Abstract
Background
While surgery is considered standard of care for early stage (I/II), non-small-cell lung cancer (NSCLC), radiotherapy is a widely accepted alternative for medically unfit patients or those who refuse surgery. International guidelines recommend several treatment options, comprising stereotactic body radiation therapy (SBRT) for small tumors, conventional radiotherapy ≥ 60 Gy for larger sized especially centrally located lesions or continuous hyperfractionated accelerated RT (CHART). This study presents clinical outcome and toxicity for patients treated with a dose-differentiated accelerated schedule using 1.8 Gy bid (DART-bid).
Patients and methods
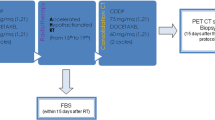
Between April 2002 and December 2010, 54 patients (median age 71 years, median Karnofsky performance score 70 %) were treated for early stage NSCLC. Total doses were applied according to tumor diameter: 73.8 Gy for < 2.5 cm, 79.2 Gy for 2.5–4.5 cm, 84.6 Gy for 4.5–6 cm, 90 Gy for > 6 cm.
Results
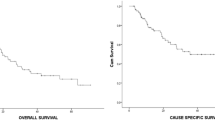
The median follow-up was 28.5 months (range 2–108 months); actuarial local control (LC) at 2 and 3 years was 88 %, while regional control was 100 %. There were 10 patients (19 %) who died of the tumor, and 18 patients (33 %) died due to cardiovascular or pulmonary causes. A total of 11 patients (20 %) died intercurrently without evidence of progression or treatment-related toxicity at the last follow-up, while 15 patients (28 %) are alive. Acute esophagitis ≤ grade 2 occurred in 7 cases, 2 patients developed grade 2 chronic pulmonary fibrosis.
Conclusion
DART-bid yields high LC without significant toxicity. For centrally located and/or large (> 5 cm) early stage tumors, where SBRT is not feasible, this method might serve as radiotherapeutic alternative to present treatment recommendations, with the need of confirmation in larger cohorts.
Zusammenfassung
Hintergrund
Die Standardbehandlung für nichtkleinzellige Bronchialkarzinome (NSCLC) im Stadium I/II ist die Operation, wobei Radiotherapie für Patienten, die nicht operabel sind oder die Operation ablehnen, als Alternative akzeptiert ist. Internationale Leitlinien empfehlen verschiedene Therapieoptionen, darunter Körperstereotaxie für kleine Tumoren, konventionelle Radiotherapie ≥ 60 Gy für größere insbesondere zentral gelegene Tumoren oder eine Behandlung nach dem CHART("continuous hyperfractionated accelerated radiotherapy")-Regime. Diese Studie zeigt klinische Ergebnisse und Toxizität nach akzelerierter Radiotherapie mit 2 × 1,8 Gy täglich (DART-bid).
Patienten und Methoden
Von 04/2002 bis 12/2010 wurden 54 Patienten (medianes Alter 71 Jahre, medianer Karnofsky-Index 70 %) mit NSCLC im Frühstadium behandelt. Die Gesamtdosis wurde nach Tumordurchmesser verordnet: 73,8 Gy (< 2,5 cm), 79,2 Gy (2,5–4 cm), 84,6 Gy (4,5–6 cm), 90 Gy (> 6 cm).
Ergebnisse
Die mediane Nachsorgedauer aller Patienten betrug 28,5 Monate (2–108), die aktuarische Lokalkontrolle (LC) nach 2 und 3 Jahren 88 % und die regionäre Kontrolle 100 %. Tumorbedingt verstarben 10/54 (19 %) Patienten, 18/54 (33 %) an kardiovaskulären oder pulmonalen Erkrankungen. Interkurrent verstarben 11/54 (20 %) Patienten, wobei die Tumorerkrankung zum Zeitpunkt der letzten Nachsorge kontrolliert war und keine therapieassoziierte Toxizität feststellbar war; 15/54 (28 %) Patienten leben noch. Sieben Patienten erlitten eine akute Ösophagitis ≤ Grad 2, 2 eine chronische Lungenfibrose Grad 2.
Schlussfolgerung
DART-bid ermöglicht eine hohe Lokalkontrollrate ohne wesentliche Toxizität. Insbesondere für zentral gelegene und/oder große (> 5 cm) Tumoren, bei denen eine Körperstereotaxie nicht durchführbar ist, könnte diese Methode als mögliche radiotherapeutische Alternative zu den derzeit gültigen Empfehlungen dienen, mit der Notwendigkeit der Validierung in größeren Kohorten.

