P., Sels, K., De Becker, W. et al. Development of a risk assessment tool for deliberate self-extubation in intensive care patients. Intensive Care Med 30, 1348–1355 (2004). https://doi.org/10.1007/s00134-004-2228-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2228-2