Abstract
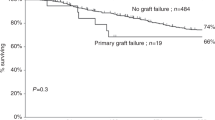
Premise: Since March 1993, 133 patients with high-risk acute leukemia (66 AML, 67 ALL) have received a megadose of T-cell depleted hematopoietic stem cells. The 1993–95 conditioning protocol included TBI, thiotepa, ATG and CY for 36 patients who received an inoculum made up of lectin-separated bone marrow and PBPCs. After 1995, to minimise the extra-hematological toxicity of the conditioning and eliminate GvHD, we substituted fludarabine for CY in the conditioning and PBPCs were depleted of T-cells by a positive selection of the CD34+ cells using CellPro (n=44 patients) or, since January 1999, CliniMacs (n=53 patients). A later modification to the protocol in January 1999 was the suspension of post transplant G-CSF.Work in Progress: We report here the results in the last 53 acute leukemia patients all of whom were transplanted under our modified protocol. Ages ranged from 9 to 62 years with a median of 38 years for the 33 patients with AML and 23 for the 20 with ALL. All were at high risk because 25 were actually in relapse at transplant, 16 were in second or later CR and even the 12 patients in CR1 were at high risk because of the unfavourable prognostic features. Overall 52/53 patients (98%) engrafted. The TBI-Fludarabine-based conditioning was well tolerated even in the 14 patients between 45 and 62 years of age. There was no veno-occlusive disease of the liver and the incidence of severe mucositis was low. Even though no post-transplant immunosuppressive therapy was given, acute GvHD grade≥II occurred in only 4 cases and only one progressed to chronic GvHD. Overall, 16 patients (30%) have died of non-leukemic causes. Relapses occurred mainly in patients who were already in relapse at transplant (12/25). Only 3 of the 28 who were in any CR at transplant have so far relapsed. As our group has already shown, donor-vs-recipient NK cell alloreactivity exerts a specific graft-vs-AML effect in the absence of GvHD. In fact, leukemia relapse was largely controlled in AML recipients whose donor was NK alloreactive, with only 2 out of 16 relapsing. To date, 13 of 18 AML (72%) and 5 of 10 ALL (50%) who were in any CR at transplant, survival for patients transplanted in CR is 60% in the 18 AML patients and 38% in the 10 ALL. The probability of EFS was significantly better in the 16 AML patients whose transplant included donor vs recipient NK cell alloreactivity than in those whose transplant did not (70% vs 7%). In conclusion, given our current results, the most suitable candidate for the full haplotype mismatched transplant should be in early stage disease and selection of an NK alloreactive donor is recommended.
Similar content being viewed by others
References
Hansen JA, Petersdorf E, Martin PJ, et al. Hematopoietic stem cell transplants from unrelated donors.Immunol Rev. 1997; 157:141–151.
Beatty PG, Mori M, Milford E. Impact of racial genetic polymorphism on the probability of finding an HLA-matched donor.Transplantation. 1995;60:778–783.
Reisner Y, Kapoor N, Kirkpatrick D, et al. Transplantation for severe combined immunodeficiency with HLA-A, B, D, DR incompatible parental marrow cells fractionated by soybean agglutinin and sheep red blood cells.Blood 1983;61:341–348.
Anasetti C, Beatty PG, Storb R, et al. Effect of HLA incompatibility on graft-versus-host disease, relapse, and survival after marrow transplantation for patients with leukemia or lymphoma.Hum Immunol. 1990;29:79–91.
Kernan NA, Flomemberg N, Dupont B, et al. Graft rejection in recipients of T cell depleted HLA-nonidentical marrow transplants for leukemia: identification of host derived antidonor allocytotoxic T lymphocytes.Transplantation. 1987;43:482–487
Bachar-Lusting E, Rachamim N, Li HW, Lan F, Reisner Y. Megadose of T cell-depleted bone marrow overcomes MHC barriers in sublethally irradiated mice.Nat Med. 1995;1:1268–1273
Rachamin N, Gan J, Segall R, et al. Tolerance induction by “megadose” hematopoietic transplants: donor-type human CD34 stem cells induce potent specific reduction of host anti-donor cytotoxic T lymphocyte precursors in mixed lymphocyte culture.Transplantation 1998;65:1386–1393.
Aversa F, Tabilio A, Terenzi A, et al. Successful engraftment of T-cell-depleted haploidentical “three-loci” incompatible transplants in leukemia patients by addition of recombinant human granulocyte colony-stimulating factor-mobilized peripheral blood progenitor cells to bone marrow inoculum.Blood. 1994;84:3948–3955.
Terenzi A, Aristei C, Aversa F, et al. Efficacy of fludarabine as an immunosuppressor for bone marrow transplantation conditioning: Preliminary results.Transplant Proc. 1996;28:3101.
Aversa F, Tabilio A, Velardi A, et al. Treatment of high risk acute leukemia with T-cell-depleted stem cells from related donors with one fully mismatched HLA haplotype.N Engl J Med. 1998;339:1186–1193.
Pan L, Delmonte J Jr, Jalonen CK, Ferrara JL. Pretreatment of donor mice with granulocyte colony-stimulating factor polarizes donor T lymphocytes toward type-2 cytokine production and reduces severity of experimental graft-versus-host disease.Blood. 1995;86:4422–4429.
Volpi I, Perruccio K, Tosti A, et al. Post-grafting granulocyte colony-stimulating factor administration impairs functional immune recovery in recipients of HLA haplotype-mismatched hematopoietic transplants.Blood. 2001;97:2514–2521.
Ruggeri L, Capanni M, Casucci M, et al. Role of natural killer cell alloreactivity in HLA-mismatched hematopoietic stem cell transplantation.Blood. 1999;94:333–339.
Ruggeri L, Capanni M, Urbani E, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants.Science 2002;295:2097–2100.
Author information
Authors and Affiliations
About this article
Cite this article
Aversa, F., Terenzi, A., Felicini, R. et al. Haploidentical stem cell transplantation for acute leukemia. Int J Hematol 76 (Suppl 1), 165–168 (2002). https://doi.org/10.1007/BF03165238
Issue Date:
DOI: https://doi.org/10.1007/BF03165238