Similar content being viewed by others
References
Detterbeck FC, Boffa DJ, Tanoue LT (2009) The new lung cancer staging system. Chest 136:260–271
Mauguen A, Le Pechoux C, Saunders MI et al (2012) Hyperfractionated or accelerated radiotherapy in lung cancer: an individual patient data meta-analysis. J Clin Oncol 30:2788–2797
Bogart JA, Hodgson L, Seagren SL et al (2010) Phase I study of accelerated conformal radiotherapy for stage I non-small-cell lung cancer in patients with pulmonary dysfunction: CALGB 39904. J Clin Oncol 28:202–206
Cheung PC, Yeung LT, Basrur V, Ung YC, Balogh J, Danjoux CE (2002) Accelerated hypofractionation for early-stage non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 54:1014–1023
Howington JA, Blum MG, Chang AC, Balekian AA, Murthy SC (2013) Treatment of stage I and II non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143:e278S–313S
Goeckenjan G, Sitter H, Thomas M et al (2011) Prevention, diagnosis, therapy, and follow-up of lung cancer. Interdisciplinary guideline of the German Respiratory Society and the German Cancer Society—abridged version. Pneumologie 65:e51–75
Vansteenkiste J, De Ruysscher D, Eberhardt WE et al (2013) Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24:vi89–98
www.nccn.org. Accessed: 28 Feb. 2014
Wurstbauer K, Deutschmann H, Kopp P et al (2010) Nonresected non-small-cell lung cancer in Stages I through IIIB: accelerated, twice-daily, high-dose radiotherapy—a prospective phase I/II trial with long-term follow-up. Int J Radiat Oncol Biol Phys 77:1345–1351
Wurstbauer K, Deutschmann H, Dagn K et al (2013) DART-bid (Dose-differentiated accelerated radiation therapy, 1.8 Gy twice daily)—a novel approach for non-resected NSCLC: final results of a prospective study, correlating radiation dose to tumor volume. Radiat Oncol 8:49
van Baardwijk A, Tome WA, van Elmpt W et al (2012) Is high-dose stereotactic body radiotherapy (SBRT) for stage I non-small cell lung cancer (NSCLC) overkill? A systematic review. Radiother Oncol 105:145–149
Fowler JF, Tome WA, Fenwick JD, Mehta MP (2004) A challenge to traditional radiation oncology. Int J Radiat Oncol Biol Phys 60:1241–1256
Deutschmann H, Steininger P, Nairz O et al (2008) “Augmented reality” in conventional simulation by projection of 3-D structures into 2-D images: a comparison with virtual methods. Strahlenther Onkol 184:93–99
Essler M, Wantke J, Mayer B et al (2013) Positron-emission tomography CT to identify local recurrence in stage I lung cancer patients 1 year after stereotactic body radiation therapy. Strahlenther Onkol 189:495–501
Solda F, Lodge M, Ashley S, Whitington A, Goldstraw P, Brada M (2013) Stereotactic radiotherapy (SABR) for the treatment of primary non-small cell lung cancer; systematic review and comparison with a surgical cohort. Radiother Oncol 109:1–7
Grills IS, Mangona VS, Welsh R et al (2010) Outcomes after stereotactic lung radiotherapy or wedge resection for stage I non-small-cell lung cancer. J Clin Oncol 28:928–935
Shirvani SM, Jiang J, Chang JY et al (2012) Comparative effectiveness of 5 treatment strategies for early-stage non-small cell lung cancer in the elderly. Int J Radiat Oncol Biol Phys 84:1060–1070
Rowell NP, Williams CJ (2001) Radical radiotherapy for stage I/II non-small cell lung cancer in patients not sufficiently fit for or declining surgery (medically inoperable): a systematic review. Thorax 56:628–638
Baumann M, Herrmann T, Koch R et al (2011) Final results of the randomized phase III CHARTWEL-trial (ARO 97–1) comparing hyperfractionated-accelerated versus conventionally fractionated radiotherapy in non-small cell lung cancer (NSCLC). Radiother Oncol 100:76–85
Saunders M, Dische S, Barrett A, Harvey A, Griffiths G, Palmar M (1999) Continuous, hyperfractionated, accelerated radiotherapy (CHART) versus conventional radiotherapy in non-small cell lung cancer: mature data from the randomised multicentre trial. CHART Steering committee. Radiother Oncol 52:137–148
Saunders M, Dische S, Barrett A, Harvey A, Gibson D, Parmar M (1997) Continuous hyperfractionated accelerated radiotherapy (CHART) versus conventional radiotherapy in non-small-cell lung cancer: a randomised multicentre trial. CHART Steering Committee. Lancet 350:161–165
