Abstract
Purpose
To evaluate inter- and intrafraction organ motion with an ultrasound-based prostate localization system (BAT®) for patients treated with intensity-modulated radiotherapy for prostate cancer.
Patients and Methods
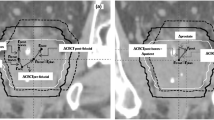
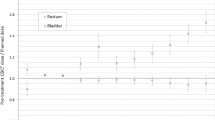
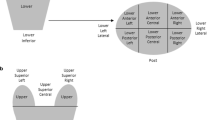
After set-up to external skin marks, 260/219 ultrasound-based alignments were performed before/after irradiation in 32 consecutive patients. Image quality was classified as good, satisfactory or poor. Patient- and imaging-related parameters were analyzed to identify predictors for poor image quality. Shifts in relation to the treatment planning computed tomography (CT) were recorded before/after irradiation in the superior-inferior (SI), anterior-posterior (AP) and right-left (RL) directions to determine inter-/intrafraction prostate motion.
Results
The thickness of tissue anterior to the bladder and bladder volume during the ultrasound localization as well as an inferior prostate position relative to public symphysis (determined in treatment planning CT) were found to be independent predictors of a poor image quality. Interfraction shifts (mean ± standard deviation: −0.2 ± 4.8 [SI], 2.4 ± 6.6 [AP] and 1.9 ± 4.6 [RL]) varied much stronger than intrafraction shifts (0.0 ± 2.0 [SI], 0.6 ± 2.2 [AP] and 0.2 ± 1.9 [RL]). A larger pressure of the ultrasound probe (determined as a larger reduction of the distance abdominal skin to prostate between the planning CT and the ultrasound) was applied in case of poor image quality, associated with larger systematic posterior prostate displacements.
Conclusion
Intrafraction prostate shifts are considerably smaller in comparison to interfraction shifts. Bladder filling and a small pressure on the ultrasound probe are crucial to achieve an adequate image quality without systematic prostate displacements.
Zusammenfassung
Ziel
Bestimmung der inter- und intrafraktionellen Organbewegung mit einem ultraschallbasierten Lokalisationssystem der Prostata (BAT®) bei mit intensitätsmodulierter Radiotherapie behandelten Patienten mit Prostatakarzinom.
Patienten und Methodik
Nach Lagerung entsprechend der externen Hautmarkierung wurden 260/219 ultraschallbasierte Positionierungen vor/nach Bestrahlung bei 32 konsekutiven Patienten durchgeführt. Die Bildqualität wurde als gut, zufriedenstellend oder schlecht bewertet. Patienten- und bildgebungsabhängige Parameter wurden zur Identifikation von Prädiktoren für schlechte Bildqualität analysiert. Verschiebungen im Verhältnis zur Bestrahlungsplanungs-Computertomographie(-CT) wurden in der superior-inferioren (SI), anterior-posterioren (AP) und Rechts-links-(RL-)Achse vor/nach Bestrahlung dokumentiert, um inter-/intrafraktionelle Prostatabewegungen zu bestimmen.
Ergebnisse
Sowohl die Dicke des Gewebes ventral der Blase und das Blasenvolumen während der Ultraschalllokalisation als auch eine inferiore Prostatalage relativ zur Symphyse (bestimmt im Bestrahlungsplanungs-CT) fanden sich als unabhängige Prädiktoren einer schlechten Bildqualität. Interfraktionelle Verschiebungen (Mittelwert ± Standardabweichung: −0,2 ± 4,8 [SI], 2,4 ± 6,6 [AP] und 1,9 ± 4,6 [RL]) variierten viel stärker als intrafraktionelle Verschiebungen (0,0 ± 2,0 [SI], 0,6 ± 2,2 [AP] und 0,2 ± 1,9 [RL]). Ein stärkerer Druck auf die Ultraschallsonde (als eine größere Reduktion des Abstandes Bauchhaut zu Prostata zwischen dem Planungs-CT und dem Ultraschall bestimmt) wurde vor allem bei schlechter Bildqualität ausgeübt, verbunden mit größeren systematischen dorsalen Prostataverschiebungen.
Schlussfolgerung
Intrafraktionelle Prostataverschiebungen sind deutlich geringer als interfraktionelle Verschiebungen. Blasenfüllung und ein geringer Druck auf die Ultraschallsonde sind zum Erzielen einer adäquaten Bildqualität ohne systematische Prostataverschiebungen entscheidend.
Similar content being viewed by others
References
Akimoto T, Muramatsu H, Takahashi M, et al. Rectal bleeding after hypofractionated radiotherapy for prostate cancer: correlation between clinical and dosimetric parameters and the incidence of grade 2 or worse rectal bleeding. Int J Radiat Oncol Biol Phys 2004;60:1033–1039.
Boda-Heggemann J, Köhler FM, Küpper B, et al. Accuracy of ultrasound-based (BAT) prostate-repositioning: a three-dimensional on-line fiducial-based assessment with cone-beam computed tomography. Int J Radiat Oncol Biol Phys 2008;70:1247–1255.
Cheung P, Sixel K, Morton G, et al. Individualized planning target volumes for intrafraction motion during hypofractionated intensity-modulated radiotherapy boost for prostate cancer. Int J Radiat Oncol Biol Phys 2005;62:418–425.