Maguire PD, Marks LB, Sibley GS et al (2001) 73.6 Gy and beyond: hyperfractionated, accelerated radiotherapy for non-small-cell lung cancer. J Clin Oncol 19:705–711
Sibley GS, Jamieson TA, Marks LB, Anscher MS, Prosnitz LR (1998) Radiotherapy alone for medically inoperable stage I non-small-cell lung cancer: the Duke experience. Int J Radiat Oncol Biol Phys 40:149–154
Jeremic B, Shibamoto Y, Acimovic L, Milisavljevic S (1997) Hyperfractionated radiotherapy alone for clinical stage I nonsmall cell lung cancer. Int J Radiat Oncol Biol Phys 38:521–525
van Baardwijk A, Wanders S, Boersma L et al (2010) Mature results of an individualized radiation dose prescription study based on normal tissue constraints in stages I to III non-small-cell lung cancer. J Clin Oncol 28:1380–1386
Baumann P, Nyman J, Hoyer M et al (2009) Outcome in a prospective phase II trial of medically inoperable stage I non-small-cell lung cancer patients treated with stereotactic body radiotherapy. J Clin Oncol 27:3290–3296
Duncker-Rohr V, Nestle U, Momm F et al (2013) Stereotactic ablative radiotherapy for small lung tumors with a moderate dose. Favorable results and low toxicity. Strahlenther Onkol 189:33–40
Timmerman R, McGarry R, Yiannoutsos C et al (2006) Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J Clin Oncol 24:4833–4839
Soliman H, Cheung P, Yeung L et al (2011) Accelerated hypofractionated radiotherapy for early-stage non-small-cell lung cancer: long-term results. Int J Radiat Oncol Biol Phys 79:459–465
Asai K, Shioyama Y, Nakamura K et al (2012) Radiation-induced rib fractures after hypofractionated stereotactic body radiation therapy: risk factors and dose-volume relationship. Int J Radiat Oncol Biol Phys 84:768–773
Lagerwaard FJ, Verstegen NE, Haasbeek CJ et al (2012) Outcomes of stereotactic ablative radiotherapy in patients with potentially operable stage I non-small cell lung cancer. Int J Radiat Oncol Biol Phys 83:348–353
Dunlap NE, Cai J, Biedermann GB et al (2010) Chest wall volume receiving >30 Gy predicts risk of severe pain and/or rib fracture after lung stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 76:796–801
Mutter RW, Liu F, Abreu A, Yorke E, Jackson A, Rosenzweig KE (2012) Dose-volume parameters predict for the development of chest wall pain after stereotactic body radiation for lung cancer. Int J Radiat Oncol Biol Phys 82:1783–1790
Forquer JA, Fakiris AJ, Timmerman RD et al (2009) Brachial plexopathy from stereotactic body radiotherapy in early-stage NSCLC: dose-limiting toxicity in apical tumor sites. Radiother Oncol 93:408–413
Ong CL, Palma D, Verbakel WF, Slotman BJ, Senan S (2010) Treatment of large stage I-II lung tumors using stereotactic body radiotherapy (SBRT): planning considerations and early toxicity. Radiother Oncol 97:431–436
Palma D, Visser O, Lagerwaard FJ, Belderbos J, Slotman B, Senan S (2011) Treatment of stage I NSCLC in elderly patients: a population-based matched-pair comparison of stereotactic radiotherapy versus surgery. Radiother Oncol 101:240–244
Senthi S, Haasbeek CJ, Slotman BJ, Senan S (2013) Outcomes of stereotactic ablative radiotherapy for central lung tumours: a systematic review. Radiother Oncol 106:276–282
Jeremic B, Classen J, Bamberg M (2002) Radiotherapy alone in technically operable, medically inoperable, early-stage (I/II) non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 54:119–130
Jeremic B (2007) Low incidence of isolated nodal failures after involved-field radiation therapy for non small-cell lung cancer: blinded by the light? J Clin Oncol 25:5543–5545
Rosenzweig KE, Sura S, Jackson A, Yorke E (2007) Involved-field radiation therapy for inoperable non small-cell lung cancer. J Clin Oncol 25:5557–5561
Compliance with ethical guidelines
Conflict of interest
F. Zehentmayr, K. Wurstbauer, H. Deutschmann, C. Fussl, P. Kopp, K. Dagn, G. Fastner, P. Porsch, M. Studnicka, and F. Sedlmayer state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zehentmayr, F., Wurstbauer, K., Deutschmann, H. et al. DART-bid: dose-differentiated accelerated radiation therapy, 1.8 Gy twice daily. Strahlenther Onkol 191, 256–263 (2015). https://doi.org/10.1007/s00066-014-0754-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0754-6