Cheung R, Tucker SL, Ye JS, et al. Characterization of rectal normal tissue complication probability after high-dose external beam radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 2004;58:1513–1519.
de Crevoisier, Tucker SL, Dong L, et al. Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy. Int J Radiat Oncol Biol Phys 2005;62:965–973.
Dobler B, Mai S, Ross C, et al. Evaluation of possible displacement induced by pressure applied during transabdominal ultrasound image acuisition. Strahlenther Onkol 2006;182:240–246.
Elsayed H, Bolling T, Moustakis C, et al. Organ movements and dose exposures in teletherapy of prostate cancer using a rectal balloon. Strahlenther Onkol 2007;183:617–624.
Guckenberger M, Flentje M. Intensity-modulated radiotherapy (IMRT) of localized prostate cancer: a review and future perspectives. Strahlenther Onkol 2007;183:57–62.
van Herk M. Errors and margins in radiotherapy. Semin Radiat Oncol 2004;1:52–64.
Jackson A, Skwarchuk MW, Zelefsky MJ, et al. Late rectal bleeding after conformal radiotherapy of prostate cancer. II. Volume effects and dose-volume histograms. Int J Radiat Oncol Biol Phys 2001;49:685–698.
Jereczek-Fossa BA, Cattani F, Garibaldi C, et al. Transabdominal ultrasonography, computed tomography and electronic portal imaging for 3-dimensional conformal radiotherapy for prostate cancer. Strahlenther Onkol 2007;183:610–616.
McNair HA, Hansen VN, Parker CC, et al. A comparison of the use of bony anatomy and internal markers for offline verification and an evaluation of the potential benefit of online and offline verification protocols for prostate radiotherapy. Int J Radiat Oncol Biol Phys 2008;71:41–50.
Müller AC, Ganswindt U, Bamberg M, et al. Risk of second malignancies after prostate irradiation? Strahlenther Onkol 2007;183:605–609.
O’Doherty UM, McNair HA, Norman AR, et al. Variability of bladder filling in patients receiving radical radiotherapy to the prostate. Radiother Oncol 2006;79:335–340.
Pinkawa M, Asadpour B, Gagel B, et al. Prostate position variability and dose-volume histograms in radiotherapy for prostate cancer with full and empty bladder. Int J Radiat Oncol Biol Phys 2006;64:856–861.
Pinkawa M, Asadpour B, Siluschek J, et al. Bladder extension variability during pelvic external beam radiotherapy with a full or empty bladder. Radiother Oncol 2007;83:163–167.
Pinkawa M, Fischedick K, Asadpour B. Health-related quality of life after adjuvant and salvage postoperative radiotherapy for prostate cancer — a prospective analysis. Radiother Oncol 2008;88:135–139.
Pinkawa M, Fischedick K, Asadpour B, et al. Low-grade toxicity after conformal radiation therapy for prostate cancer — impact of bladder volume. Int J Radiat Oncol Biol Phys 2006;64:835–841.
Pinkawa M, Fischedick K, Asadpour B, et al. Toxicity profile with a large prostate volume after external beam radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2008;70:83–89.
Pinkawa M, Siluschek J, Gagel B, et al. Influence of the initial rectal distension on posterior margins in primary and postoperative radiotherapy for prostate cancer. Radiother Oncol 2006;81:284–290.
Pinkawa M, Siluschek J, Gagel B, et al. Postoperative radiotherapy for prostate cancer: evaluation of target motion and treatment techniques (intensity-modulated versus conformal radiotherapy). Strahlenther Onkol 2007;183:23–29.
Serago CF, Chungbin SJ, Buskirk SJ, et al. Initial experience with ultrasound localization for positioning prostate cancer patients for external beam radiotherapy. Int J Radiat Oncol Biol Phys 2002;53:1130–1138.
Vordermark D, Marold D, Wirth S, et al. Patterns of care in the radiotherapy of prostate cancer in Northern Bavaria 1998–2000. Strahlenther Onkol 2007;183:314–320.
Weiss W, Horninger W, Forthuber BC, et al. Single-institution results of primary external-beam radiation for the treatment of t1–t3 prostate cancer. Strahlenther Onkol 2007;183:321–326.
Wertz H, Boda-Heggemann J, Walter C, et al. Image-guided in vivo dosimetry for quality assurance of IMRT treatment of prostate cancer. Int J Radiat Oncol Biol Phys 2007;67:288–295.
Wertz H, Lohr F, Dobler B, et al. Dosimetric impact of image-guided translational isocenter correction for 3-D conformal radiotherapy of the prostate. Strahlenther Onkol 2007;183:203–210.
Wiezorek T, Voigt A, Metzger N, et al. Experimental determination of peripheral doses for different IMRT techniques delivered by a Siemens lineas accelerator. Strahlenther Onkol 2008;184:73–79.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinkawa, M., Pursch-Lee, M., Asadpour, B. et al. Image-guided radiotherapy for prostate cancer. Strahlenther Onkol 184, 679–685 (2008). https://doi.org/10.1007/s00066-008-1902-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-008-1902-7